Fig. 6.1
Illustration of recession surgery. The lateral rectus, after being secured with suture is detached from the insertion site (a) and reattached at a proximal site by partial thickness scleral bites (b)
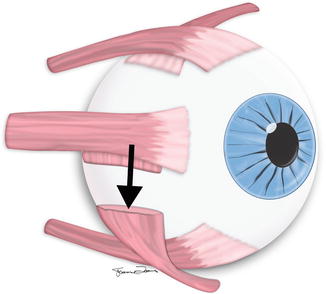
Fig. 6.2
Illustration of inferior oblique myectomy. The Inferior oblique muscle is hooked in the region between the lateral and inferior rectus muscles. A portion of the muscle is excised (myectomy) and the two ends allowed to passively reinsert on the globe. The distal end retracts to the anatomical insertion and the proximal end typically reinserts close to the lateral border of the inferior rectus, well posterior to its insertion (arrow)
The muscle slack resulting from the recession, myotomy, and tenotomy procedures can be depicted on imaging as increased maximum transverse diameter of the involved muscle belly (Fig. 6.3). Otherwise, it is difficult to appreciate the actual degree of recession as current imaging techniques cannot accurately identify the site of an extraocular muscle insertion when it is anterior to the equator of the eye (the most typical location), unless surface coils are used.
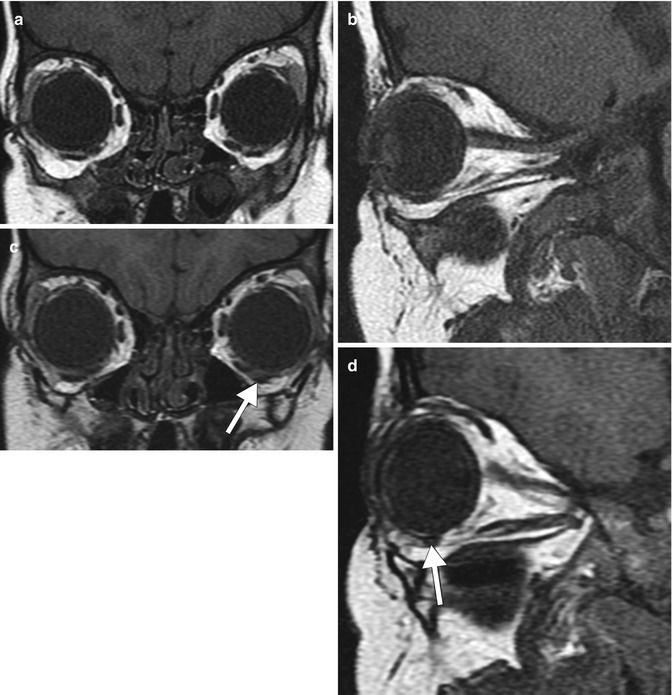
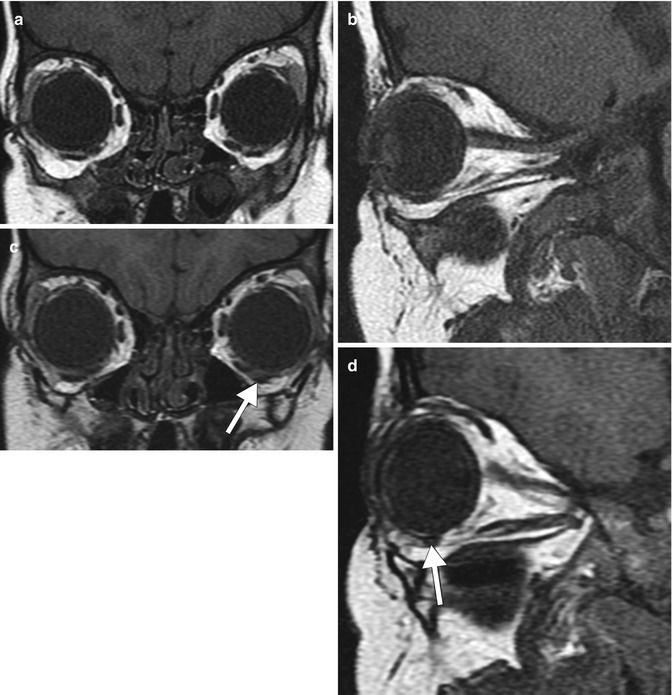
Fig. 6.3
MRI of inferior oblique myectomy with a residual band (top arrow). Coronal and sagittal T1-weighted MR images before (a, b) and after (c, d) surgery show that the left inferior oblique muscle belly has shifted slightly medially and has a larger cross-sectional diameter (arrows)
6.1.3 Muscle Strengthening Procedures
Resection and, Tuck/Plication. Muscle action can be augmented via tightening or shortening. Muscle shortening involves removing a specific length of muscle (“resection”) and reimplanting the foreshortened muscle on the globe (Fig. 6.4). Alternatively, a muscle tuck or plication procedure can provide equivalent shortening while preserving the anterior ciliary circulation by creating a redundancy in the muscle (Fig. 6.5). The effects of such procedures can be very subtle or not directly apparent even on high spatial resolution MRI. Nevertheless, MRI can be useful for delineating the postoperative anatomy, particularly when further surgery is contemplated (Figs. 6.6 and 6.7).
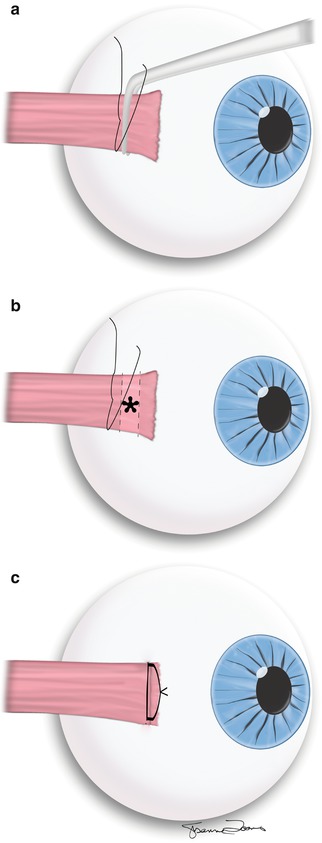
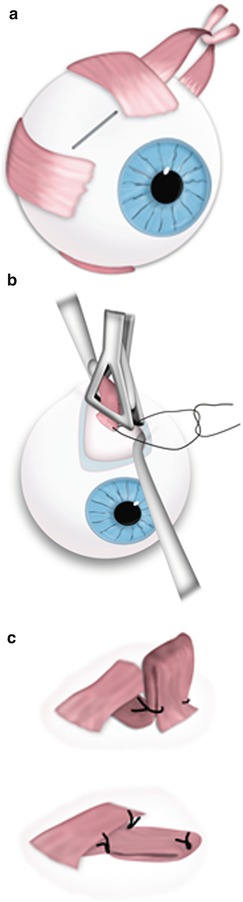
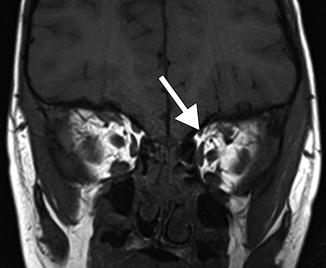
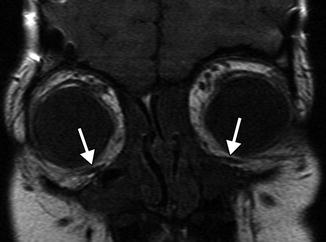
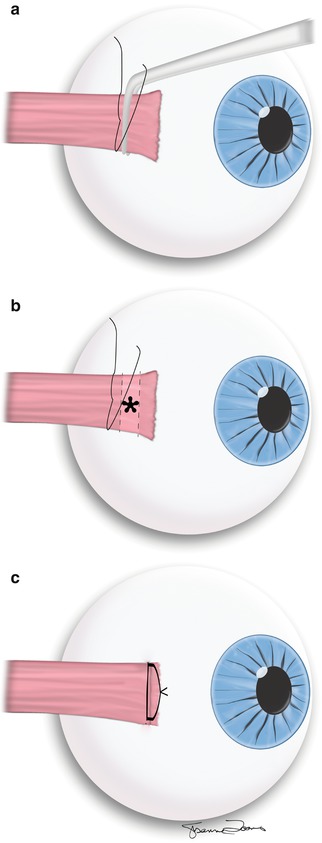
Fig. 6.4
Illustration of resection surgery. The rectus muscle is secured with sutures at a measured site distal to the muscle insertion. The muscle is then clamped and cut proximal to the sutures (a). The muscle stump is then removed (b) and the shortened (resected) muscle is advanced and secured at the anatomical insertion site (c)
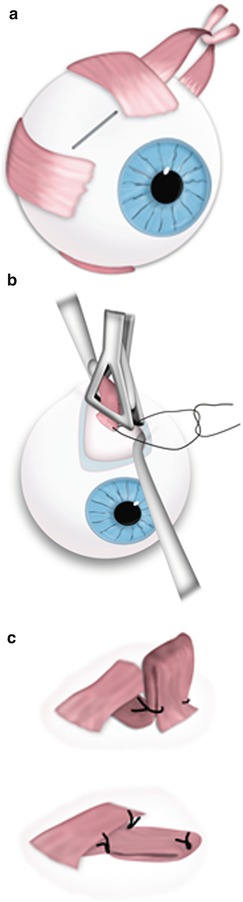
Fig. 6.5
Illustration of superior oblique tuck. Superior oblique is identified and secured with a hook (a). Superior oblique is lifted from the orbit, folded onto itself; folded muscle is secured with suture (b). Final configuration of the oblique tuck nasal to the superior rectus muscle (c)
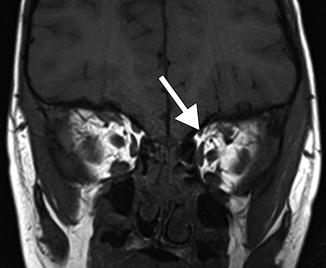
Fig. 6.6
Superior oblique tuck. The patient presented with persistent symptoms of left superior oblique palsy after superior oblique tuck. Coronal high spatial resolution T1-weighted MRI shows an asymmetrically small left superior oblique (arrow)
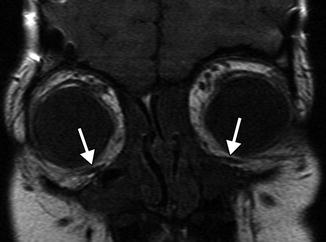
Fig. 6.7
Bilateral inferior oblique myectomy. Coronal high spatial resolution T1-weighted MRI shows the residual portions of the bilateral inferior oblique muscles (arrows)
6.1.4 Muscle Transposition
Transposition procedures are typically employed when loss of innervation to one or more of the extraocular muscles, or traumatic loss of an extraocular muscle, limits options to remediate the misalignment. Extraocular muscle transposition consists of disinserting and reattaching all or part of the muscle to the globe at a site remote from the original path of the muscle (Fig. 6.8). The purpose of this procedure is to alter the direction of the force vector and therefore, the action that the extraocular muscle exerts on the globe. For example, if the superior rectus is disinserted from the globe and reattached near the anatomical insertion of the lateral rectus muscle, it will lose some ability to elevate the eye and gain capacity to abduct or outwardly pull the eye. Transposition of the superior rectus with or without transposition of the inferior rectus to the region adjacent to the lateral rectus muscle is one option used to restore abduction in patients with sixth nerve palsy. In addition, botulinum toxin A can be injected into the medial rectus, or it can be recessed in order to limit its action. Splitting the lateral rectus into superior and inferior halves and transposing each nasally to a location adjacent to the medial rectus effectively pulls the eye medially and can remediate much of the misalignment created by complete third nerve palsy. High-resolution T1-weighted images can often adequately depict the path and morphology of transposed extraocular muscles (Fig. 6.9).
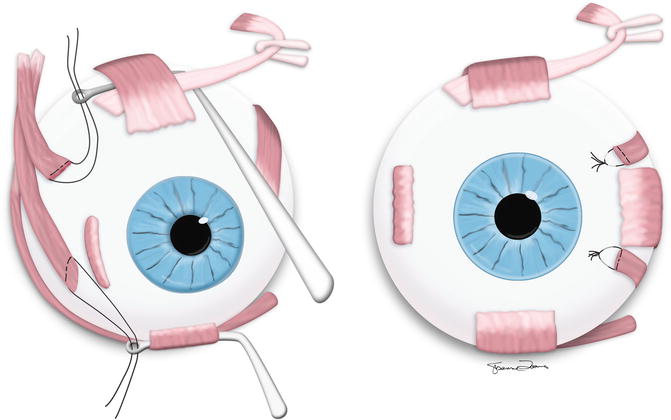
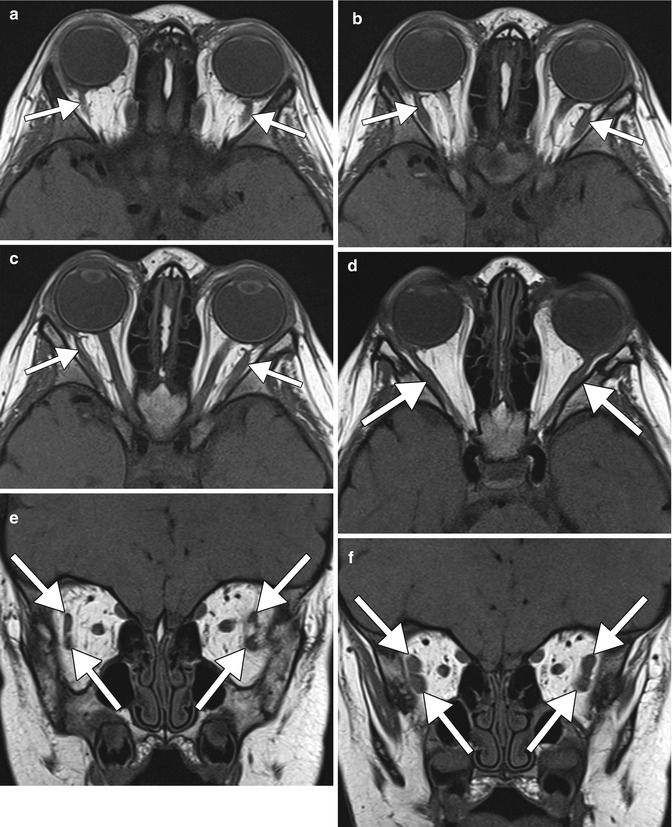
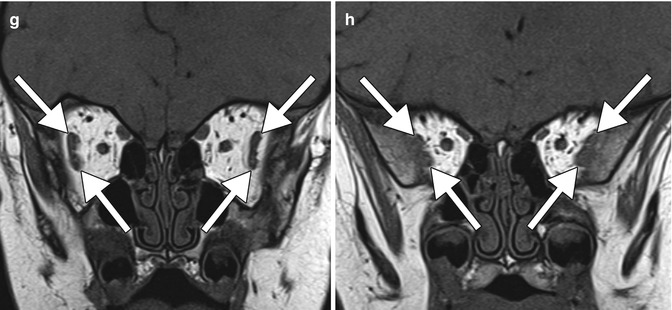
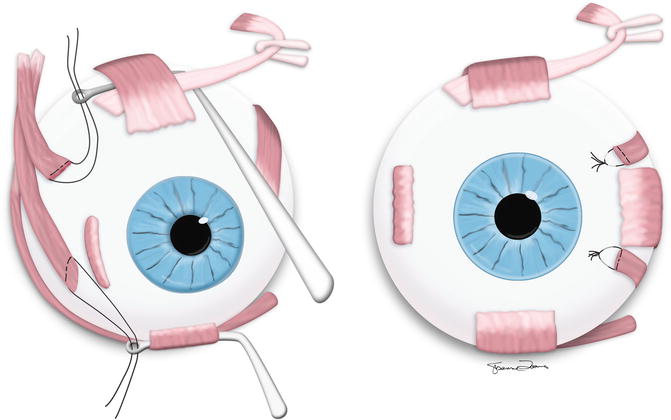
Fig. 6.8
Adjustable medial transposition of the split lateral rectus is one surgical option used to treat misalignment from complete third nerve palsy (Adapted with permission from Shah et al. (2014))
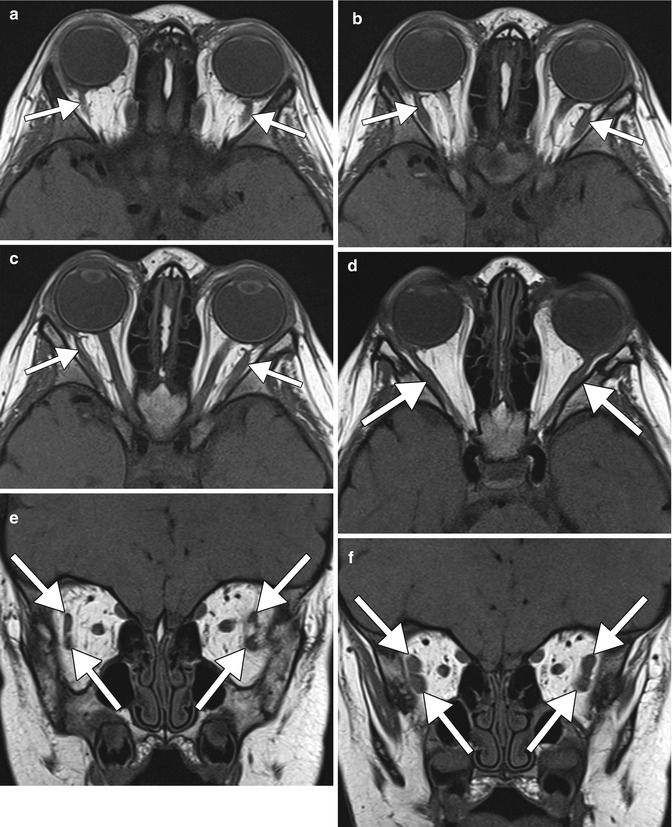
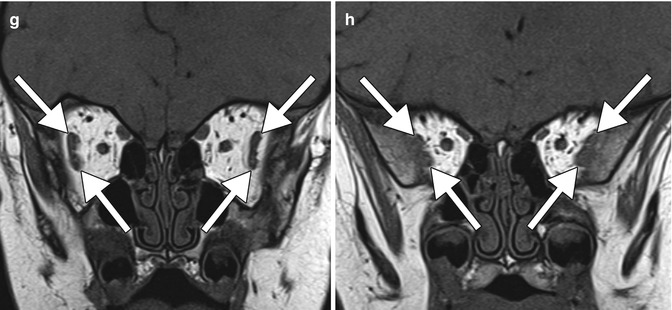
Fig. 6.9
Y splitting of the lateral rectus with medial transposition. The patient is a 19-month-old with bilateral third nerve palsy. Sequential axial (a–d) and coronal (e–h) T1-weighted MR images show splitting and thickening of both lateral rectus muscles distally (arrows) (Adapted with permission from Shah et al. (2014))
6.1.5 Chemosurgery
Botulinum toxin injection. Botulinum is a potent neurotoxin produced by the bacterium Clostridium botulinum. It interferes with neural transmission by blocking the release of acetylcholine, thereby resulting in muscle paralysis. Botulinum toxin administration or chemodenervation is a reasonable alternative to recession or other surgical weakening procedures in select cases. Although no structural changes in the muscle are discernable on imaging after chemodenervation, the improved ocular alignment can be appreciated (Fig. 6.10).
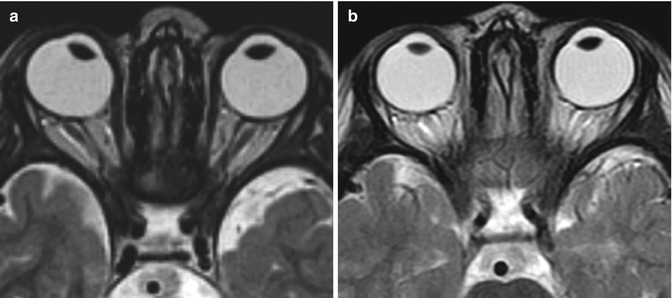
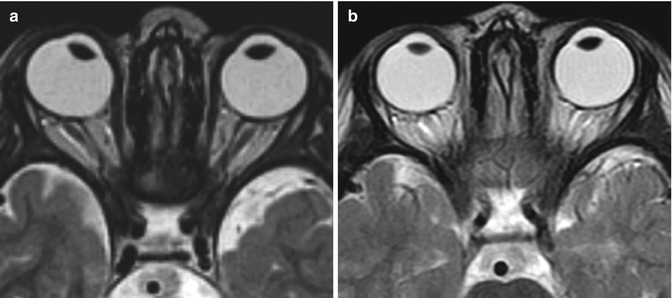
Fig. 6.10
Botulinum toxin. The patient has a history of complete sixth nerve palsy with medial rectus contracture, and is status post inferior rectus and superior rectus full tendon transposition to the lateral rectus of the right eye. The axial T2-weighted MR images obtained before (a) and after (b) botulinum toxin treatment to the right medial rectus muscle show improved alignment of the right globe
6.1.6 Complications of Strabismus Surgery
Slipped muscles. Extraocular muscles can “slip” from their intended insertion during strabismus surgery when the muscle capsule (external coat) is mistaken for muscle tendon or belly; the capsule, rather than the muscle, is sutured to the globe allowing the muscle to slide back within this capsular sheath, causing a more-than-planned recession effect. Slipped muscles can be retrieved by following the thin avascular muscle capsule posteriorly until the muscle is identified. In addition, muscle slippage or “loss” can occur if the suture securing the muscle to the sclera gives way, allowing the muscle to slip back or recess excessively, sometimes well behind the equator, and even off the globe. This is often called a “lost muscle.” In reality, residual check ligaments called “pulleys” and other connective tissue attachments typically approximate the muscle to the globe, thereby facilitating surgical recovery and repair. MRI can often depict the approximate location of the muscle insertion in cases of slipped or “lost” muscles, thereby facilitating recovery (Fig. 6.11).
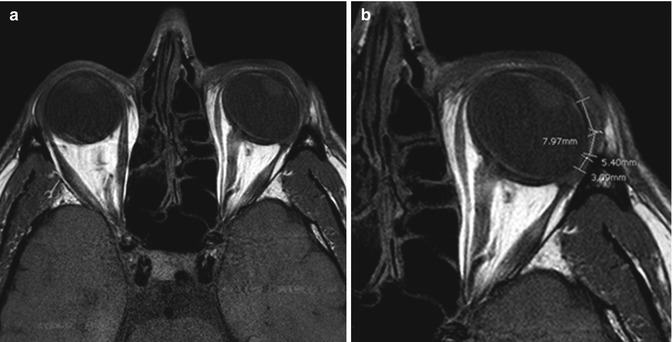
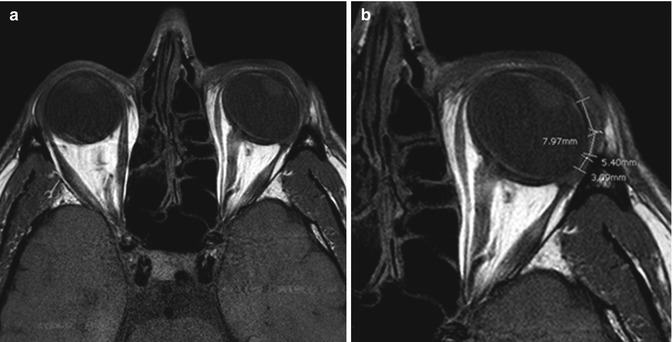
Fig. 6.11
“Lost” muscle after recession. Axial T1-weighted images without (a) and with (b) measurements drawn show the degree of posterior retraction of the left lateral rectus muscle (7.97 + 5.40 + 3.09 mm from limbus = 16.46 mm from limbus). Note the posterior widening of the muscle belly secondary to this extreme recession
Torn muscle/Pulled-in-two syndrome. Torn extraocular muscles from strabismus surgery can lead to pulled-in-two syndrome. Pulled-in-two syndrome describes the subtype of “lost muscle” that occurs when there is an unplanned horizontal transection of the muscle. This atypical transection can occur during strabismus surgery in cases of extreme muscle tension (e.g., with thyroid orbitopathy) or when the muscle is weakened by disease or prior surgical trauma. Orbital hardware such as an encircling band used to repair retinal detachment can predispose a muscle to such rupture. Unfortunately, the transection typically occurs at the tendon–muscle junction, approximately 10 mm from the muscle insertion, making recovery of the muscle challenging as the foreshortened muscle readily retracts behind the equator. MRI can be used to localize the distal ruptured muscle in anticipation of retrieval if recovery has not proven feasible during the initial surgical procedure (Fig. 6.12).
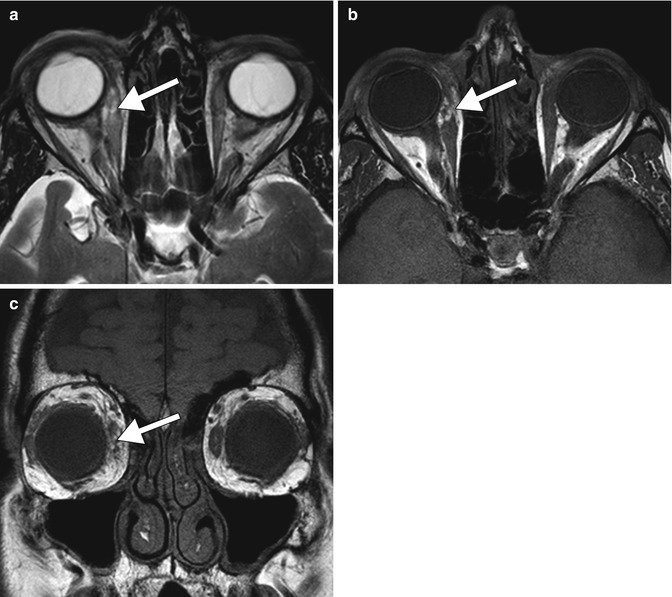
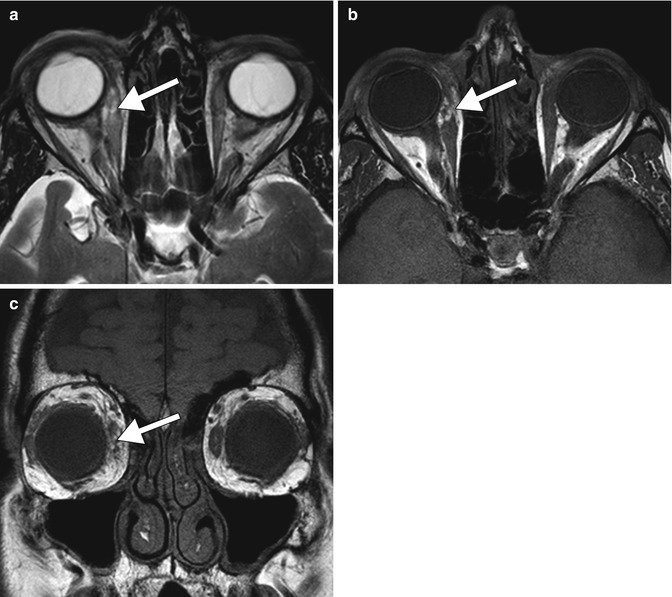
Fig. 6.12
Torn muscle. The patient underwent a recent bilateral medial rectus shortening procedure. Axial T2-weighted (a), axial T1-weighted (b), and coronal T1-weighted (c) MR images show a defect in the belly of the right medial rectus muscle (arrows). The right globe is externally rotated. Both medial rectus muscles are otherwise edematous from recent surgery
Giant conjunctival cyst. Inclusion cysts are rare complications of strabismus surgery that usually occur from months to years after strabismus surgery. The cyst wall is usually composed of non-keratinized epithelial cells. The cysts have a tendency to enlarge over time. Small cysts present as little more than cosmetic deformities. Larger cysts can sometimes become the de facto insertion for the adjacent muscle to the globe; as the cyst enlarges, the insertion of the muscle falls back resulting in a “slipped” or over-recessed muscle. If the extraocular muscle is attached to the cyst rather than directly to the globe “loss” of the muscle may occur during attempted excision of the cyst. Pre-operative imaging can help delineate the relationship of the cyst to the affected extraocular muscle and provide the surgeon with information needed to prevent this complication. On ultrasound biomicroscopy, inclusion cysts appear as well-circumscribed lesions with low internal reflectivity and hyperechoic components. CT and MRI can be useful for evaluating the posterior extension of the cyst. These lesions typically appear as well-defined fluid attenuation ovoid masses on CT and as non-enhancing T1 hypointense and T2 hyperintense on MRI (Fig. 6.13).
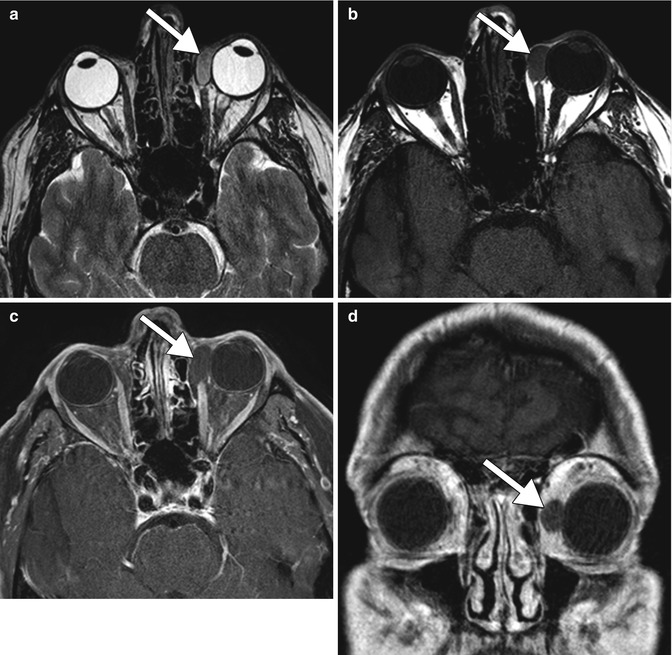
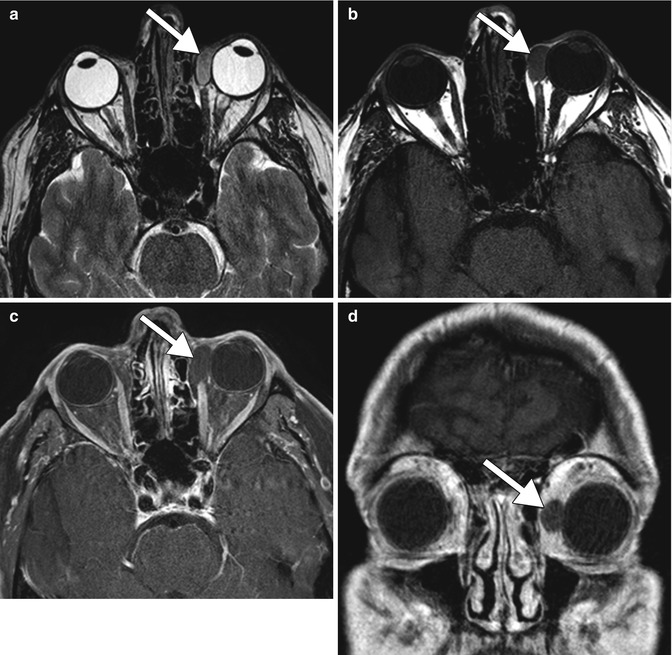
Fig. 6.13
Postoperative conjunctival inclusion cyst. Axial T2-weighted (a), axial T1-weighted (b), axial post-contrast fat-suppressed T1-weighted (c), and coronal post-contrast T1-weighted (d) MR images show an oval fluid-filled lesion (arrows) posteriorly displacing the insertion of the left medial rectus muscle (Adapted with permission from Mehendale et al. (2012))
Acquired Brown syndrome. Brown syndrome is a limitation of elevation in adduction due to an abnormality of the superior oblique tendon sheath complex. This condition can result from superior oblique tuck, or from a cyst or mass in the location of the trochlea. If secondary to a tuck or localized inflammation, thickening of the tendon can be observed on CT or MRI. In particular, abnormal hyperintensity on fat-suppressed T2-weighted sequences and enhancement on post-contrast T1-weighted sequences in and around the superior oblique can be observed on MRI, which is suggestive of an inflammatory process (Fig. 6.14).
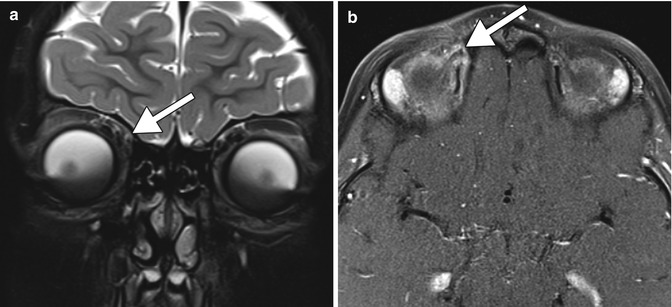
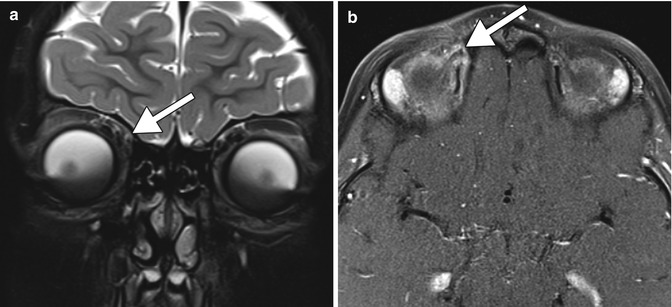
Fig. 6.14
Acquired Brown syndrome. Coronal fat-suppressed T2-weighted (a) and axial fat-suppressed post-contrast T1-weighted (b) MR images show T2 hyperintensity and enhancement involving the right superior oblique tendon (arrows)
6.2 Part II: Orbital Imaging Following Surgery for Craniofacial Malformations
6.2.1 Overview
Craniosynostosis is the premature fusion of sutures in the infant skull. This condition affects 1 in 2,500 births and is syndromic in 15–40 % of cases. Due to the premature fusion the skull acquires an abnormal shape as it grows, and this can potentially restrict cerebral growth and venous or cerebrospinal fluid drainage and a secondary increase in intracranial pressure can ensue. Strabismus occurs in 60–70 % of patients with craniosynostosis. V pattern strabismus is the most common variety. This may be due to excyclorot-ation of the extraocular muscles, aberrant insertions of extraocular muscles, abnormal extraocular muscle development, and anomalous localization of the superior oblique tendon. Furthermore, orbital depth is decreased in some variants, including Apert, Crouzon, and Pfeiffer syndromes, resulting in exorbitism and often more exaggerated strabismus. Endoscopic strip craniectomy is a procedure designed to directly open prematurely fused sutures and is typically performed between 2 and 4 months of age. Direct calvarial vault expansion is usually delayed until 9–12 months of life. There are a variety of procedures included in the category of calvarial vault expansion including orbitofrontal advancement, distraction osteogenesis, and orbital rim augmentation. These surgeries are complex, may be performed in a staged manner, and sometimes include the use of distraction devices. In addition, some affected patients have associated midface hypoplasia or retrusion, which can be addressed via LeFort osteotomy, typically later in childhood. Imaging aids initial assessment by providing detailed information on the degree of premature fusion of the sutures and indicators of possible elevation in intracranial pressure (copper-beaten bone, increased ventricular size, and jugular venous stenosis and emissary vein formation). Imaging can be performed after calvarial expansion to assess the evolution of the calvarial morphology, and to help with pre-operative planning of strabismus surgery by determining the degree of excyclorotation of the involved extraocular muscles and aberrancy in the path of the superior oblique. Otherwise, diagnostic imaging is mainly reserved for the evaluation of suspected postoperative complications or to follow cranial and ventricular growth. Advances in CT post-processing techniques such as iterative reconstruction have enabled scanning patients at a considerably lower dose than via standard CT without compromising image quality. Low-dose CT techniques with high spatial resolution can be useful for delineating the osseous structures, while MRI is suitable for imaging the globe and extraocular muscles. Besides craniosynostosis surgery, imaging may occasionally be performed after frontoethmoid encephalocele repair. The purpose of CT or MRI may be to verify complete reduction of the encephalocele, intactness of the surgical repair, and to evaluate potential complications, such as CSF leakage.
6.2.2 Orbitofrontal Advancement
Orbitofrontal (fronto-orbital) advancement is performed for metopic, unicoronal, or bicoronal synostosis. The procedure essentially consists of bicoronal craniotomy and anterior translation of the reshaped frontal bone and supraorbital bar after completion of lateral orbital wall osteotomies. The procedure reduces or eliminates the prominent frontal ridge at the metopic suture and deepens the orbital cavities (Fig. 6.15). Postoperative volumetric changes in the orbits can be quantified on CT. Orbit expansion does not fully restore normal orbital volume, but is generally effective for mitigating preoperative symptoms, such as exophthalmos, and corneal erosion.
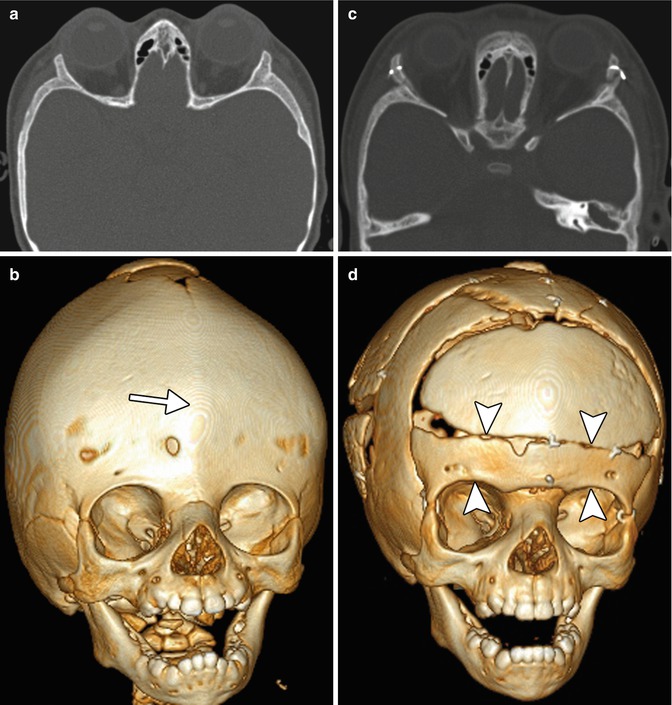
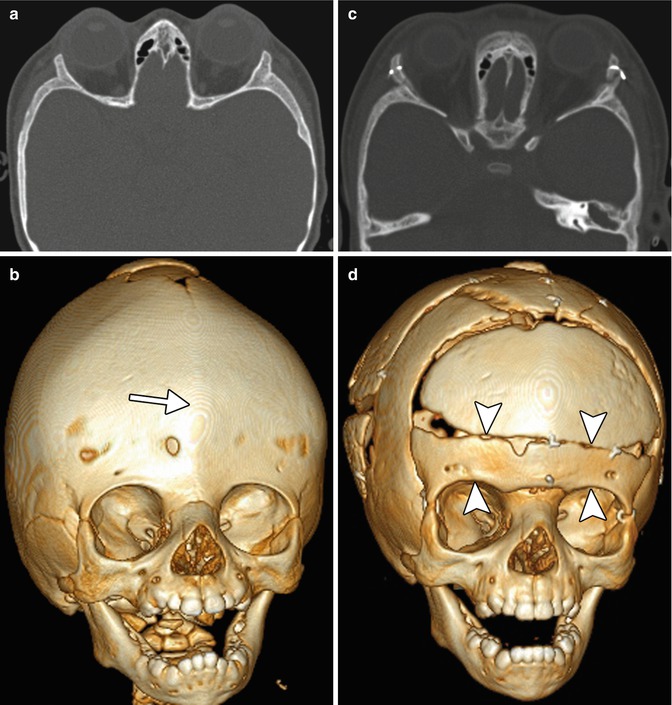
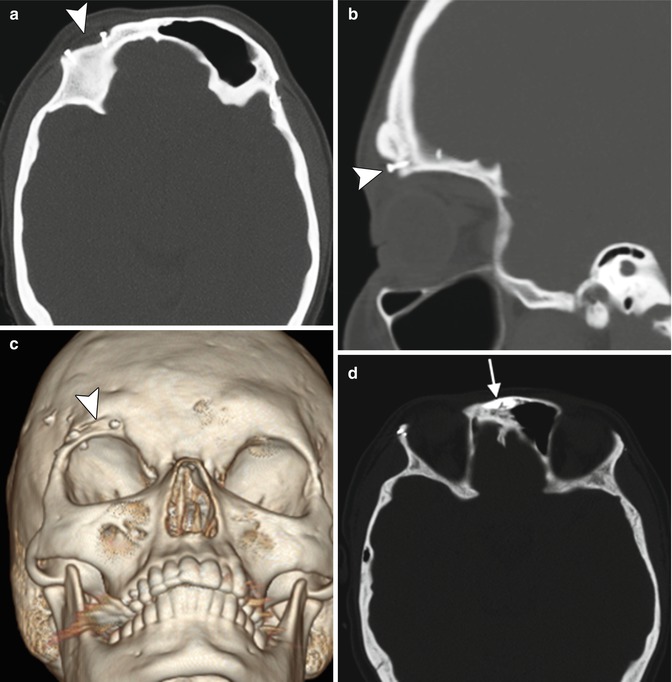
Fig. 6.15
Orbitofrontal advancement. The patient has a history of trigonocephaly. Preoperative axial (a) and 3D volume rendered (b) CT images show metopic synostosis with a prominent frontal ridge (arrow), shallow orbits, and hypotelorism. Postoperative axial (c) and 3D volume rendered CT (d) images show interval improvement of the contours of the frontal calvarium and less shallow orbital cavities with anterior translation of the orbital bandeau (arrowheads)
6.2.3 Barrel Stave Cranial Vault Remodeling
Barrel stave osteotomies can be performed as part of craniosynostosis surgery for the treatment of dolichocephaly and turricephaly. The maneuver consists of creating multiple parallel flexible strips of calvarium that facilitate remodeling of the skull and initially resemble the stave joints of a barrel (Fig. 6.16). Over time, bone forms between the strips of calvarium, which then acquires a new shape.
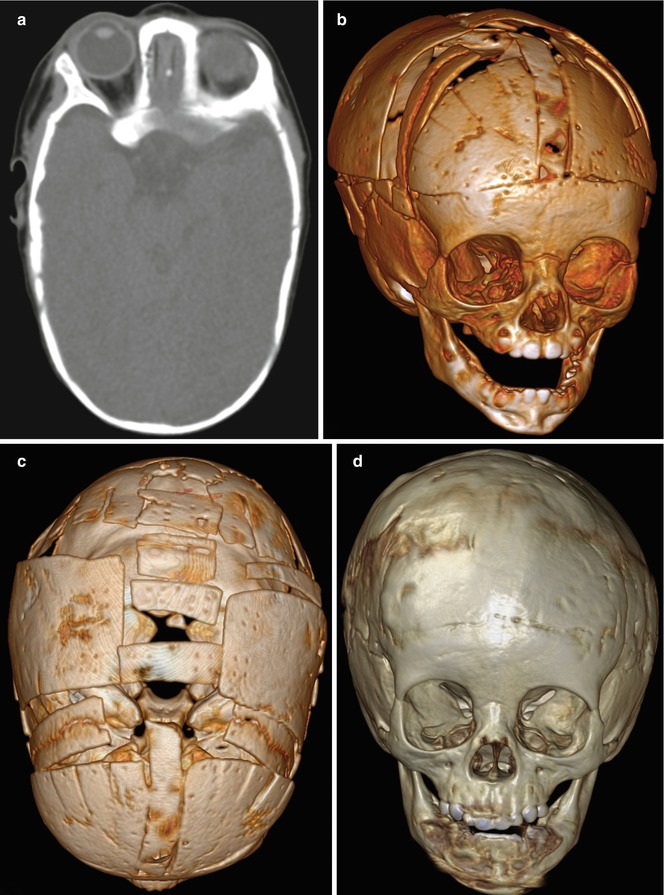
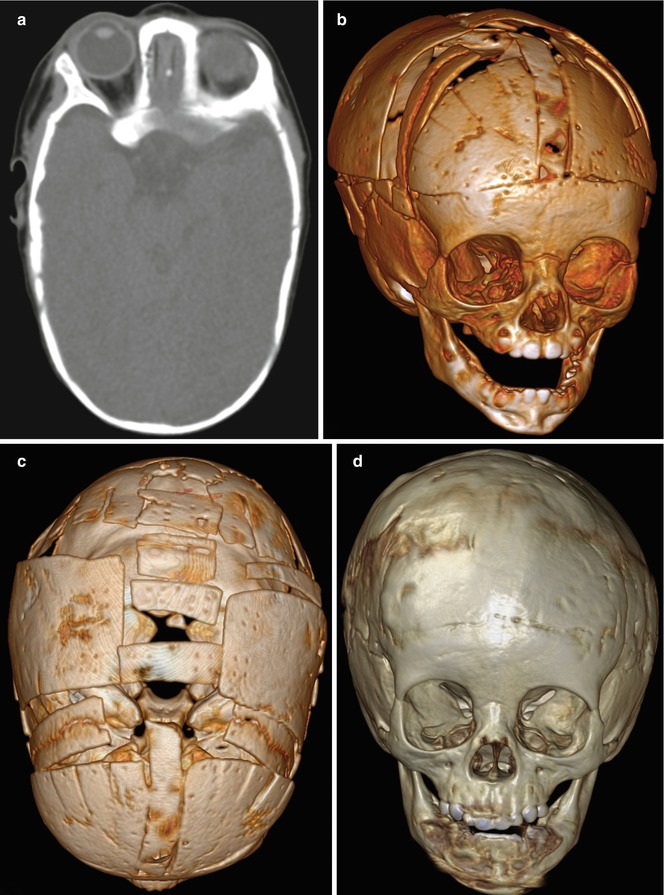
Fig. 6.16
Barrel stave osteotomies. Preoperative axial CT image (a) shows scaphocephaly. Oblique frontal and vertex 3D volume rendered CT images (b, c) show multiple osteotomies and repositioned segments of calvarium. Follow-up frontal 3D volume rendered CT image (d) obtained approximately 1 year later shows expected healing of the osteotomies
6.2.4 Distraction Osteogenesis
Posterior vault expansion using distraction osteogenesis has become a first-line treatment in syndromic craniosynostosis. Indeed, distraction osteogenesis following a monobloc osteotomy has largely superseded traditional grafting and fixation due to the decreased risk of infection and other morbidity. Craniofacial CT with 3D imaging may be obtained during the course of distraction to monitor the progress of the osteogenesis and stability of the distractors (Fig. 6.17).
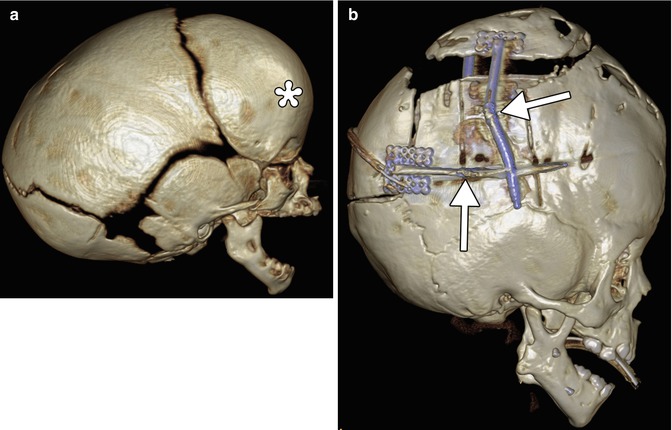
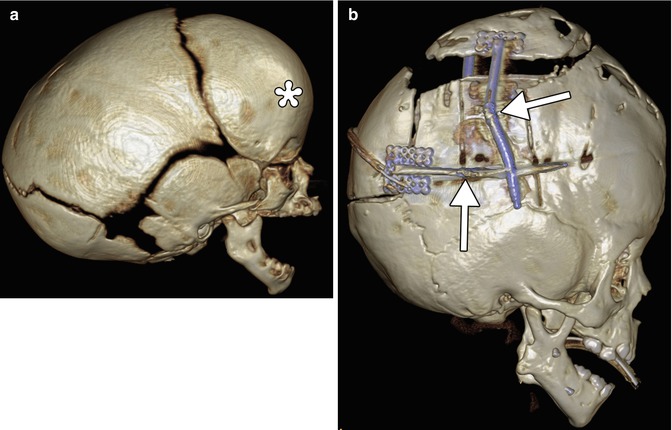
Fig. 6.17
Cranial vault expansion with distraction osteogenesis. Preoperative 3D volume rendered CT (a) shows scaphocephaly with frontal bossing. Postoperative 3D volume rendered CT (b) shows interval osteotomy and application of distraction devices (arrows) to the posterior calvarium. There is improvement in the overall shape of the skull
6.2.5 Periorbital Augmentation
Postoperative depressions in the periorobital region are common following orbital rim advancement and cranial vault remodeling in children. Augmentation of the bony deficiencies can be accomplished using versatile biocompatible materials, such as Medpor and hydroxyapatite. On CT, Medpor appears as low attenuation, while hydroxyapatite appears as high attenuation, similar to cortical bone (Fig. 6.18).