Chapter 12 IMAGING OF THE KNEE
The knee is the largest synovial-lined joint in the body. It has a complex anatomic design that simultaneously allows for the support of the entire weight of the body while providing maximum mobility. The knee is a hinge joint and as such relies heavily on a complex system of soft tissue structures for support and stability. However, several of these structures are particularly vulnerable to injury.
MODALITIES
Radiography
A joint effusion often accompanies internal derangement of the knee and is usually detectable on good-quality radiographs. Detection of a fat-fluid level on a cross-table lateral view indicates a likely intracapsular fracture. Several subtle radiographic abnormalities can be indicators of significant internal derangement. For instance, the Segond fracture (lateral capsular avulsion fracture of the tibia; see Fig. 12-8A) and the deep lateral femoral sulcus sign (see Fig. 12-9A) indicate likely anterior cruciate ligament disruption. A small avulsion fracture of the lower pole of the medial patellar facet can be seen after transient dislocation of the patella and may necessitate followup MRI to delineate the extent of associated soft tissue abnormalities. Radiographs are also very useful for evaluating suspected arthritis, monitoring healing of fractures, and evaluating potential hardware complications after arthroplasty.
Computed Tomography
Multidetector CT with its ability to provide highresolution reconstructed images in any plane has proved very useful in evaluation of the knee. This modality is most commonly used to accurately depict the location and extent of fractures, including a precise determination of articular incongruity, particularly as it pertains to fractures of the tibial plateau (see Fig. 12-67). The high-resolution multiplanar capability is also ideal for evaluating the status of a healing fracture and is useful for detecting signs of early healing versus nonunion. This can be particularly helpful in evaluating fractures about the knee and the tibial shaft, where fracture nonunion or delayed union is a common complication. Multidetector CT is also very useful for evaluating prosthesis of the knee following arthroplasty for complications such as loosening, infection, and osteolysis. Finally, multidetector CT combined with intra-articular contrast is proving to be very useful in the evaluation of internal derangement, especially in patients who are not able to undergo MRI because of implanted devices such as a pacemaker.
Ultrasound
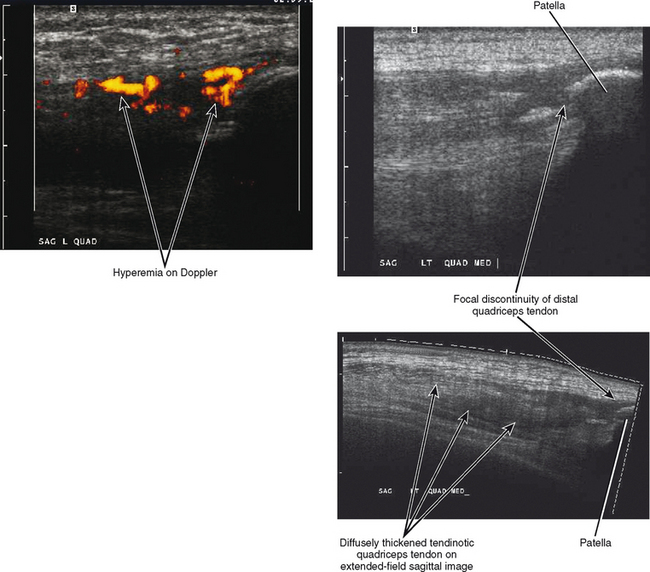
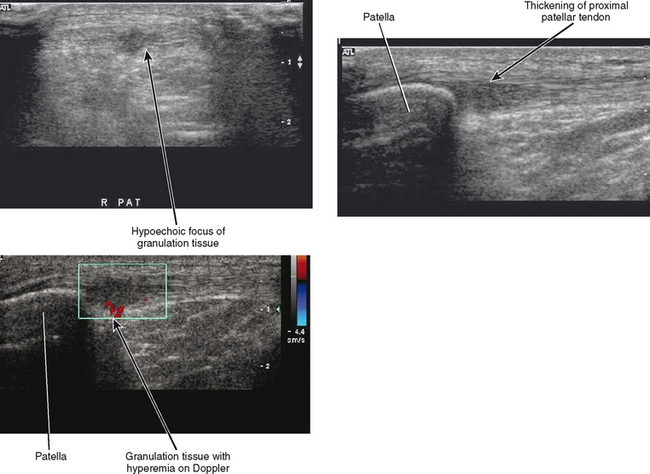
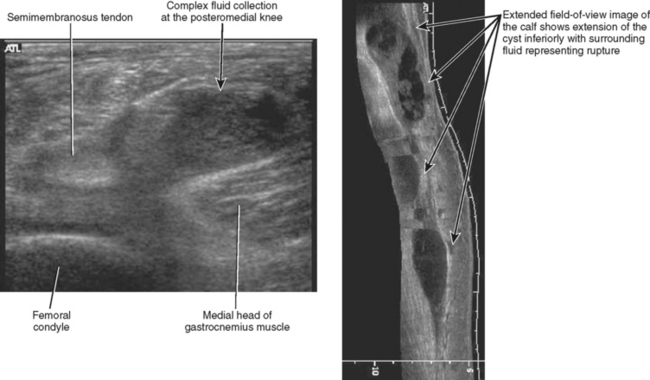
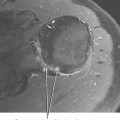
Ultrasound has only limited usefulness with regard to evaluation of the knee. A few studies have demonstrated the appearance of meniscal tears using ultrasound examination; however, only the peripheral portions of the menisci are typically visualized. MRI remains the modality of choice in evaluation of the menisci primarily because of its increased accuracy and ability to provide more global evaluation of the knee. Ultrasound can accurately depict and classify abnormalities of the collateral ligaments as well as the quadriceps (Fig. 12-1) and patellar tendons (Fig. 12-2) and can be useful in a targeted evaluation of these structures, but it is incapable of accurately assessing the anterior or posterior cruciate ligaments. The osseous structures and articular surfaces cannot be adequately evaluated with ultrasound. Probably one of the more common uses of ultrasound with regard to imaging of the knee is to confirm a Baker’s cyst, which appears as an anechoic structure along the posterior medial aspect of the knee arising between the medial head of the gastrocnemius and the semimembranosus tendons (Fig. 12-3). The presence of a Baker’s cyst has been shown to be associated with an increased incidence of internal derangement of the knee; as a result, MRI may again be the study of choice for providing a more global assessment of the knee with regard to the presence of a Baker’s cyst.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is the modality of choice for evaluating the soft tissue structures of the knee, and indeed the knee is the most commonly imaged joint using MRI. MRI accurately depicts abnormalities of the osseous structures and articular cartilage along with all of the soft tissue structures, including the tendons, ligament, and menisci. Direct or indirect MR arthrography is typically reserved for postoperative cases to aid in differentiating postsurgical change from recurrent meniscal tears, but contrast can also be helpful in grading osteochondral lesions and in detecting intra-articular bodies. Intravenous gadolinium may be helpful in selected cases in differentiating solid from cystic lesions and in evaluating soft tissue masses and suspected infection.
LIGAMENTS
Cruciate Ligaments
Anterior Cruciate Ligament
The anterior cruciate ligament (ACL) is an intra-articular, extrasynovial structure that is lined by its own synovial sheath separating it from the joint space. It is composed of two discrete bundles—the larger posterolateral bundle and the smaller anteromedial bundle—named for their insertion sites on the tibia. The ACL arises proximally from the intercondylar notch of the lateral femoral condyle and inserts distally on the tibial plateau adjacent to the anterior tibial spine. The ACL broadens at both attachment sites to a thickness approximately three times the cross-sectional diameter of the midsubstance of the ligament. The ACL receives its blood supply via a periligamentous plexus contained within the synovial lining of the ligament. Disruption of the periligamentous plexus is primarily responsible for the hemarthrosis that occurs with acute ACL disruption.
The Lachman test is used clinically to evaluate the status of the ACL. With the patient in the supine position, the test is performed by flexing the knee 20 to 30 degrees and then applying anterior force to the proximal tibia while the femur is stabilized with the opposite hand. The extent of translation of the proximal tibia along with the firmness of the “end point” determines the status of the ACL. Anterior translation of the tibia combined with the lack of a firm end point is the hallmark of a disrupted ACL. As an adjunct to the Lachman test, a variety of devices known as arthrometers (most commonly the KT1000) can provide an objective measurement of the amount of anterior tibial translation. The role of MRI therefore is to confirm the presence of a suspected ACL injury, to differentiate partial from complete tear, to further define the extent and location of injury as a guide to surgical planning, and finally to detect the presence of associated injuries, including meniscal pathology, articular cartilage injury, and other ligamentous injuries (Box 12-1).
BOX 12-1 ROLE OF MRI IN THE EVALUATION OF ANTERIOR CRUCIATE LIGAMENT (ACL) INJURY
Normal MR Appearance of the ACL
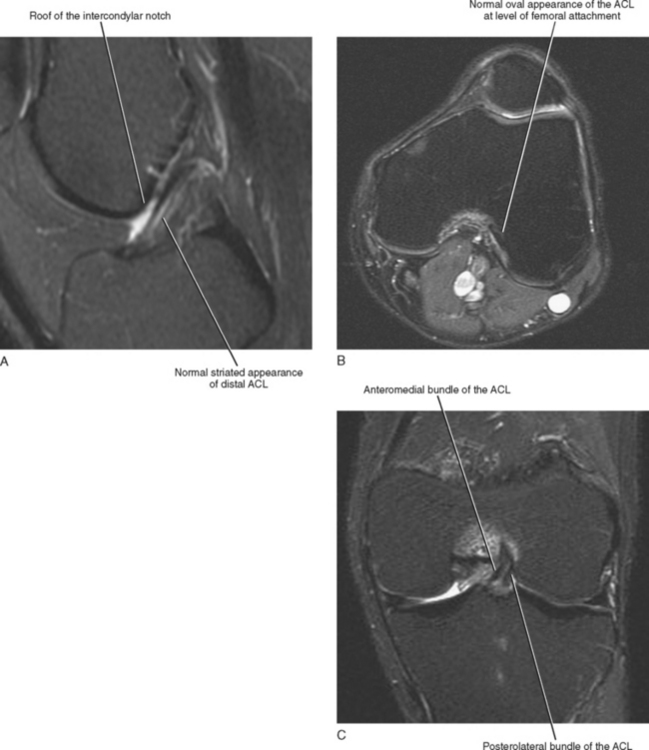
The primary evaluation of the ACL is routinely performed using T2-weighted sagittal images. The ACL originates on the intercondylar notch cortex of the lateral femoral condyle and traverses the intercondylar notch to insert onto the tibial plateau. The anteromedial bundle inserts onto the medial tibial spine, whereas the posterolateral bundle inserts between the spines. The proximal ACL demonstrates homogeneous low signal intensity within the substance of the ligament, whereas distally the ligament takes on a more striated appearance with fat and synovium interspersed between the anteromedial and posterolateral bundles as they fan out near their attachment to the tibial plateau. This appearance should not be misinterpreted as a tear (Fig. 12-4A). With the knee in full extension, the course of the normal ligament is usually straight but may demonstrate minimal posterior bowing. With the knee in full extension, the ACL should parallel but not touch the roof of the intercondylar notch (Blumensaat’s line). Visualization of both bundles from their origin to insertion indicates an intact ligament.
During evaluation of the ACL in the sagittal imaging plane, partial volume averaging of the proximal fibers of the ACL with the adjacent lateral femoral condyle often limits evaluation of the femoral attachment. The proximal attachment site of the ACL is a common location for injury, and routine evaluation of the ACL should always include assessment of the femoral attachment site on both the axial and coronal images. A hurried evaluation of the ACL using only the sagittal imaging plane will undoubtedly result in the occasional embarrassment of a missed proximal ACL tear that is readily apparent on both the coronal and axial imaging planes. Axial images are especially helpful in the evaluation of the femoral attachment site (Fig. 12-4B), whereas the coronal images are complementary in the evaluation of both the femoral and tibial attachments of the ACL (Fig. 12-4C). During our early experience with MRI of the knee, it was often stated that oblique or “tilted” sagittal images were necessary to optimize evaluation of the ACL. However, the proper use of axial and coronal images provides for an adequate evaluation of the ACL, and oblique images are not necessary.
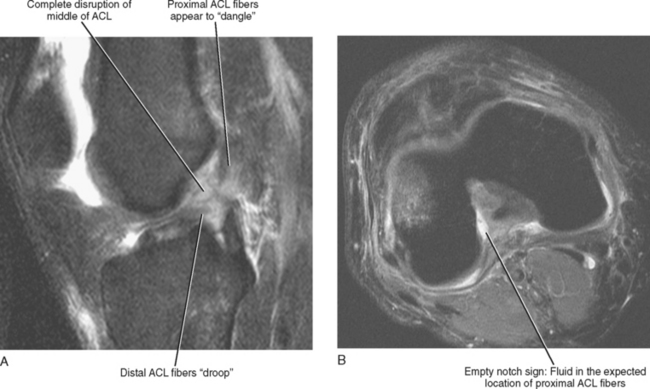
Direct MRI Signs of ACL Disruption
For detection of ACL disruption, MRI is more than 95% sensitive with an overall accuracy ranging between 90% and 95%. There are several direct signs of injury that are very helpful in the evaluation of the ACL (Box 12-2). The most important sign is complete disruption or discontinuity of the fibers. In the acute injury, disruption of the ACL is often associated with thickening, hemorrhage, edema, and distortion of the adjacent fibers. Complete disruption most often occurs in the middle of the ACL and often leads to an abnormal slope (Fig. 12-5A) or posterior bowing of the distal fibers. The proximal fibers appear to “dangle” from the femoral notch while the distal fibers “droop” inferiorly and no longer parallel Blumensaat’s line.
A complete evaluation of the ACL must also include an assessment of the tibial and femoral attachment sites. The proximal ACL is the second most common site of injury, and a femoral avulsion injury may result in little or no morphologic change in the appearance of the ACL with the exception of the droop. Fluid signal may be seen at the normal ACL attachment site on either axial or coronal images, and this is referred to as the empty notch sign (Fig. 12-5B).
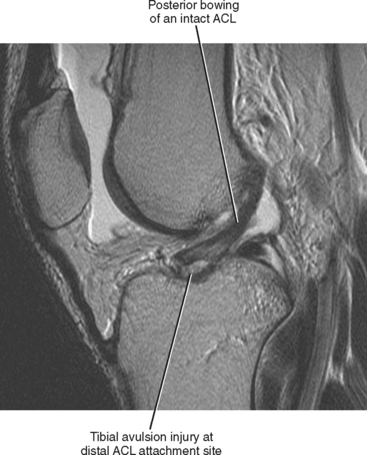
Avulsion of the ACL at its distal attachment site usually results in a small osseous fragment that is best visualized on non–fat-saturated sagittal images (Fig. 12-6). The ACL may demonstrate normal morphology but often shows posterior bowing, so if one evaluates only the ACL and not the adjacent tibia, the avulsion fracture can easily be missed. In addition, tibial edema associated with an avulsion fracture is usually minimal, so one’s eye is not drawn to this area when evaluating the osseous structures. It is therefore important to specifically evaluate the osseous attachment of the ACL to exclude a tibial avulsion injury. Tibial avulsion injuries of the ACL, though initially reported in adolescent patients, have more recently been described in adult skiers. It is important to accurately detect both femoral and tibial avulsion injuries and to describe the status of the adjacent ligament because these injuries can often be repaired with a direct primary reattachment of the ligament proximally or by reattachment of the bone fragment distally rather than necessitating a graft reconstruction, as required with midsubstance tears.
Indirect MRI Signs of ACL Disruption
In most instances, the direct MRI signs of ACL disruption are conclusive. However, occasionally the status of the ACL is equivocal on the basis of these direct MRI signs. This is more likely to be true if the images are suboptimal because of patient motion or if the images are obtained on a low field strength magnet or with suboptimal technique. Also, it is occasionally difficult to differentiate a partial-thickness tear or sprain from a complete ACL disruption. In these instances, indirect signs can be especially helpful and can increase the level of confidence in diagnosing ACL disruption (Table 12-1). Most indirect MRI signs are related to osseous abnormalities that occur at the time of acute ACL injury.
Table 12-1 Indirect Signs of ACL Disruption
| Specific for ACL disruption | Bone marrow edema sign: lateral femoral condyle and posterolateral tibial plateau (pivot shift injury) |
ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
The pivot shift mechanism of injury is one of the most common mechanisms resulting in disruption of the ACL. It is a low-energy noncontact injury that commonly occurs in athletes and is particularly common among American football players and skiers. The injury typically occurs when a valgus load is applied to the knee while the knee is in various states of flexion. At the same time, internal rotation of the tibia or external rotation of the femur takes place while the foot is planted against the ground. This type of injury occurs during maneuvers such as rapid deceleration combined with simultaneous change of direction. These maneuvers load the ACL and can result in its rupture. Once the ACL tears, it allows the tibia to translate anteriorly relative to the femur, and during this first phase of translation the resulting impaction of the tibia against the femur gives rise to the bone bruise pattern described as the “pivot shift” marrow edema pattern (lateral femoral condyle and posterolateral tibial plateau) (Fig. 12-7). The exact location of the bone bruise on the lateral femoral condyle depends on the degree of flexion of the knee at the time of injury. Greater flexion results in a bone bruise located more posteriorly within the femoral condyle, whereas less flexion results in a more anteriorly located bone bruise.
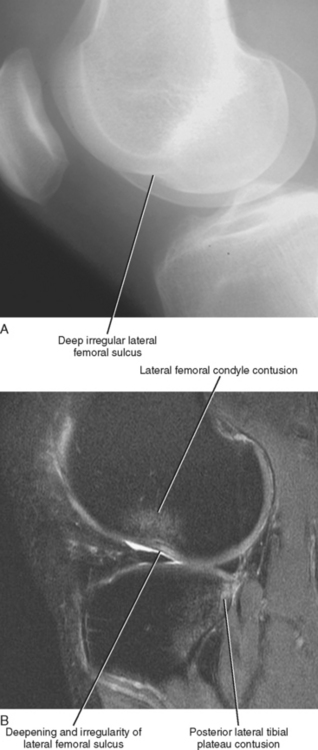
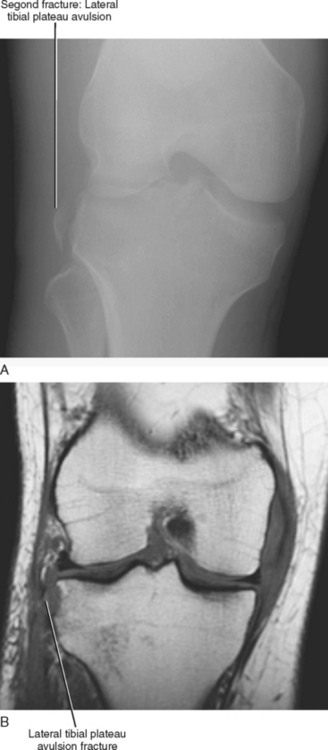
Excessive compressive forces at the time of impaction injury can also lead to an osteochondral impaction fracture of the lateral femoral condyle, referred to as the deep notch or deep femoral sulcus sign of the lateral femoral condyle (Fig. 12-8). This results in an irregular contour of the articular surface of the lateral femoral and deepening of the lateral femoral sulcus, often associated with underlying marrow edema. An impaction injury of the posterior lip of the lateral tibial plateau can also result in a depressed fracture of the posterior articular surface of the tibia. The same mechanism of rotational forces and anterior translation of the tibia can cause a capsular avulsion of the lateral tibial plateau referred to as the Segond fracture (Fig. 12-9). These three injuries all result from abnormal forces at the time of anterior tibial translation. In an adult, the tibia can only translate anteriorly if the ACL is torn. Therefore, these signs (i.e., bone contusions) are specific for ACL disruption and, when present, can be very helpful in confirming the presence of an ACL tear on MRI. There have been reports of the pivot shift bone contusion pattern occurring in children with an intact ACL, and this is thought to be possible because of the increased laxity of the ACL during childhood, which allows anterior translation of the tibia in the face of an intact ACL.
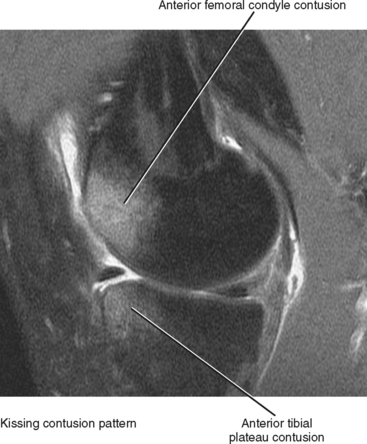
Another bone bruise pattern that has been associated with ACL disruption is the kissing contusion pattern (Fig. 12-10). This pattern of injury results from impaction of the anterior tibia against the anterior femur and occurs during a hyperextension injury and is less specific for ACL disruption. It can result in an isolated tear of either the ACL or posterior cruciate ligament (PCL) or a combination injury involving both ligaments. Hyperextension of the knee can also result in extensive soft tissue injury of the posterior medial or lateral capsular structures as well as injury to the posterior neurovascular structures. A combination ACL and PCL injury may indicate previous dislocation or severe hyperextension injury, and the posterior vascular structures should be closely evaluated for evidence of injury. Other less specific signs associated with ACL injury include the anterior drawer sign, buckling of the PCL, and acute hemarthrosis.
Detection of a chronic ACL disruption on MRI is more difficult because the ACL fibers lack the typical edema and thickening that is seen after an acute injury. In addition, most of the indirect signs that are present at the time of acute injury are absent in chronic tears. As a result, MRI is slightly less accurate in the detection of a chronic ACL disruption. Nonvisualization of the ACL in both the sagittal and coronal imaging planes in the absence of edema is a sign of chronic ACL disruption. More commonly, residual fibers are present but demonstrate abnormal morphology (thinning and attenuation) or an abnormal posterior slope. Occasionally, the proximal fibers of the torn ACL scar to the PCL and maintain a relatively normal slope or demonstrate only subtle posterior bowing. In these instances, the empty notch sign may be helpful in detecting a chronic proximal disruption (see Fig. 12-5B). Other MRI findings that may indicate a chronic ACL disruption include the posterior drawer sign and an old deepened lateral femoral sulcus with no underlying marrow edema.
A partial-thickness tear or sprain may occasionally mimic a complete tear of the ACL. With a partial-thickness tear, there may be fluid signal within the fibers of the ACL, but some fibers remain intact throughout the normal course of the ligament. It is also possible to tear a single bundle of the ACL and see the second bundle intact. If this occurs proximally, the femoral attachment of the ACL demonstrates a round rather than oval appearance on the axial images since one of the bundles will be absent (Fig. 12-11). Typically with a sprain or partial-thickness tear, the secondary signs of injury are absent.
Posterior Cruciate Ligament
Normal MRI Appearance of the PCL
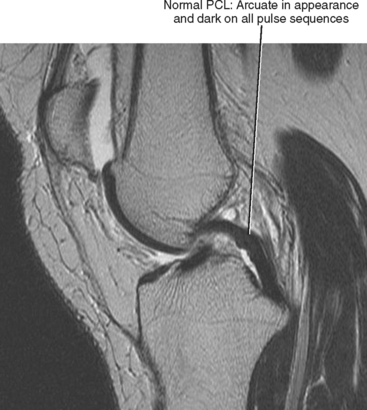
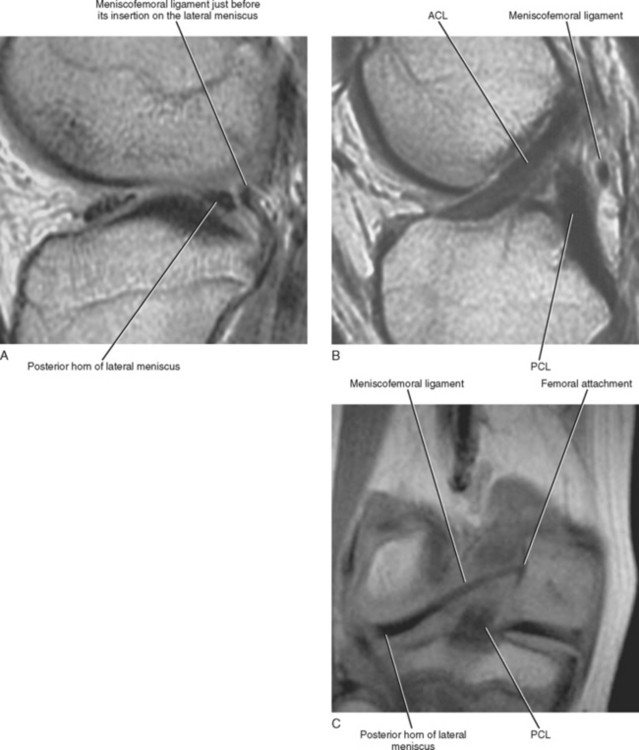
The PCL is best evaluated on T2-weighted sagittal images of the knee, and although coronal and axial images are complementary, they are rarely necessary to establish the diagnosis of a PCL injury. The PCL is usually visualized in its entirety on one or, at most, two consecutive sagittal images. The PCL is roughly two times the thickness of the ACL, and unlike the ACL typically appears uniformly dark on all pulse sequences. Occasionally, the separate PCL bundles can be seen on MR imaging, giving the PCL a striated appearance, or, on the other hand, intrasubstance degeneration results in intrinsic signal alteration in an intact PCL. With the knee in full extension, the PCL demonstrates an arcuate or curved appearance (Fig. 12-12). The meniscofemoral component of the PCL is best visualized on sagittal or coronal images and can be seen as a small bandlike structure coursing either anterior (Humphry) or posterior (Wrisberg) to the PCL and extending from the posterior horn of the lateral meniscus to attach on the inner aspect of the medial femoral condyle (Fig. 12-13).
Direct MRI Signs of PCL Disruption
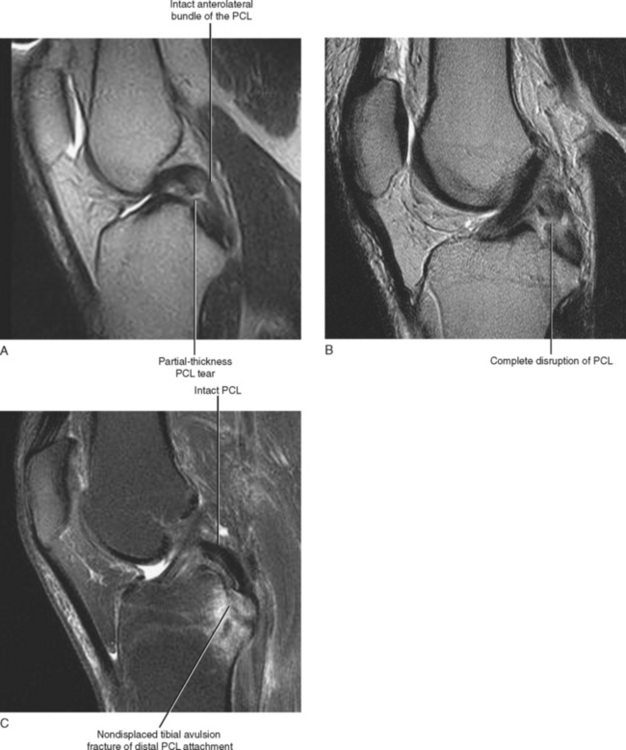
Most PCL injuries are partial-thickness tears or sprains that involve the posteromedial bundle. MR imaging demonstrates fluid signal partially traversing the PCL with an intact anterolateral bundle (Fig. 12-14A). Complete disruption of the PCL most frequently occurs in the middle of the ligament and in the acute setting demonstrates high T2-weighted signal completely traversing the ligament with discontinuity of the fibers (Fig. 12-14B; Table 12-2). Avulsion injuries of the PCL can occur at either the femoral or the tibial attachment site, but most frequently on the tibial side. They are often associated with a large nondisplaced fracture fragment of the posterior tibial plateau and adjacent marrow edema (Fig. 12-14C). An avulsion injury of the PCL at the femoral attachment site has been referred to as a peel-off injury and sometimes results in a small fleck of bone being pulled off the femur. Avulsion injuries are important to differentiate from midsubstance tears because they are treated differently. Large tibial avulsion fractures are often treated conservatively if the fracture fragment is not significantly displaced, or, if necessary, the fracture fragment can be reduced and fixed. Primary repair of the PCL may be possible following a peel-off injury at the femoral attachment site. Midsubstance tears require reconstruction with a graft since attempted primary repairs of these tears are usually unsuccessful.
Table 12-2 Direct Signs of PCL Injury
| Imaging Finding | PCL Injury |
|---|---|
| Discontinuity of fibers (fluid signal completely traversing fibers) | Complete tear: Most common in midsubstance |
| Fluid signal partially traversing ligament | Partial-thickness tear: Most commonly involves posteromedial bundle |
| Large fracture fragment with edema: PF or MRI | Avulsion of tibial attachment site |
| Tiny avulsion fragment: PF or MRI | Femoral peel-off injury |
| Absent PCL fibers or may scar down and appear intact on MRI | Chronic PCL disruption |
MRI, magnetic resonance imaging; PCL, posterior cruciate ligament; PF, plain film radiography.
Indirect MRI Signs of PCL Disruption
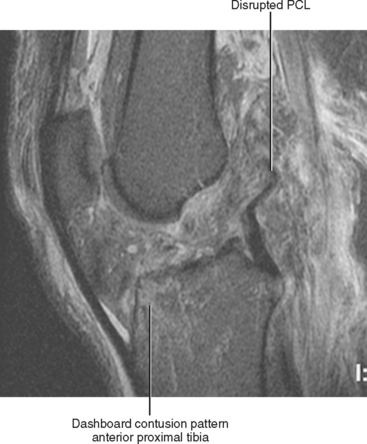
As with ACL injuries, most secondary imaging signs associated with PCL injuries represent osseous abnormalities that occur at the time of injury (Table 12-3). The dashboard mechanism of injury can lead to a bone contusion pattern that is isolated to the anterior aspect of the proximal tibia (Fig. 12-15). This pattern of marrow edema has a high association with PCL injury, and it results from a direct impact of the bone against the dashboard or against the ground if secondary to a fall. The kissing contusion pattern (described previously in the section, Indirect MRI Signs of ACL Disruption) may also be seen in association with PCL injuries resulting from a hyperextension of the knee (see Fig. 12-10). Other osseous abnormalities that have been associated with PCL injury include avulsions of the tibial or femoral attachments of the PCL, often visible on radiographs and on MRI. Avulsion fractures of the fibular head, Gerdy’s tubercle, and a medial capsular avulsion injury have also been described as potential secondary signs that can be associated with PCL injury.
Table 12-3 Indirect MRI Signs of PCL Injury
| Osseous Abnormality | Mechanism of Injury |
|---|---|
| Dashboard bone contusion pattern | Results from direct impaction injury to anterior aspect of the proximal tibia |
| Kissing bone contusions | Hyperextension injury |
| Fibular head avulsion fracture | Avulsion of conjoined tendon |
| Gerdy’s tubercle avulsion | Avulsion of iliotibial band |
| Medial Segond fracture | Avulsion of medial capsular structures |
Miscellaneous Abnormalities of the Cruciate Ligaments
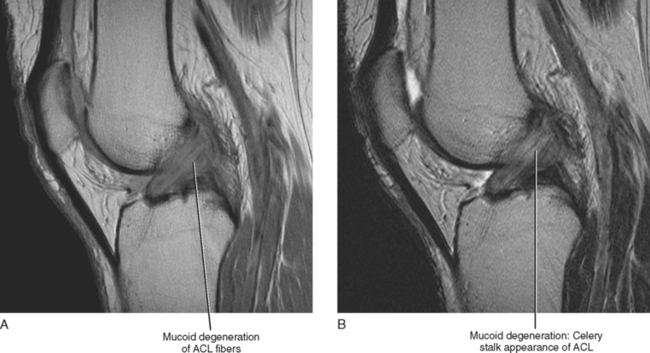
Mucoid degeneration of the cruciate ligaments is a common finding in the older patient population with osteoarthritis but it can also occur in the younger population as isolated mucoid degeneration. Mucoid degeneration is often mistaken for disruption or a partial-thickness tear of the ACL or PCL. It is not associated with instability of the knee. Histologically, the cruciate ligaments demonstrate distortion of the collagen fibers, multifocal mucoid degeneration, and mutilocular fibrous-walled cysts. This entity appears to be on a continuum with cruciate ganglion cysts, which are described in further detail in the text that follows. On MRI, the ligaments demonstrate an ill-defined appearance with increased girth compared with the normal ligament (Fig. 12-16). There is typically intermediate signal intensity within the substance of the ligament on all pulse sequences. The fibers of the cruciate ligament are usually well visualized and run in the normal orientation but are splayed, revealing what has been described as a “celery stalk” appearance. Mucoid degeneration can also result in reactive marrow edema, erosion, or subchondral cyst formation of the adjacent tibia or femur. The key to differentiating mucoid degeneration from a cruciate tear is that the fibers of the ligament are continuous, demonstrate a normal orientation, and are splayed rather than disrupted. With mucoid degeneration, both bundles of the ACL can usually be identified, whereas with an old partial-thickness tear the bundles may be nonvisualized or indistinct.
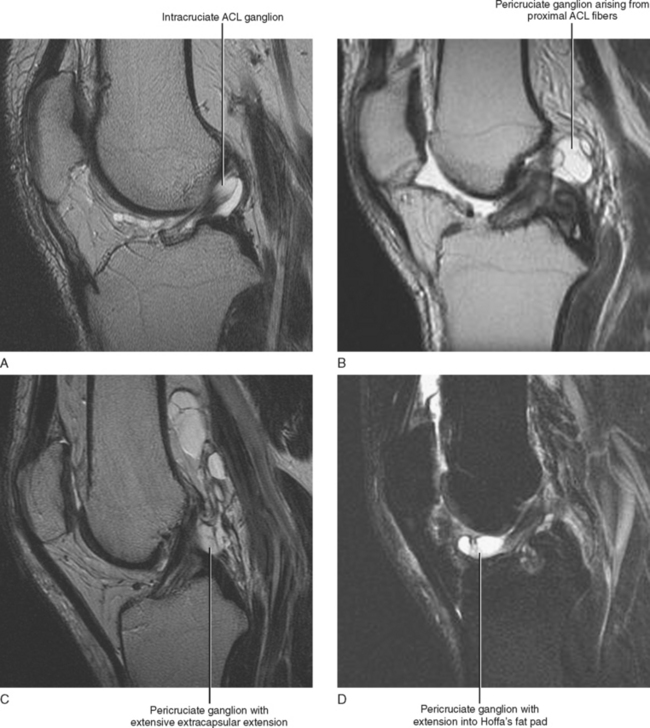
As previously described, the cruciate ligaments are enveloped within a synovial fold; as a result, ganglia formation can occur on either the surface or within the substance of the ACL or PCL (Fig. 12-17). Cysts that arise within the substance of the ligament demonstrate an MR appearance similar to that of mucoid degeneration with increased girth of the ligament and splaying of the fibers. Intracruciate ganglia, however, demonstrate more sharply demarcated T2-weighted signal with characteristic cyst morphology. Cruciate ganglia that arise on the surface of the ligament are referred to as pericruciate ganglia and can become large and extend into various recesses about the knee. They can extend into Hoffa’s fat pad anteriorly or dissect along the posterior horn of either the medial or lateral meniscus posteriorly. On occasion, they may even penetrate the joint capsule posteriorly or erode into adjacent bone.
The ganglia are well defined, septated, oval, or lobular, and they follow water signal on all pulse sequences. Ganglia can be differentiated from fluid within a recess of the knee because there is typically a fluid collection separate from the rest of the joint fluid, and they can result in mass effect on the adjacent structures. Ganglia are often incidentally identified on MRI exams performed for other reasons. However, if they are large enough, they may cause symptoms of catching, locking, and pain. Ganglia arising within the substance of the ligament may mimic a tear, whereas those arising on the surface of the ligament may mimic a meniscal cyst. Pericruciate ganglia can be particularly difficult to distinguish from meniscal cysts arising from the anterior horn of the lateral meniscus and adjacent to the posterior horn of the medial meniscus. Clear depiction of a horizontal cleavage tear of the adjacent meniscus with extension of the tear into the cyst is diagnostic of a meniscal cyst rather than a cruciate ganglion. The absence of an adjacent meniscal tear would be more supportive of the diagnosis of a pericruciate ganglion.
MEDIAL SOFT TISSUES OF THE KNEE
Historically, anatomic descriptions of the medial soft tissue support structures of the knee have been oversimplified in MRI literature. Over the past few years, however, the orthopedic community has begun to gain a more thorough understanding of the role of several of the specific soft tissue structures of the medial aspect of the knee and to better understand the importance of their repair when attempting to maximize surgical outcomes after injury. No longer is it adequate for the radiologist to collectively refer to the anteromedial soft tissue support structures as the medial retinaculum or to collectively refer to the medial support structures of the knee as the medial collateral ligament. Increasingly, the surgeon wants to know the status of a specific soft tissue structure such as the medial patellofemoral ligament, the meniscotibial ligament, or the capsular arm of the semimembranosus tendon. The radiologist should possess a detailed knowledge of the anatomy of the medial soft tissues structures of the knee, have an understanding of the specific injury patterns that involve these structures, and finally should be able to recognize the MRI appearance of these specific injuries.
Medial Soft Tissue Anatomy
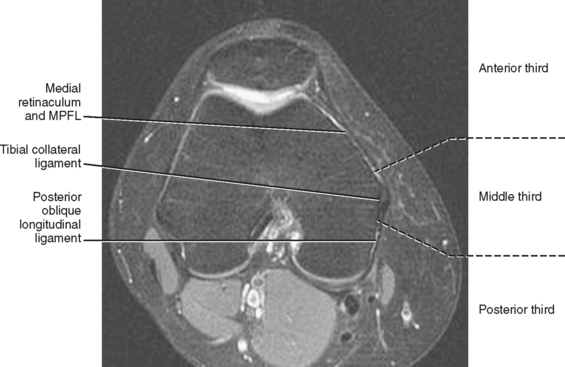
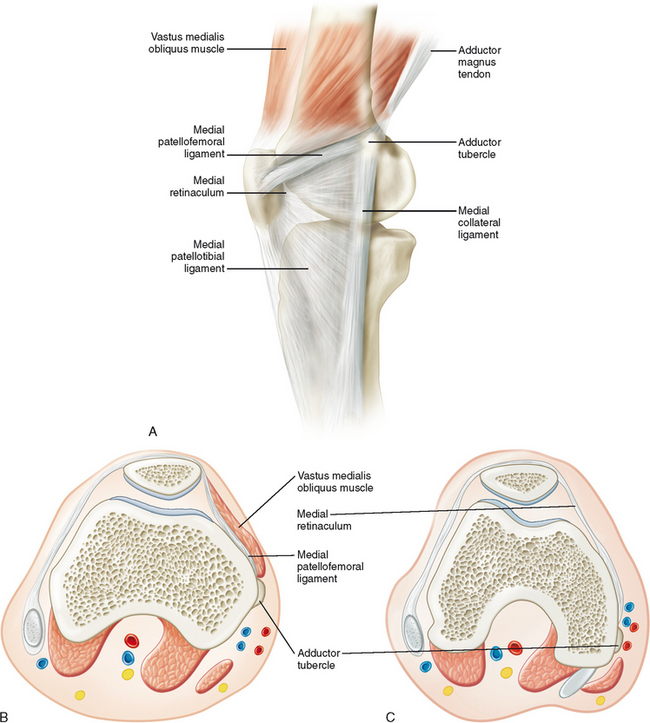
For the purposes of better understanding the anatomy of layers 2 and 3, it is helpful to divide the medial aspect of the knee into anterior, middle, and posterior thirds (Fig. 12-18). A thorough knowledge of the anatomy in each compartment allows the radiologist to accurately describe injuries that are currently of clinical importance to the orthopedic surgeon and it also builds a foundation for the radiologist to expand descriptions of injuries as surgical techniques evolve and additional structures become clinically and surgically relevant.
Anterior Third Anatomy
In the anterior aspect of the knee, layers 2 and 3 cannot be clearly differentiated because they fuse anteriorly to form the medial soft tissue restraint of the patella. The anterior medial soft tissue restraint of the patella is composed of four distinct structures. These include the medial patellofemoral ligament (MPFL), the medial parapatellar retinaculum, the medial patellotibial ligament, and the medial patellomeniscal ligament. The MPFL is the most important of these four structures regarding stabilization of the patella. Although it varies in size and thickness, it remains constant in location. The MPFL originates on the adductor tubercle proximal to the origin of the superficial fibers of the medial collateral ligament and then extends distally to insert on the undersurface of the vastus medialis obliquus (VMO) muscle and on the medial aspect of the upper pole of the patella. The parapatellar or “medial” retinaculum originates as a condensation of the fascia and aponeurosis of the VMO muscle and inserts onto the middle third of the medial aspect of the patella. It allows the VMO muscle to insert directly onto the medial aspect of the patella, thereby allowing the VMO muscle to serve as an active stabilizer of the patella. The patellotibial ligament arises from the tibia near the distal attachments of the gracilis and semitendinosus tendons and then courses cephalad to insert onto the medial aspect of the lower pole of the patella. Finally, the patellomeniscal ligament lies deep to the patellotibial ligament running in a similar direction and plane but inserting onto the meniscus rather than the tibia. Some consider this to be a separate ligament, and others consider this structure to be a deep component of the patellotibial ligament.
Injury Patterns of the Anterior Third of the Medial Soft Tissue Structures (MPFL)
Why does any of this anatomy matter? I have always referred to these structures collectively as the medial retinaculum, and no one has ever challenged me. Is there a clinical reason to be more specific when describing these structures, and, if so, how can I differentiate them on MRI? The answer is yes. The MPFL has been shown to be the most important soft tissue stabilizer preventing lateral subluxation of the patella (Table 12-4). It provides most of the restraining force, whereas the other three structures provide minimal restraint toward the prevention of lateral patellar subluxation. Many orthopedic surgeons now repair a torn MPFL to minimize the rate of recurrence of patellar dislocation, whereas disruption of the other three structures does not routinely warrant surgical repair. It is therefore important to comment specifically on the integrity of the MPFL after transient dislocation of the patella and to distinguish between a tear of the MPFL and a tear of the parapatellar or “medial” retinaculum (Table 12-5).
Table 12-4 Anatomy of the Medial Patellofemoral Ligament
| Origin | Adductor tubercle of medial femoral condyle |
| Insertion | Superior pole of patella |
| Location on axial MRI | Sits deep to the vastus medialis obliquus muscle |
| Function | Primary stabilizer of patella (prevents lateral subluxation) |
| Injury location | |
| Mechanism of injury | Lateral patellar dislocation |
Table 12-5 MRI Findings after Transient Lateral Dislocation of the Patella
| Bone contusion pattern | |
| Articular surfaces | |
| Medial soft tissue restraint injuries | |
| Miscellaneous | Joint effusion |
MPFL, medial patellofemoral ligament.
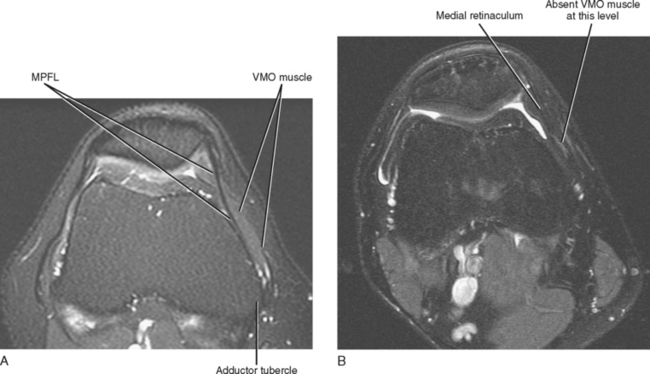
The MPFL and the medial retinaculum are best depicted on axial MR images and are simple to differentiate from one another. These two structures are located at the same depth; however, the MPFL is a more proximal structure. The key to distinguishing the MPFL from the medial retinaculum is its relation to the overlying VMO muscle. The MPFL extends from the adductor tubercle on the medial femoral condyle to the medial aspect of the superior pole of the patella and lies deep to the VMO muscle, whereas the medial retinaculum attaches to the mid-pole of the patella and is located distal to the VMO muscle (Fig. 12-19). Therefore, on axial images if the VMO muscle is present on the image, then the underlying ligamentous structure represents the MPFL. Absence of the VMO muscle on axial images indicates that the image was obtained distal to the level of the VMO muscle, and the medial soft tissue restraint of the patella at these levels represents either the medial patellar retinaculum or the medial patellotibial ligament (Fig. 12-20).
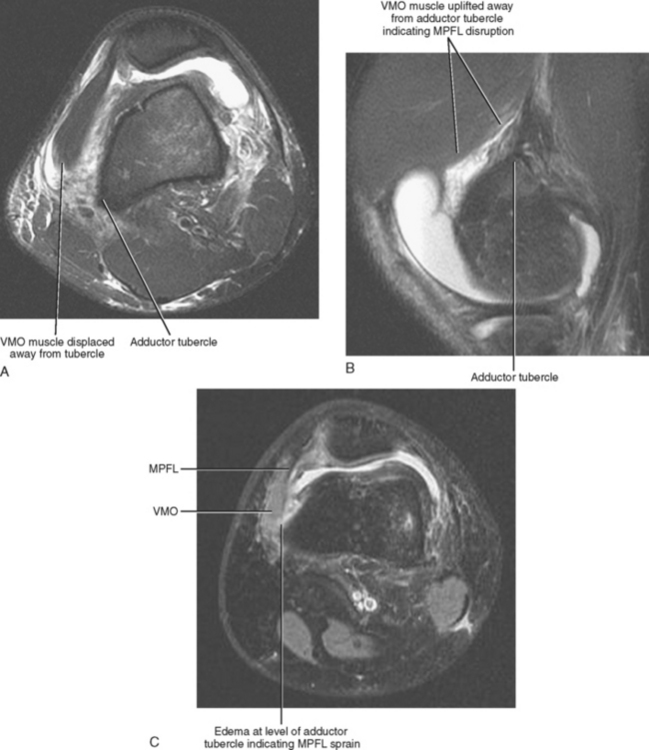
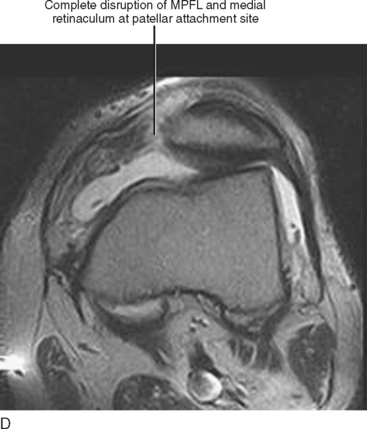
On MRI, the MPFL is visualized in the axial or sagittal imaging planes as a thin linear structure located deep to the VMO, extending from the superior pole of the patellar to the adductor tubercle. As it approaches the adductor tubercle, it blends with the deep fibers of the VMO and is not always clearly differentiated from the deep fascia of the VMO (see Fig. 12-20A). Injury of the MPFL can be classified as a sprain, partial-thickness tear, or complete tear. Approximately 80% of MPFL injuries occur at the femoral attachment site, whereas the remaining 20% occur in either the middle of the ligament or at the patellar attachment site. Disruption of the MPFL at its patellar attachment site or in the middle of the ligament is depicted on MRI as discontinuity and laxity or retraction of the fibers. At the femoral attachment site, the ligament is not clearly differentiated from the fascia of the VMO muscle, and disruption at this level is demonstrated as displacement or uplifting of the VMO muscle away from the adductor tubercle secondary to fluid or hematoma (Fig. 12-21). This can be identified in either the axial or sagittal imaging planes. A sprain or partial-thickness tear appears as edema adjacent to the adductor tubercle, but the VMO muscle is not displaced away from the adductor tubercle.
Middle Third Anatomy
The superficial fibers of the tibial collateral ligament originate on the adductor tubercle of the medial femoral condyle adjacent to the origin of the MPFL and extend in a vertical fashion to an area of broad insertion on the tibia approximately 5 cm below the level of the joint line and deep to the insertion of the pes anserinus tendon. The ligament measures approximately 1.5 cm in anterior to posterior width, and the anterior edge of the tibial collateral ligament often demonstrates a rolled appearance. The ligament is best visualized on coronal images along the medial joint line as a continuous low signal intensity band (Fig. 12-22). The ligament is also seen on axial images as a thin oval structure, which measures approximately 1. 5 cm anterior to posterior and is located superficial to the medial joint line. The rolled appearance of the anterior aspect of the ligament is easily seen on axial images and may give the false impression of thickening of the tibial collateral ligament when imaging through the most anterior aspect of the ligament in the coronal plane.
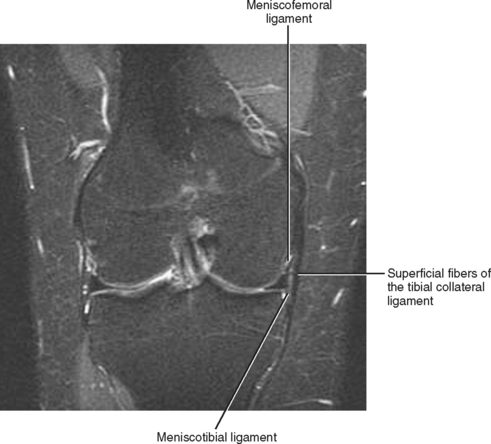
The deep fibers of the tibial collateral ligament are separated from the superficial fibers by a potential space referred to as the tibial collateral ligament bursa. The deep fibers of the tibial collateral ligament form the medial joint capsule (layer 3) and can be divided into three distinct components. The first part directly overlies the medial meniscus and is firmly attached to the adjacent meniscus. The more inferior component is referred to as the meniscotibial ligament and represents a short ligamentous structure that extends from the inferior aspect of the medial meniscus to the adjacent tibia. The more superior component is the longer meniscofemoral ligament, which provides the femoral attachment of the medial meniscus. The deep fibers of the tibial collateral ligament (meniscotibial and meniscofemoral ligaments) are best evaluated on coronal and sagittal MR images (see Fig. 12-22).
Injury Patterns of the Middle Third of the Medial Soft Tissue Structures (Tibial Collateral Ligament)
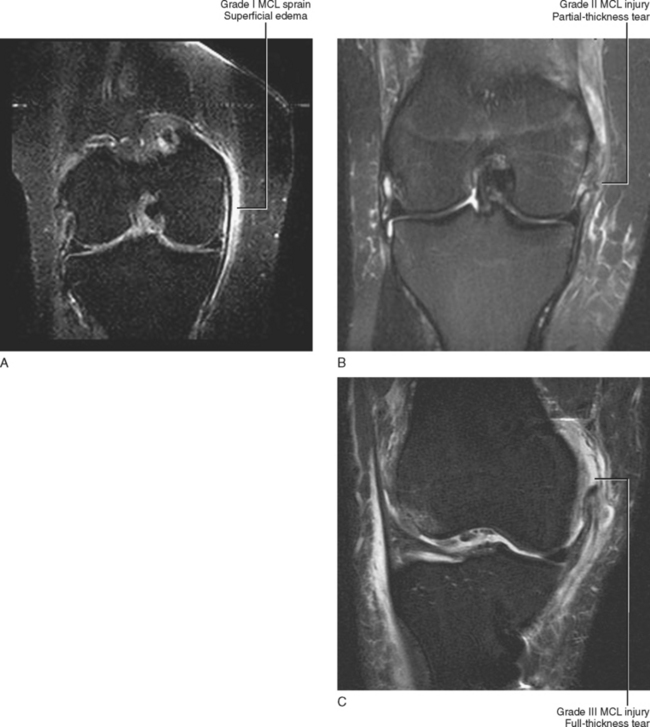
A three-point grading system is used to describe tibial collateral ligament injuries; grade I indicates a sprain, grade II a partial-thickness tear, and grade III a complete tear (Fig. 12-23). Injuries are best depicted on T2-weighted coronal images, and the use of fat-saturation techniques improves conspicuity of the injury. The axial plane is complementary in the evaluation of tibial collateral ligament injuries.
A sprain is demonstrated on MRI as edema superficial to the tibial collateral ligament. Thickening and edema may also be seen within the substance of the ligament, but there should not be fluid signal intensity within the substance of the ligament or disruption of the fibers (see Fig. 12-23). There are a several potential pitfalls with regard to diagnosing a sprain of the tibial collateral ligament (Table 12-6). First, edema isolated to the soft tissues deep to the collateral ligament is often seen in association with an intra-articular process, and this pattern of edema does not indicate collateral ligament injury. Second, it is not uncommon to see edema superficial to the collateral ligament as a reactive phenomenon secondary to an intra-articular process such as a meniscal tear or osteoarthritis. Therefore, one should use caution in diagnosing a sprain of the tibial collateral ligament purely on the basis of superficial edema in the absence of a history of trauma, especially if an adjacent intra-articular pathologic process is present (Box 12-3). Another potential pitfall that can mimic a sprain of the MCL is the presence of a geniculate vessel paralleling the MCL. This can occasionally give the appearance of a small linear collection of fluid superficial to the MCL, but should not be mistaken for an MCL injury. Finally, a tear of the MPFL at the level of the adductor tubercle results in edema at the level of the proximal MCL attachment and can mimic injury of the MCL.
Table 12-6 Mimics of MCL Injury
| MR Finding | Source of MRI Finding |
|---|---|
| Edema deep to MCL | Intra-articular process |
| Edema superficial to MCL | May be reactive to intra-articular process/must correlate with clinical history |
| Edema at level of adductor tubercle | MPFLinjury |
| Fluid signal superficial to MCL | Geniculate vessels |
| Thick anterior fiber of MCL on coronal image | Anterior edge of MCL has a rolled appearance |
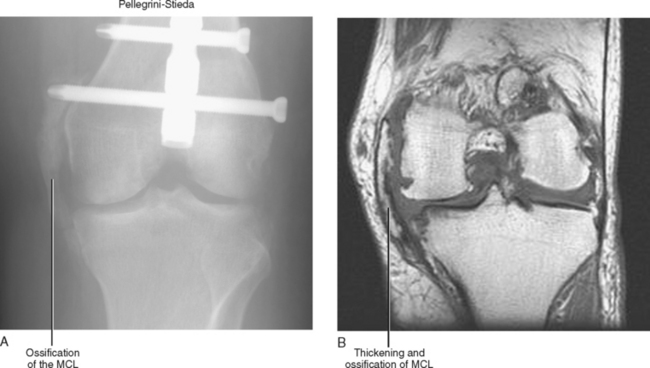
On MRI, a partial-thickness tear appears as a partial-thickness disruption of the fibers with surrounding edema and fluid. These injuries most commonly involve the proximal aspect of the MCL proximal to the level of the joint line. A complete tear is diagnosed when the fibers are completely disrupted with surrounding edema and hemorrhage. Once again these injuries most commonly occur proximal to the joint line. Chronic injury of the tibial collateral ligament results in thickening of the fibers best seen on the coronal images but with a lack of adjacent soft tissue edema. A chronic injury of the tibial collateral ligament may demonstrate ossification within the ligament and is referred to as Pellegrini-Stieda syndrome (Fig. 12-24). A potential pitfall for diagnosing chronic tibial collateral ligament injury is that the most anterior fibers of the normal MCL may appear rolled and as a result, the coronal image through the most anterior portion of the ligament may demonstrate apparent thickening. True thickening resulting from an old injury can be seen on several sequential coronal images and not solely on the most anterior coronal image.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree