Fig. 17.1
Sagittal fat-suppressed T2- (a), T1- (b), and axial fat-suppressed T2-weighted (c) MRI of the lumbar spine show L5/S1 disc signal alteration with impingement of the intact posterior longitudinal ligament
Fig. 17.2
Axial (a) and sagittal reformatted (b) CT images of the lumbar spine show L5/S1 lumbar disc herniation
Fig. 17.3
Sagittal fat-suppressed T2- (a), T1- (b), and axial T2-weighted (c) MRI of the lumbar spine show a relatively recent Schmorl node (arrow) at the endplate of L2 with adjacent bone marrow edema
The pars interarticularis is a thin isthmus of bone that connects the superior to the inferior articular process of the posterior elements of the vertebral body. At its upper extent it is connected to the vertebral body by the pedicle. Spondylolysis is the forward displacement of one vertebra relative to the next leading to a step in the posterior vertebral line. It is caused by a defect of the pars intra-articularis and, in most cases, represents a fracture secondary to an overuse stress injury caused by the repetitive loading of the lumbar spine. The severity of the slip is expressed in 4° ranging from a low grade I (less than 25 % slip) in steps of 25 % to a complete displacement of the vertebrae (type IV) (Fig. 17.4). Whenever sporting activity involves hyperextension and hyperextension rotation, there is risk of these stress fractures. However, the association of pars defects and spondylolysis with rowing is under debate (Dragoni et al. 2007; Rossi and Dragoni 1990; Soler and Calderon 2000). It is possible that rowing simply exacerbates lesions acquired from other activities earlier in life and it may be that with proper technique the rowing activity will not cause the fracture. Conventional radiographs, CT, skeletal scintigraphy, MRI, and even pars blockades may be used for the investigation of spondylolysis. Several techniques in combination may be required to provide a complete answer. For many the first step in imaging will be conventional radiographs. In many cases CT and MRI are recommended for further assessment (McNally et al. 2005), and in many centers MRI will be used as the first investigation as it does not employ ionizing radiation and is more likely to give a specific diagnosis. Most importantly MRI will show bone edema in the pars interarticularis before a fracture occurs allowing preventative changes in the athlete’s activity and permitting the injury to heal spontaneously. Interestingly, rowers who do not develop back pain in their teens or early twenties have significantly lower rates of back pain as they age than the general population. If a rower completes a junior rowing career without experiencing back pain, his or her prognosis for back pain later in life is better than that of the general population (Smoljanović et al. 2011; Teitz et al. 2002). Those rowers who present with lower back pain must be examined carefully to help prevent serious damage and late sequelae.
Fig. 17.4
Sagittal reformatted (a) and axial (b) CT images of the lumbosacral spine shows spondylolysis in L5/S1 (arrow) with mild anterior slipping and narrowing of the intervertebral foramen
17.2.3 Sacrum
Sacroiliac pain is not unusual in rowers. There is no definite difference in the incidence of sacroiliac joint complaints among the different rowers und scullers (McNally et al. 2005; Timm 1999). Sacroiliac pain may be referred to the upper thigh but rarely below the knee. Whether the pain originates from the joint and/or the substantial and thick complex of sacroiliac and lumbosacral ligaments is a matter of debate. Some practitioners advocate anesthetic blocks, with a short-acting local anesthetic in one structure and longer-acting local anesthetic in the other. The duration of pain relief will help to determine the origin of pain and may guide the choice of treatment. Stress reaction and edema in bone may occur, especially in the older population.
17.2.4 Thoracic Wall
Stress injuries are the result of overload of normal muscle, ligaments, entheses, or bone due to substantial load and repetitive activity. They may also occur with much less load when the bone or soft tissue is weak or previously injured. Rib stress fractures follow an imbalance between the rate of bone resorption and bone formation during bone remodeling (Figs. 17.5 and 17.6) (Christiansen and Kanstrup 1997; Dragoni et al. 2007). Early injuries may not show a fracture line, with only edema observed. Later partial fractures without displacement occur; if the load continues, they may progress to full fractures and potentially displacement. In general, stress fractures in athletes are the result of excessive, repetitive loads on normal bones that have not been adapted to these activities. They are exacerbated when the athlete elects or is encouraged to “train through the pain.” A series of rib stress fractures in elite female rowers was reported in 1985 (Holden and Jackson 1985; Vinther et al. 2005). Many of the diagnoses were made using nuclear medicine (bone scintigraphy), and it is not clear which of these injuries were intercostal muscle tears, which were periosteal avulsion injuries, and which were bone stress lesions. Bone scintigraphy will be positive for all these conditions. Stress injuries of the intercostal space and ribs are a known specific rowing-related injury and account for the most time lost from on-water training and competition (Wajswelner et al. 2000; Warden et al. 2002). They are one of the most common reasons for medical attention to rowing athletes in major championships. Therefore, early recognition is crucial for appropriate treatment and early return to rowing. Rates of occurrence of about 6–22 % have been reported (Dragoni et al. 2007; Wajswelner et al. 2000; Warden et al. 2002). Fractures generally occur during periods of intense training and usually lead to serious effects on rowing performance. Elite rowers are more likely to experience rib stress fractures than beginner or intermediate rowers. Rib stress fractures are more prevalent among rowers between 22 and 27 years of age, which is also the age range of most elite rowers. The etiology of stress fractures of the rib is probably multifactorial (McGregor et al. 2004; Wajswelner et al. 2000; Warden et al. 2002). The injuries may have little to do with age alone, but may be more influenced by level of performance and training loads (McDonnell et al. 2011). Equipment and technical factors including poor stroke mechanics, a lack of flexibility and/or strength, and a sharp increase in training loads contribute to stress phenomena (Christiansen and Kanstrup 1997). There is no difference in injury incidence between sweep rowers and scullers. Rib or intercostal stress injuries can occur in any location of any rib but most commonly occur in the anterolateral or dorsolateral aspect of the chest wall, typically in the region of the sixth to tenth ribs. Although rib stress fractures have been reported equally for sweep rowing and sculling, the locations of injuries are slightly different. In sweep rowing, 81 % of rib stress fractures occurred in the anterolateral/lateral aspects of the rib cage on the side away from the oar, while in sculling they tend to occur evenly along the anterolateral/lateral and posterolateral/posterior aspects of the rib cage (McDonnell et al. 2011). Intercostal stress injuries present with sharp intercostal pain, which is increased by coughing and even deep breathing. Localized complaints in the region of the affected rib radiating anteriorly as well as posteriorly to the axillary area are characteristic (Dragoni et al. 2007; Hosea and Hannafin 2012). Biomechanical studies suggest that the highest bending stresses occur at the posterolateral section of the rib. To transfer the force generated by the legs and trunk into the arms, and subsequently to the oar, the scapulothoracic muscles, especially the serratus anterior, contract maximally at the catch (Boland 1986). Rib fractures in rowers are caused by the repeated rowing stroke with contraction of the serratus anterior and external oblique muscles leading bending forces to the lateral segment of the rib (Karlson 1998). The risk may be increased also by low calcium, low vitamin D, eating disorders, low testosterone, or use of depot progesterone injections (McDonnell et al. 2011; Wajswelner et al. 2000; Warden et al. 2002). Treatment begins with a change to the training schedule to reduce the load on the affected area. This may be as simple as changing the side the swept oar athlete rows on. Many rowers will become more comfortable training on a single side of the boat and a change may be curative albeit disruptive to crew lineups. Cross-training will be the first choice for scullers who cannot select which side to row.
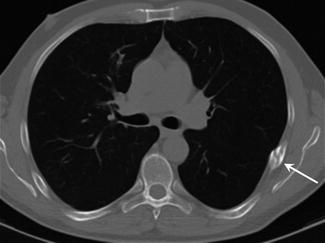
Fig. 17.5
Coronal (a) and axial (b) fat-suppressed T2- and axial T1-weighted (c) MRI of the right rib cage show rib stress fractures (arrow) in the lateral aspect of the thorax
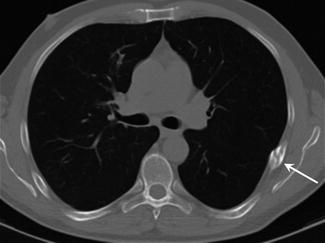
Fig. 17.6
Axial CT image of the rib cage shows a dorsolateral rib stress fracture (arrow)
17.2.5 Knee
As rowing is a non-weight-bearing activity, rowers’ knees typically do not sustain traumatic ligamentous or meniscal injury. However, the knee of the competitive rower is at some risk for overuse injury due to the strain of repetitive maximal loading in the fully flexed position. Not surprisingly patellofemoral pain syndrome is a common complaint among rowers. The knee is subjected to large patellofemoral compression loads during training and especially competitions. In a survey of rowing-related injuries, the knee was the most commonly affected site (Boland 1986; Hosea and Hannafin 2012). Two typical overuse syndromes encountered in rowers are iliotibial band syndrome and patellar tendinitis (Figs. 17.7 and 17.8). However, chondromalacia patellae is not rare and can be exacerbated by maltracking. In case of patella alta, craniolateral impingement of Hoffa’s fat pad may also be observed and may cause complaints. Once these conditions become established, pain may be significant and rowing must be curtailed. Assessment of a rower presenting with generalized knee pain should include a history of previous injury such as patellofemoral dislocation or subluxation, locking, swelling, or giving way (Vinther et al. 2005).
Fig. 17.7
Coronal (a) and axial (b) fat-suppressed proton density-weighted MRI of the left knee show definite edema (arrow) between the iliotibial tract and lateral femoral condyle in keeping with iliotibial tract friction syndrome
Fig. 17.8
Sagittal T1- (a) and fat-suppressed T2-weighted (b) MRI of the knee show an enlargement and edema of the patellar tendon and to a mild degree the patella itself too, consistent with patellar tendinitis
Iliotibial band friction syndrome is discussed in the literature but seems to be very uncommon in the rowing population (Boland 1986). It may rather be caused or initiated by training outside the boat for increasing the condition generally or in winter. The iliotibial band originates as the tendinous extension of the fascia covering the gluteus maximus and tensor fascia latae muscles proximally and attaches to the Gerdy tubercle on the proximal aspect of the anterolateral tibial condyle. While sending fibers to the lateral intramuscular septum and the lateral aspect of the patella over the lateral femoral condyle, the iliotibial band is free to glide anteriorly and posteriorly. As the iliotibial tract moves frequently over the lateral condylar prominence of the knee in even mild varus deformity, inflammation and pain can result from friction, leading to complaints.
Patellar tendinitis is another overuse condition encountered in rowers and is characterized by anterior knee pain. The injury results from repetitive microtrauma to the patellar tendon just distal to the patellar attachment (Boland 1986).
With patella alta, repeated flexion and compression of the patella to the femur may lead to impingement of the uppermost part of Hoffa’s fat pad causing complaints (Fig. 17.9).
Fig. 17.9
Coronal (a) and axial (b) fat-suppressed proton density-weighted MRI of the knee show craniolaterally edematous changes at Hoffa’s fat pad (arrow). This alteration is caused by an impingement effect due to a patella alta
While rowing, repetitive knee flexion and extension generates large patellofemoral compression loads resulting in injury of the hyaline cartilage of the patella. Chondromalacia of the patella presents with complaints of anterior knee pain with rowing and quad-strengthening training activities (Fig. 17.10). Patients with chondromalacia, with recurrent knee effusions and pain, should be advised to discontinue rowing.