Fig. 15.1
Fish bone in the hypopharynx. (a, b) Lateral view of the neck and sagittal CT reformation demonstrating fish bone (curved arrow) in the prevertebral soft tissue, at the level of the C5 vertebra

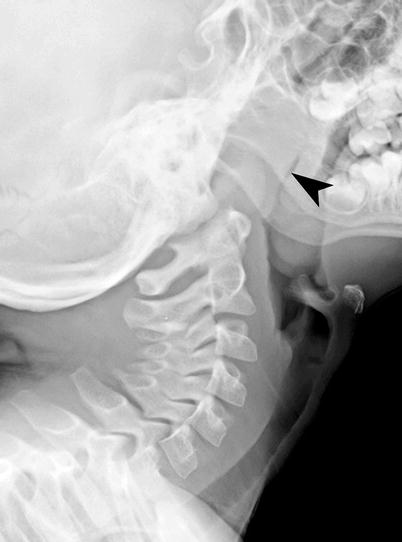
Fig. 15.2
Foreign body in the hypopharynx. (a) AP and lateral radiographs of the neck demonstrating radiopaque coin (curved arrow) lodged in the prevertebral soft tissues, above the cricopharyngeus. (b) Sagittal CT reformation of the neck demonstrates a plastic foreign body (arrowhead) in the prevertebral soft tissues, lodged just proximal to the cricopharyngeus muscle. (c) AP radiograph of the neck demonstrates radiopaque bottle cap (arrowhead) lodged in the hypopharynx soft tissues, above the cricopharyngeus
Radiopaque coins are the most commonly ingested foreign body in the pediatric patient. In patients with symptoms related to the esophageal coin, immediate removal with endoscopy is recommended, while in asymptomatic patients with esophageal coin, conservative management for 12–24 h is recommended, with the hope of spontaneous passage of the coin [2]. The management of esophageal coin in asymptomatic patients where the coin is located below the thoracic inlet includes next radiograph. If the follow-up x-ray demonstrates persistent esophageal coin, then endoscopic removal is required [3].
Infections
Oral cavity infections are most often related to periodontal diseases. Periodontal infection originates from gingivitis and leads to periodontal pocket of infection, seen as radiolucency around the root of the teeth. Infections from periodontal disease can extend into the submandibular or sublingual space, depending on whether the roots of the teeth extend above or below the mylohyoid muscle insertion. Cortical destruction is more common on the lingual aspect of the mandible than the buccal aspect because of the thinner cortex on the lingual aspect. Odontogenic infection from incisors, canines, and first premolar tends to involve the lingual space. The second and third mandibular molar roots extend below mylohyoid muscle insertion and therefore tend to involve the submandibular space.
Infection in buccal space arises from maxillary incisor, canine, premolar, and first molar. Masticator space infections arise from the second maxillary molar. Infection from the third maxillary molar tends to involve the parapharyngeal space.
On contrast-enhanced CT scan study, bony erosions can be identified around the root of the affected teeth, with extension of the abscess in to the soft tissues of the floor of mouth (Fig. 15.3) [4].
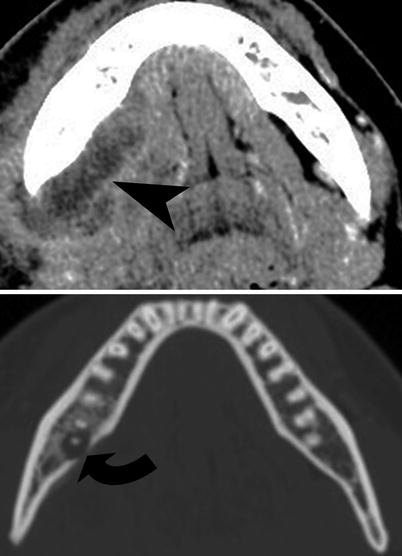
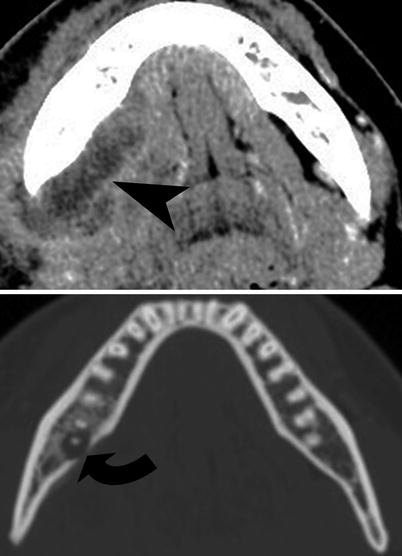
Fig. 15.3
Periodontal abscess. Contrast-enhanced CT scan study of the mandible demonstrates periodontal abscess (curved arrow) with extension of the abscess into the right submandibular triangle (arrowhead)
Sialadenitis
Sialadenitis refers to viral or bacterial infection of salivary gland, most commonly affecting the parotid gland. The frequency of viral infection (mumps) has drastically decreased due to the widespread use of immunization. The viral causes of sialadenitis include mumps virus (most common), HIV, coxsackie, parainfluenza virus, and herpes virus. Bacterial infection can be caused by obstruction of Wharton’s duct (submandibular gland) or Stensen’s duct (parotid gland) by sialolithiases. The most common organisms causing sialadenitis include Staphylococcus aureus, Streptococcus viridans, Haemophilus influenzae, Streptococcus pyogenes, Pseudomonas aeruginosa, and Escherichia coli. Sjögren syndrome most commonly is associated with parotid sialadenitis, keratoconjunctivitis sicca, and xerostomia.
Salivary gland duct obstruction secondary to sialolithiases most commonly involves the submandibular gland. The stones are most commonly composed of calcium phosphate or calcium carbonate and are usually radiopaque enough to be visible on plain radiography. Eighty to ninety-five percent of submandibular gland sialolithiases are radiopaque and therefore seen on plain radiography [5]. Sialography is the imaging modality of choice for demonstration of the salivary gland ducts.
The salivary gland can be imaged using plain radiography, sialography, ultrasonography, and CT scan. CT allows excellent comparison with contralateral salivary gland, demonstrating sialolithiases, distinguishing intrinsic from extrinsic inflammatory process, and defining abscess/phlegmon formation. Sialadenitis is typically seen on CT as salivary gland enlargement, surrounding inflammatory changes and ductal dilatation with calculi (Fig. 15.4) [6].
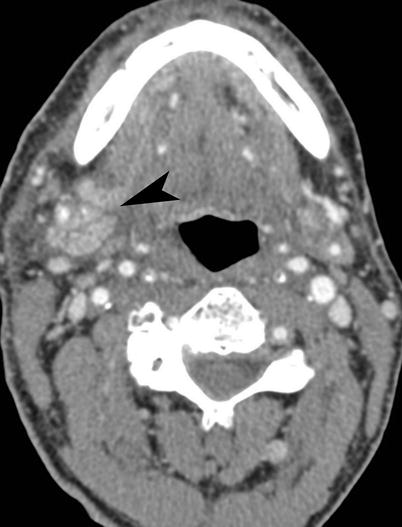
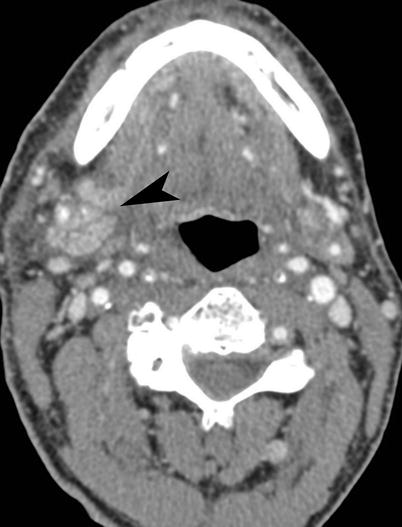
Fig. 15.4
Sialadenitis. Contrast-enhanced CT scan study of the floor of the mouth demonstrates unilateral enlargement of the right submandibular gland (arrowhead) with surrounding edema
Danger Space and Retropharyngeal Space Abscess
Danger space is located posterior to the retropharyngeal space and is bounded anteriorly by the alar fascia and posteriorly by the prevertebral fascia. The clinical significance of danger space infection is that the infection can directly spread to the posterior mediastinum, on either side of midline.
The retropharyngeal space is located between the buccopharyngeal fascia (visceral fascia surrounding the pharynx) and alar fascia. It is bounded laterally by the parapharyngeal space and carotid sheath. Inferiorly it extends to the level of the tracheal bifurcation, and superiorly it extends to the base of skull.
The plain radiographic findings include prevertebral soft tissue thickening, which is indicated by retrotracheal space (at C6) more than 14 mm in children and 22 mm in adults. Contrast-enhanced CT is the definitive test for demonstration of the size, location, and extent of the abscess in the deep spaces of the neck. It is not possible to distinguish retropharyngeal space from danger space abscess, unless the abscess is seen extending below the T4 vertebra (Fig. 15.5).
Fig. 15.5
Danger space abscess (a, b) and retropharyngeal abscess (c). (a) Sagittal information on the neck and chest demonstrates air containing abscess cavity (arrowheads) located posterior to the esophagus and extending from the neck into the mediastinum. (b) Plain radiograph of the neck also demonstrates the containing abscess cavity (arrowheads) in the prevertebral soft tissues. (c) Sagittal CT reformation demonstrates low-density retropharyngeal abscess (curved arrow) in the prevertebral soft tissues
Retropharyngeal Abscess
It is most commonly seen before the age of 6 years and is most often caused by Staphylococcus, Streptococcus, and Haemophilus. It most often arises secondary to suppurative changes in retropharyngeal lymph nodes draining tonsillitis, pharyngitis, or otitis media [7]. These suppurative lymph nodes can rupture and result in retropharyngeal abscess. The retropharyngeal abscess may also be caused by spine surgery, discitis, vertebral osteomyelitis, or pharyngeal perforation.
Contrast-enhanced CT is the imaging modality of choice and can show prevertebral soft tissue swelling and loculated abscess with enhancing wall (Fig. 15.8b). It can also show other findings such as discitis/osteomyelitis, airway compromise, thrombophlebitis, and epidural abscess.
Lemierre’s Syndrome
Lemierre’s syndrome, also called postanginal sepsis or necrobacillosis, is characterized by thrombophlebitis in the neck, most often due to Fusobacterium necrophorum infection [8]. Other species of Fusobacterium species are responsible for 11 %, and other gram-negative organisms are responsible in 8 % of cases of Lemierre’s syndrome [9]. It most commonly affects young adults after a complicated pharyngitis with parapharyngeal or peritonsillar abscess formation. These abscesses provide optimal surroundings for the growth of the anaerobic bacteria, which proliferate to involve the adjacent internal jugular vein. The thrombophlebitis of the internal jugular vein can cause embolization of the infected clot to the lungs and septicemia.
The imaging findings of septic thrombophlebitis and associated abscess can be demonstrated on US or CT study. The acute internal jugular vein thrombus can be seen on contrast-enhanced CT as low-density filling defect with distension of the vein (Fig. 15.6). Contrast-enhanced CT can also demonstrate the septic microemboli to the lungs indicated by multiple peripheral round- or wedge-shaped nodules and lung abscess formation. Other pulmonary findings include consolidation, pleural effusion, and empyema.
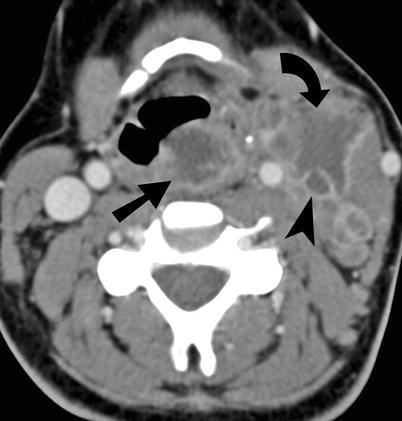
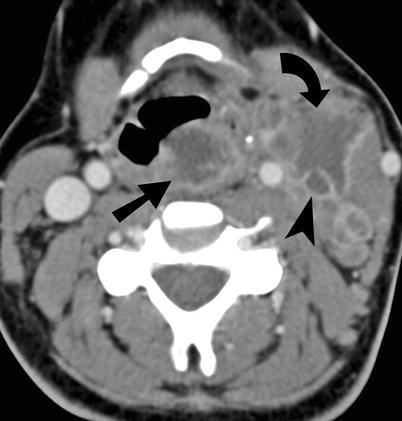
Fig. 15.6
Lemierre syndrome. Contrast enhanced CT scan study of the neck demonstrates retropharyngeal abscess (straight arrow) with extension on the left side to produce left internal jugular vein (arrowhead) thrombophlebitis. The septic thrombus in the left internal jugular vein is also producing abscess (curved arrow) in the soft tissues of the left anterior triangle of the neck
Tonsillitis and Peritonsillar Abscess
Peritonsillar abscess is a complication of acute tonsillitis, due to extension of infection through the tonsillar capsule, to the potential space between the capsule and the superior constrictor muscle. It represents the most common deep soft tissue infection of the neck, most commonly caused by Staphylococcus, Streptococcus, Haemophilus, pneumococcus, Fusobacterium, and Peptostreptococcus.
Imaging is most often performed in cases of complicated tonsillitis, where peritonsillar infection is suspected. The imaging findings include palatine tonsillar enlargement, striated enhancement, peritonsillar liquefaction, and loculated abscess formation (Fig. 15.7). The definitive treatment of peritonsillar abscess is surgical incision and drainage in the emergency room after intravenous antibiotics.
Fig. 15.7
Tonsillitis and peritonsillar abscess. (a) Lateral radiograph of neck demonstrates enlargement of the pharyngeal tonsils (arrowheads) in the lateral wall of the oropharynx. (b–d). Contrast-enhanced T1-weighted MRI and noncontrast CT (axial and coronal) demonstrate bilateral palatine tonsillar enlargement (bifid arrow). (e) Contrast-enhanced CT scan study of the upper neck demonstrates left peritonsillar abscess (curved arrow), producing mass effect on the oropharyngeal airway. (f) Contrast-enhanced T1-weighted MRI of the upper neck demonstrates left peritonsillar abscess (arrowhead) with mass effect on the oropharyngeal airway
Adenoidal Hypertrophy
Adenoidal hypertrophy is common in the 6-month to 6-year age group. Clinical examination and flexible nasopharyngoscopy can be performed to evaluate the adenoidal size. Nasal endoscopy may be complementary to lateral radiograph of the neck in evaluation of the adenoids [10]. Although its role is controversial, lateral radiograph of the neck was shown to be a reliable diagnostic test in the evaluation of hypertrophied adenoids (Fig. 15.8a) [10, 11].