Imaging plays an important role in the diagnosis and treatment of brain abscess, pyogenic infection, and encephalitis. The role of CT and MRI in the diagnosis and management of pyogenic brain abscess and its complications is reviewed. The imaging appearances of several common and select uncommon infectious encephalitides are reviewed. Common causes of encephalitis in immunocompromised patients, and their imaging appearances, are also discussed. When combined with CSF, serologic studies and patient history, imaging findings can suggest the cause of encephalitis.
- •
The most common identified sources of brain abscess include: otomastoiditis, sinusitis, odontogenic abscess, hematogenous dissemination from a distant source and neurosurgical complication.
- •
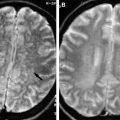
MRI is sensitive for the detection of brain abscess. Restricted diffusion within a centrally T2 hyperintense ring enhancing mass is characteristic but not pathognomonic of pyogenic brain abscess.
- •
MRI can demonstrate the complications from brain abscess including intracranial herniation, hydrocephalus, meningitis, subdural or epidural empyema, venous sinus thrombosis and ventriculitis.
- •
Imaging is critical to the rapid diagnosis of brain abscess, provides guidance for stereotactic localization and is useful for monitoring response following treatment.
- •
Infectious encephalitis is usually viral in etiology and should be considered in patients complaining of fever and headache with altered level of consciousness or evidence of cerebral dysfunction.
- •
The MRI features of encephalitis are highly variable according to the offending organism and patient age.
- •
HSV encephalitis is associated with high mortality and in adults typically causes asymmetric bilateral FLAIR/T2WI hyperintensity in the medial temporal lobes, insular cortex and posterior-inferior frontal lobes with relative sparing of the basal ganglia.
Introduction
Cerebritis is an area of poorly defined acute inflammation in the brain with increased permeability of the local blood vessels, but without neovascularity or angiogenesis. Cerebritis can result from a variety of etiological factors, including pyogenic infection, and if left untreated in this setting leads to pyogenic brain abscess formation. A pyogenic abscess is a focal area of parenchymal infection that contains a central collection of pus surrounded by a vascularized collagenous capsule. Before the late 1800s brain abscess was typically fatal and only discovered on postmortem examination. In 1893, Sir William Macewen published the monograph Pyogenic Infective Diseases of the Brain and Spinal Cord , which described the successful surgical treatment of 18 of 25 reported intraparenchymal brain abscesses. Macewen stressed the importance of aseptic surgery, cerebral localization, and early diagnosis as important factors essential to the successful surgical treatment of brain abscess. After the addition of antibiotic treatment in the early 1940s, mortality from brain abscesses decreased over the next 2 decades but remained high. A multitude of imaging modalities including ventriculography, angiography, and thorotrast administration had a positive impact on the treatment of brain abscess by providing a means to sequentially image the abscess cavity. Since the mid 1970s, mortality from brain abscess has decreased from 30% to 40% to 5% to 20%, with the higher rates reported in developing nations. This reduction in mortality has largely been attributed to (1) the advent of commercially available computed tomography (CT) in 1974, and (2) improved targeted antibiotic therapy due to advances in bacteriologic techniques and new antimicrobial agents. CT allows for rapid diagnosis and localization, stereotactic aspiration, and accurate serial postoperative evaluation.
Encephalitis is a diffuse infection or inflammatory process of the brain itself with clinical evidence of brain dysfunction. Infectious encephalitis is typically viral in origin. The diagnosis of viral encephalitis should be strongly considered in patients presenting with febrile disease accompanied by headache, altered level of consciousness, and evidence of cerebral dysfunction. Imaging plays a role in the diagnosis of encephalitis when combined with the medical history, physical examination, serologic studies, and cerebrospinal fluid (CSF) analysis. In addition, there are multiple nonviral causes of infectious encephalitis including bacterial, fungal, parasitic, and rickettsial origins. The imaging appearances of several common and select uncommon infectious encephalitides along with causes of encephalitis in the pediatric patient population are reviewed in this article. Common causes of encephalitis in immunocompromised patients, and their imaging appearances, are also discussed in this article.
Pyogenic Infection
Pathophysiology
Brain abscess is often categorized by the source of infection, which influences the location of the abscess and the offending organism. The most common identified causes of brain abscess include direct spread from local infections, hematogenous dissemination from a distant source, trauma, and neurosurgical complication. Up to 30% of brain abscesses are reported as cryptogenic. Otomastoiditis, sinusitis, and odontogenic abscess are the primary sources of direct spread, which occurs through involvement of bone or via transmission of bacteria to the brain through the valveless emissary veins. Otomastoiditis causes abscess formation in the adjacent temporal lobe and cerebellum ( Figs. 1 and 2 ). Frontal and ethmoid sinusitis and odontogenic infection are frequently associated with formation of frontal lobe abscess.
Abscesses secondary to hematogenous seeding from a distant source are more typically multiple, near the gray-white junction, and usually in the distribution of the middle cerebral artery. Sources of hematogenous dissemination are variable. Identifying the source of infection is a crucial factor for adequate treatment to prevent recurrent disease. In children, there should be a high index of suspicion for congenital cyanotic heart disease. Examples of other sources include pulmonary abscess, pulmonary arteriovenous malformation (AVM), bacterial endocarditis, and intra-abdominal infections. Dental abscess can result in bacteremia with hematogenous dissemination or local thrombophlebitis.
The epidemiologic trends of brain abscess are changing. Brain abscess is uniformly more common among males than females for unknown reasons, and most commonly occurs during the first 4 decades of life, although all age groups may be affected. Aggressive medical and surgical management of otitis media has led to a decrease in otogenic-related brain abscess in developed countries, although it remains the principal source of brain abscess in developing countries such as India and China. Similarly, there are reports of decreased incidence of brain abscess secondary to congenital cyanotic heart disease in developed countries, likely attributable to earlier and improved surgical repair. Brain abscess secondary to trauma and neurosurgery has increased. The rising incidence of postsurgical abscess has largely been attributed to the increased volume of neurosurgeries performed ( Fig. 3 ). Additional predisposing factors include diabetes mellitus, alcoholism, intravenous drug abuse, pulmonary AVM, and immunosuppression.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree