Fig. 14.1
Biomechanics of the golf swing. Address position (a), takeaway (b), backswing-1 (c), backswing-2 (d), downswing (e), acceleration (f), follow-through-1 (g), follow-through-2 (h)
The latissimus dorsi and the pectoralis major are the most active during a golf swing with the former demonstrating maximal force during the downswing and acceleration and the latter during the acceleration and follow-through phases (Kim et al. 2004). Of the rotator cuff tendons, the subscapularis is the most active in each shoulder throughout the entire swing, while the supraspinatus and infraspinatus muscles of the lead shoulder (left shoulder in a right-handed golfer) demonstrate only low-level activity and serve instead to stabilize the glenohumeral joint. The glenoid fossa and its position, labrum, capsule, glenohumeral ligaments, and negative intra-articular pressure serve as further stabilizing structures (Armfield et al. 2003).
Elsewhere around the shoulder girdle, the scapular muscles function with the trapezius muscle to retract the scapula. The scapula is the most active during the downswing and acceleration phases of the lead arm and during takeaway in the trailing arm (right arm in a right-handed golfer). The serratus anterior muscle protracts the trailing arm scapula during downswing, acceleration, and follow-through. The rhomboid and levator scapulae muscles retract and elevate the scapula of the lead arm during the downswing and acceleration phases and protract and stabilize the trailing arm during the downswing.
Motions at the wrist include flexion, extension, and radial and ulnar deviation with pronation and supination of the forearms. The impact on the wrist is substantial.
Within the lower limb, the extensor and abductors of the trailing hip and the adductor magnus of the lead hip initiate pelvic rotation during the downswing with the hamstrings of the lead leg maintaining a flexed knee during pelvic rotation.
14.2.2 Racquet Sports
The literature on the biomechanics of the tennis swing is extensive, but this is not so true of the other racquet sports. Nonetheless, because aspects of the tennis swing are similar to the swings of other racquet sports, the information in the literature can be extrapolated to the other sports. There are 3 basic strokes: (1) overhead or serve, (2) forehand, and (3) backhand.
Forehand and backhand ground strokes are characterized by 3 stages: racquet preparation, acceleration, and follow-through (Marx et al. 2001). Muscle activation in the serve and forehand is greatest for the subscapularis, pectoralis major, and serratus anterior. The backhand involves the middle deltoid, supraspinatus, and infraspinatus.
Wrist extensor activity is predominant in all strokes although it should be noted that wrist extensors do not show increased activity with a single-handed backhand compared with a double-handed backhand. For a fuller description of tennis biomechanics, see Chap. 19.
14.3 Types of Injuries
The prevalence of golf injuries ranges from 25 to 62 %. Players over 50 years or with a low handicap (Andresen et al. 1999; Armfield et al. 2003; Bancroft et al. 2007; Blum et al. 2006; Burkhart et al. 2003; Bylak and Hutchison 1998; Cabrera and McCue 1986; Conklin and White 1960; Connell et al. 2001) have a higher prevalence (Theriault and Lachance 1998).
Injuries originate from overuse or trauma and primarily affect the elbow, wrist, shoulder, and the dorsolumbar sites. In the amateur golfer, the most common sites of injury are the thoracolumbar spine (27 %) and elbow (26 %); in the professional players, the wrist (27 %) predominates (McHardy et al. 2007; Theriault and Lachance 1998). The left wrist is injured more frequently (in right-handed golfers) followed by the left hand with most injuries related to the golf swing (Table 14.1) (McHardy et al. 2007).
Table 14.1
Injury incidence in male golfers
Injury incidence | Professional golfer | Amateur golfer |
|---|---|---|
Wrist | 27 % | 16 % |
Elbow | 7 % | 26 % |
Shoulder | 9 % | 8 % |
Thoracolumbar spine | 23 % | 27 % |
Patterns of injury differ between the professional and the amateur golfer, mainly due to swing mechanics and the increased number of repetitions. The most common mechanism of injury in the professional seems to be excessive practice as the swing is more consistent, and in the amateur, the cause is poor swing mechanics (Table 14.2).
Table 14.2
Potential causes of injury
In racquet sports, the most common types of injury are due to overuse and include muscle and ligament injury such as rotator cuff disease and epicondylitis. In badminton Achilles tendon injuries are very common, with one study reporting 92 % of all acute badminton injuries involving the lower extremities and 34.6 % Achilles tendon ruptures (Fahlstrom et al. 1998).
In both sports, injury patterns differ with equipment changes such as length of the club or racquet and the player’s grip.
14.4 Specific Sites of Injury and Imaging Findings
14.4.1 Shoulder
Shoulder injuries can be broadly divided into impingement and glenohumeral instability. This is generalizing matters, as the terms “instability” and “impingement” constitute spectrums of disorders with multiple classification and subclassifications with complex relationships and pathomechanics. Impingement is generally divided into 2 groups: external (or extrinsic) and internal (intrinsic) though when the term is used in isolation, it generally implies external impingement.
Several pathologic mechanisms have been described particularly in overhead and throwing athletes, and as the shoulder is the most commonly injured joint in tennis, injuries specific to tennis are discussed in Chap. 19.
14.4.1.1 Rotator Cuff Disease and Primary (Extrinsic) Impingement
Impingement is a clinical condition in which the subacromial soft tissues (bursa, biceps, and supraspinatus tendons) are compressed between the humeral head and the coracoacromial arch. Rotator cuff degeneration and tears can be a combination of intrinsic factors such as repetitive action, repetitive incidence trauma, and poor technique.
Primary impingement, in which there is impingement of the supraspinatus tendon on the coracoacromial arch, is fairly uncommon in young (athletic) individuals, but much more prevalent in older golfers (Tuite 2003).
In athletes the most frequent locations of rotator cuff tears are the anterior half of the supraspinatus tendon at 0.5–1 cm from the insertion, posterosuperior tears, and the undersurface area of the cuff attachment to the humeral head. The young athletic cuff is resistant to extensive tearing, and partial-thickness and interstitial partial tears are commonly encountered.
Ultrasound or MRI can be used to evaluate rotator cuff disease and cuff-related abnormalities. Ultrasound has the advantage of dynamic imaging, and it can be used in image-guided interventions.
On MRI, tendinosis is seen as intermediate- to high-signal intensity on T2-weighted images, frequently with mild to moderate thickening of the tendon. Ultrasound may demonstrate an enlarged, heterogeneous, or hypoechoic tendon. A tear in the tendon will appear as a fluid- or synovial-filled defect on ultrasound and as a hyperintense lesion within the tendon on T2-weighted images. Full-thickness tears extend across both the bursal and articular surfaces of the tendon; partial tears involve only one surface (Fig. 14.2).
Fig. 14.2
Rotator cuff tear. (a) Short-axis ultrasound image demonstrates full-thickness tear (arrows) of the anterior fibers of the supraspinatus tendon (S). The biceps tendon is demonstrated medially (B). (b) Coronal oblique STIR MRI of the shoulder shows partial-thickness articular surface tear (arrows) of the supraspinatus tendon. Note the intact bursal surface tendon fibers (*) outlined by subacromial bursal fluid (arrowheads). H humerus
Subacromial-subdeltoid bursal disease is more often depicted as thickening of the synovial lining rather than large quantities of bursal fluid (Fig. 14.3). The most common location is over the supraspinatus tendon where the bursa abuts the coracoacromial ligament, and dynamic shoulder assessment using ultrasound can be useful to detect a minimally enlarged bursa with arm movement. However, it should be appreciated that the ultrasound can be normal in patients with symptomatic bursal disease, highlighting a role for guided diagnostic injection.
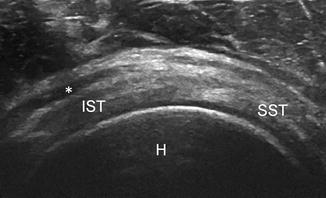
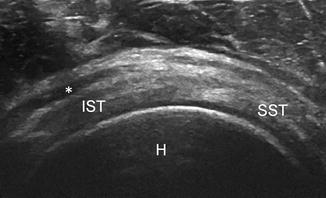
Fig. 14.3
Subacromial bursal thickening. Axial ultrasound image demonstrates thickening of the subacromial bursa (*) overlying the supraspinatus (SST) and infraspinatus tendons (IST). H humeral head
14.4.1.2 Internal Impingement Syndromes
A variety of internal impingement syndromes have been described, including posterosuperior, anterosuperior, and the anterior impingement syndromes. Although most commonly reported in baseball pitchers, posterosuperior impingement can also occur during other activities such as the golf swing or the overhead serve (Drakos et al. 2009).
There are many proposed pathomechanics for this syndrome. Golfers particularly encounter a combination of anterior capsular laxity and posterior capsular contraction. The mechanism behind this is similar to the development of glenohumeral internal rotation deficit as described by Burkhart et al. in the throwing athlete, where there is decreased internal rotation of the shoulder with the arm in abduction (Burkhart et al. 2003). In golfers, this is thought to be related to the follow-through and can lead to an abnormal range of movements and secondary impingement.
MRI features include irregularity and thickening of the posterior limb of the inferior glenohumeral ligament, microfractures/bone marrow changes of the posterosuperior glenoid and greater tuberosity of the humerus, and tears of the posterior superior labrum (Fig. 14.4a) (Giaroli et al. 2005). MRI arthrography has been used to demonstrate these lesions and in particular the use of the ABER (abduction external rotation) position. It is at this position that the supraspinatus tendon may be seen to impose between the posterosuperior glenoid rim and the greater tuberosity of the humerus, though repeated torsion of the tendon during repetitive action is thought to be more important. The supraspinatus lesion usually involves the posterior part of the tendon, in the junctional area between the supraspinatus and infraspinatus, on its joint surface, in contrast to subacromial impingement (Fig. 14.4b) (Woertler and Waldt 2006).
Fig. 14.4
Posterosuperior shoulder impingement. (a) T1-weighted MR arthrogram in abduction and external rotation (ABER) position demonstrates cortical irregularity at the greater tuberosity (arrow) of the humeral head (H) with blunting of the posterosuperior labrum (arrowhead) of the glenoid (G). (b) Coronal oblique fat-suppressed T1-weighted MR arthrogram shows partial articular surface tear of the posterior supraspinatus (arrows) with cortical irregularity at the adjacent posterosuperior humeral head (arrowhead)
There is substantial overlap with the overhead throwing athlete, particularly in glenohumeral internal rotation deficit where thickening of the inferior capsule (posterior limb of the inferior glenohumeral ligament), partial or complete rotator cuff tears, and SLAP II lesions (thought to be a consequence of the “peel back” mechanism) can be encountered at MRI (Fig. 14.5).
Fig. 14.5
SLAP lesions. (a) SLAP type II lesion: coronal oblique fat-suppressed T1-weighted MR arthrogram shows superior extension of contrast media into the superior labrum and biceps anchor (arrow). (b) SLAP type III lesion: coronal oblique T1-weighted MR arthrogram shows a bucket-handle tear of the superior labrum (white arrow) with preserved biceps anchor (black arrow)
14.4.1.3 Acromioclavicular Osteoarthritis
Chronic repetitive loading of the acromioclavicular joint leading to osteoarthritis is typically seen in the lead shoulder in golfers. It is at the top of the back swing and at the end of the follow-through that the maximal force is applied across the joint. The chronic repetitive nature of this motion leads to excessive loading of the joint (Mallon and Colosimo 1995), resulting in chronic ligament injury, cartilage injury, and secondary osteoarthritis.
Osteoarthritis can be depicted on radiographs and on MRI. One should be cautious, however, in attributing pain to osteoarthritis, as the prevalence of osteoarthritis on MRI of asymptomatic individuals has been reported to be as high as 48 % (Needell et al. 1996).
14.4.2 Elbow
14.4.2.1 Common Extensor and Flexor Tendon Disease
Traditionally medial epicondylitis has been termed “golfer’s elbow” and lateral epicondylitis “tennis elbow.” These are misnomers as both varieties occur with equal frequency in the golfer and are the most common abnormality of the elbow (McCarroll 1996). Injury to the common flexor or extensor origin can be caused by repetitive strain, typically due to improper technique, or as the result of acute trauma injury such as striking a club or racquet against a fixed object. Deceleration during the downswing and impact phases strains the medial compartment but also causes forceful contractions at the medial and lateral lower arm musculature. This leads to strain on both the lateral and medial compartments and explains the equal frequency of both medial and lateral epicondylitis in golfers.
The term epicondylitis is misleading however since these are entities of misuse tendinosis and partial tearing of the common flexor and extensor origin (medial and lateral epicondylitis, respectively) caused by repetitive traction on the osteotendinous attachment. The term “epicondylitis” persists in common usage, although common flexor or extensor tendinopathy are better designations for this disorder.
Common extensor tendinopathy predominately involves the extensor carpi radialis brevis tendon. There is also variable involvement of the extensor digitorum communis, extensor carpi radialis longus, and extensor carpi ulnaris tendons (Hume et al. 2006). Common flexor tendinopathy involves the pronator teres and flexor carpi radialis tendons; less common sites include the flexor carpi ulnaris, palmaris longus, and flexor sublimis origins (Nirschl 1988).
Ultrasound remains the imaging modality of choice and offers a quick and focused examination of both areas. The main ultrasound findings of tendinosis include pre-insertional hypoechoic swelling of the tendon with focal or diffuse areas of decreased reflectivity in the tendon substance, loss of the normal fibrillary pattern, fluid adjacent to the common tendon, and ill-defined tendon margins (Connell et al. 2001) (Fig. 14.6a). In high-grade tendinosis, striking hypervascularity of the intratendinous hypoechoic areas can be seen on Doppler interrogation (Fig. 14.6b).
Fig. 14.6
Lateral epicondylitis. (a) Sagittal ultrasound image of the common extensor origin of the elbow joint shows the common extensor tendon (E) is enlarged and hypoechoic at its origin (CEO), affecting both the superficial and deep fibers. (b) Power Doppler signal is demonstrated within the enlarged and thickened common extensor tendon (E)
Involvement of the deep fibers particularly of the extensor carpi radialis brevis component is most common. Discriminating focal areas of tendinosis and a partial tear on ultrasound can be difficult, particularly on MRI. On ultrasound a well-defined anechoic focus with no fibers intact or discrete cleavage planes are more typical of partial tears (Fig. 14.7).


Fig. 14.7
Lateral epicondylitis with partial tear. Sagittal ultrasound image of the common extensor origin (CEO) of the elbow joint shows a partial tear (calipers) of the common extensor tendon (E) seen as an anechoic focus with no fibers intact
MRI can also be used for evaluation particularly in the assessment of nonspecific elbow pain and those recalcitrant to conservative management. Studies reporting greater accuracy of MRI over ultrasound have generally not used Doppler ultrasound, which assists in the identification of the disorder. MRI shows the normal common tendons as homogenous low signal T1 and T2 structures. Similar changes are seen both in medial and lateral epicondylitis with tendon thickening and increased signal intensity on both the T1- and T2-weighted images (Fig. 14.8). This corresponds histologically to mucoid degeneration and neovascularization. Partial tears are depicted as thinning or partial disruption of the tendon and increased T2-weighted signal within and adjacent to the tendon origin (Bancroft et al. 2007). In common extensor tendinopathy, involvement of the radial collateral ligament should be assessed, as the involvement denotes a more advanced stage of the disease.
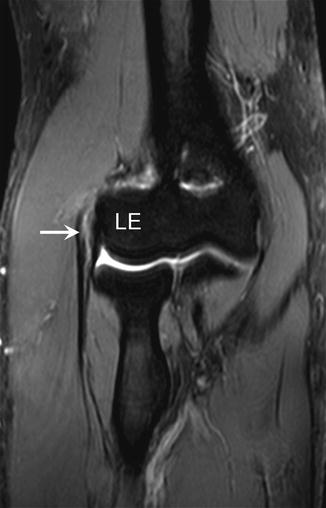
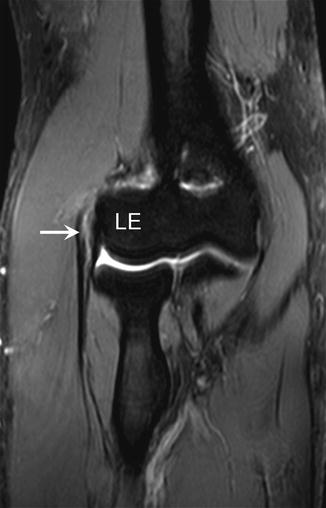
Fig. 14.8
Lateral epicondylitis. Coronal STIR MRI of the elbow demonstrates high signal (arrow) within the superficial and deep fibers of the common extensor tendon at its lateral epicondyle origin (LE)
Conservative treatment with rest, anti-inflammatory drugs and physiotherapy are the initial treatments. Percutaneous ultrasound dry needling supplemented with autologous blood or platelet-rich plasma therapy can be used for refractive cases. The role of corticosteroid injection is increasingly questioned. Surgery remains the final consideration with excision of the degenerated tissue, resection of the common tendon, and debridement of the common tendon origin.
14.4.2.2 Nerve Entrapment
Entrapment neuropathies can be difficult to differentiate from tendon disease particularly on the medial side where there is considerable overlap of symptoms between the conditions.
Ulnar neuropathy can be the result of compression or traction from valgus stress or in combination with chronic epicondylitis or ulnar collateral ligament insufficiency. Compression can occur due to a narrowed cubital tunnel, osteophytes from the ulnohumeral joint, muscle hypertrophy, or subluxation of the nerve. Subluxation can occur when the constraining Osborne ligament is injured or lax and is more likely when there is an enlarged or accessory medial head of the triceps. In itself, ulnar nerve subluxation is not always pathological, though its presence does render the nerve more prone to injury.
Entrapment of the posterior interosseous nerve, the motor branch of the radial nerve, causes lateral-side elbow pain and weakness, often confused with lateral epicondylitis. The nerve is most commonly compressed at the arcade of Frohse, a fibrous condensation at the leading edge of the superficial head of the supinator muscle. Other causes of posterior interosseous nerve and radial nerve compression include fibrous bands at either end of the radial tunnel and prominent vessels around the arcade of Henry.
Although uncommon, pronator teres syndrome has been described in racquet sports where entrapment of the median nerve occurs as the result of muscle hypertrophy of the dominant arm with entrapment between the 2 heads of the pronator teres (Frostick et al. 1999). Clinical manifestations include anterior pain and distal paresthesia worsened with resisted pronation. An accessory head of the pronator teres may also lead to neural compression.
The anterior interosseous nerve is a major branch of the median nerve and compression of this nerve causes Kiloh-Nevin syndrome. As the nerve is purely motor, compression leads to dysfunction of the flexor pollicis longus, pronator quadratus, and flexor digitorum profundus to the second and third digits and the inability to oppose thumb and index finger. The nerve can be compressed between the heads of the pronator teres muscle and the proximal edge of the flexor digitorum superficialis arch or due to anatomical variants such as Gantzer muscle, an anomalous head of the flexor pollicis longus.
Entrapment of the lateral cutaneous nerve of the forearm has been reported in racquet players (Retting and Patel 1995). The nerve is compressed between the distal biceps tendon and the brachialis muscle, probably secondary to repetitive elbow hyperextension (Cabrera and McCue 1986).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree