, Paul F. von Herrmann1, Harigovinda R. Challa2 and Johanne E. Dillon2
(1)
Department of Radiology, University of Kentucky, 800 Rose Street, HX-307B, Lexington, KY 40536-0293, USA
(2)
Division of Pediatric Radiology, University of Kentucky, Lexington, KY, USA
Abstract
The diagnosis and management of pediatric patients in the emergency department has unique challenges that often require a different approach by the clinician than with an adult patient. Although children may develop many of the same illnesses as adults, certain life-threatening diagnoses are seen more often in the pediatric population. An immature immune system, small body size, and developmental anomalies are several factors that can place children at an increased risk for specific diseases. This chapter will focus on the imaging evaluation of diagnoses that occur more often or with a unique appearance in the pediatric population.
Introduction
The diagnosis and management of pediatric patients in the emergency department has unique challenges that often require a different approach by the clinician than with an adult patient. Although children may develop many of the same illnesses as adults, certain life-threatening diagnoses are seen more often in the pediatric population. An immature immune system, small body size, and developmental anomalies are several factors that can place children at an increased risk for specific diseases. This chapter will focus on the imaging evaluation of diagnoses that occur more often or with a unique appearance in the pediatric population.
Neurology
Acute Disseminated Encephalomyelitis (ADEM)
Acute disseminated encephalomyelitis is a diagnostic challenge both to the clinician and the radiologist owing to its similarity in presentation with other diseases, specifically multiple sclerosis (MS). The disease is an acute demyelinating process (often preceded by a viral illness or vaccination) predominantly affecting the white matter, deep gray matter, brain stem, and spinal cord with an estimated mortality rate as high as 5 % [1]. Because of the confusing and severe presentations of patients, imaging is frequently obtained for further evaluation.
Magnetic resonance imaging (MRI) of the head is the preferred modality for evaluation of the majority of patients with symptoms suggestive of ADEM, and further evaluation with MRI of the spine is often performed as well. The limited literature available comparing the sensitivity of computed tomography (CT) to MRI suggests that MRI is far superior both in sensitivity and specificity compared to CT [2]. CT may be performed initially to exclude neurosurgical emergencies, but CT will often underestimate the extent of disease and may not appropriately characterize the condition. On MRI, the imaging findings of ADEM are similar to other demyelinating disorders and typically include focally increased signal in the white matter on T2-weighted sequences, mild enhancement on postcontrast sequences, and restricted diffusion in acute lesions (Fig. 26.1). The distribution of lesions is variable, though certain patterns of involvement may help favor the diagnosis of ADEM over MS. The thalamus (30–40 %), basal ganglia (30–40 %), cerebellum (30–40 %), and brain stem (45–55 %) are affected more frequently in ADEM than MS, and the periventricular white matter and corpus callosum are frequently spared [3, 4].
Fig. 26.1
ADEM. (a–c) Axial FLAIR sequence images in a 4-year-old girl demonstrate increased signal in the bilateral subcortical white matter (curved arrows), bilateral thalami (arrowheads), and middle cerebellar peduncle (straight arrows) involvement
Treatment includes admission for administration of intravenous steroids and for some patients, intravenous immunoglobulin. The majority of patients will improve clinically with mild residual impairment in 57–90 % of patients [1]. Disease relapses are possible.
Intracranial Complications of Acute Otitis Media and Sinusitis
Due to the high prevalence of viral infections and the small diameter of draining pathways for the middle ear cavity and sinuses, children are at increased risk for developing acute otitis media (AOM) and acute sinusitis. In rare cases, the infection can extend intracranially. Meningitis, intracranial abscesses, and septic thrombosis of intracranial venous structures may result. Patients with known or suspected sinusitis or AOM presenting with sudden worsening of headache, visual symptoms, seizures, or neurologic deficits may necessitate imaging for further evaluation.
MRI of the head with contrast is the examination of choice to evaluate for intracranial spread of infection. The specificity of MRI is superior in evaluation for meningitis and intracranial abscesses and in differentiating dural reaction from extra-axial or intra-axial abscess. Early in the process, meningeal inflammation may be the first abnormality present, which typically appears as meningeal enhancement on both CT and MRI. As an extra-axial abscess develops, the appearance is typically a fluid collection with high T2 signal intensity and low T1 signal intensity on MRI and usually higher attenuation relative to cerebrospinal fluid (CSF) on CT (Fig. 26.2). Abscess on either modality generally demonstrates peripheral enhancement on postcontrast images. Dural venous or cavernous sinus thrombosis are often challenging with either CT or MRI, though thrombosis is best established on postcontrast images on either a CT or MR venogram examination appearing as a filling defect in the venous structure. Venous congestion may result from septic venous thrombosis and vasogenic and cytotoxic cerebral edema, sometimes with associated susceptibility artifact (representing hemorrhage) or restricted diffusion, may be seen in the parenchyma drained by the thrombosed dural venous sinus (Fig. 26.3) [5]. Cerebritis typically manifests as focally decreased attenuation on CT and increased T2 signal intensity in the brain parenchyma on MRI. As the process progresses to abscess formation, either modality will demonstrate progressive peripheral enhancement on postcontrast imaging along with surrounding vasogenic edema. Intracranial abscesses often exhibit restricted diffusion on MRI.
Fig. 26.2
Frontal sinusitis with subdural empyema. (a) Axial CT images of an 11-year-old boy exhibits opacification of the right maxillary (arrow) and frontal sinuses (arrowhead). (b) Axial post-gadolinium T1-weighted image demonstrates oval abscess (arrow) with meningeal enhancement in the interhemispheric fissure
Fig. 26.3
Cavernous sinus thrombosis. (a, b) Axial and coronal T1-weighted post-gadolinium demonstrates enhancement and enlargement of the left cavernous sinus (white arrow) in a patient with marked mucosal enhancement of the adjacent sphenoid sinus. Note the diminished caliber of the left internal carotid artery (black arrow) relative to the right side due to mass effect
Intravenous antibiotics are indicated for intracranial spread of infection. Treatment of intracranial abscess typically involves surgical drainage. Septic thrombosis of the dural venous sinuses and cavernous sinus is managed with intravenous antibiotics and surgical drainage of the adjacent infectious source.
Orbital Infection: Subperiosteal Abscess and Orbital Cellulitis
Infection in the orbit constitutes an ophthalmologic emergency. Whether as a result of sinusitis or periorbital cellulitis extending across the orbital septum, this constitutes an emergency as the infection can cause blindness and spread intracranially. Imaging may be performed to determine the extent of the infection, to localize an abscess or for surgical planning.
CT of the orbits is often the first imaging modality ordered because it is quick, accessible, and has a high sensitivity and specificity; however, according to the 2009 American College of Radiology (ACR) Appropriateness Criteria, contrast-enhanced MRI is recognized as a first-line imaging test to evaluate orbital infections. With periorbital cellulitis invading the orbit, the infection typically invades medially as the orbital septum is thinner in its medial portion. Orbital cellulitis will be seen on CT as obliteration of fat planes and soft tissue enhancement if contrast is administered. On MRI, the infection will demonstrate low T1 signal intensity, high T2 signal intensity and soft tissue enhancement. In regards to subperiosteal abscess, the findings at CT generally include an extraconal fluid collection adjacent to an opacified sinus. Early orbital abscesses may not demonstrate peripheral enhancement on contrast-enhanced examinations on CT (Fig. 26.4) [6]. On MRI, subperiosteal abscesses have low T1 signal intensity, high T2 signal intensity, often peripherally enhance and often restrict diffusion (Fig. 26.5). When contrast is administered, both MRI and CT are acceptable in diagnosing superior ophthalmic venous thrombosis.
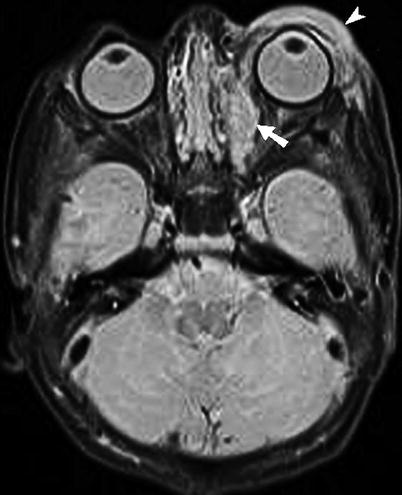
Fig. 26.4
Subperiosteal abscess. (a, b) Axial and coronal CT image demonstrates ethmoidal and frontal sinusitis with right extraconal subperiosteal abscess (arrow), adjacent to the medial rectus muscle. There is breech identified in the right lamina papyracea (arrowhead)
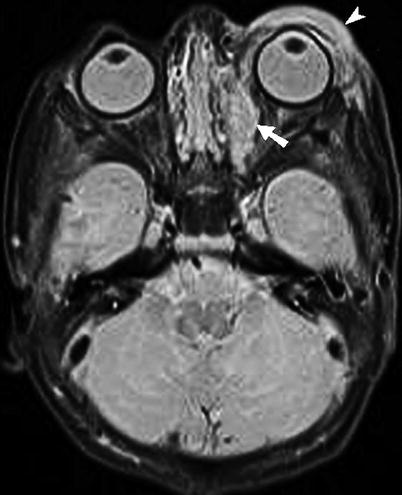
Fig. 26.5
Subperiosteal abscess. T2-weighted STIR sequence in an 8-day-old demonstrates subperiosteal abscess (short white arrow) along medial wall of the left orbit, secondary to ethmoidal sinusitis. There is left-sided proptosis with preseptal edema (arrowhead)
Treatment for orbital cellulitis is intravenous antibiotics. Subperiosteal abscess typically warrants surgical intervention especially when there is visual acuity loss or paralysis of extraocular muscles.
Transverse Myelitis
One of the more neurologically devastating diagnoses is transverse myelitis, which is defined as demyelination across the spinal cord that can occur at any level. Back pain and sensory deficits are common presenting symptoms. In addition to CSF analysis, imaging is often warranted to support the diagnosis and define its extent, as well as to exclude a mass in the spinal column that could produce similar symptoms but would have a different treatment.
MRI of the spine with contrast is the examination of choice in patients with suspected transverse myelitis, and MRI of the head is often also obtained. Affected portions of the spinal cord characteristically have increased signal on T2-weighted images and typically span at least two-thirds of the spinal cord in transverse dimensions (Fig. 26.6). There may be edema resulting in expansion of the cord. Contrast enhancement, usually peripherally around the lesion, may be seen in a significant percentage of patients [7].
Fig. 26.6
Transverse myelitis. (a, b) Axial and sagittal T2-weighted images of the thoracic spine demonstrate multiple foci of abnormal increased signal (arrowheads) extending transversely through the spinal cord in an acutely paraplegic 18-year-old male
Treatment generally includes intravenous steroids, though some patients may also receive plasmapheresis. Prognosis is variable with approximately one-third of patients fully recovering and one-third of patients regaining minimal to no function.
Ventriculoperitoneal Shunt Malfunction
Ventriculoperitoneal (VP) shunts are usually placed to treat hydrocephalus. Shunting malfunction may manifest with either increased or decreased ventricle size with accompanying changes in intracranial pressure. Radiologically important causes of shunt malfunction include shunt valve malfunction, infection, tubing discontinuity, and loculated CSF accumulation in the peritoneal cavity (CSF pseudocyst), each of which are treated differently. Radiologic evaluation is usually indicated to confirm a change in size of the ventricles, evaluate for other intracranial abnormalities as well as to identify potential underlying mechanisms of disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree