Chapter 7 IMAGING OF THE SHOULDER
The shoulder girdle is a complex anatomic unit that is designed to maximize the position on the hand and opposing thumb in three-dimensional space. The shoulder is often thought of as synonymous with the glenohumeral joint, but is actually composed of four separate joints (sternoclavicular, scapulothoracic, acromioclavicular, and the glenohumeral). These four joints work synergistically with numerous muscles and ligaments to optimize motion of the upper extremity and to balance range of motion and stability. Shoulder pain is a very common complaint and is most often seen in association with acute trauma or repetitive overuse. Recent advances in cross-sectional imaging, including CT and MRI, have revolutionized the evaluation of the shoulder, particularly with regard to the soft tissue structures. Conventional radiography, however, remains a mainstay of imaging and is often the first examination ordered for a patient with complaints of shoulder pain.
MODALITIES
Computed Tomography
Computed tomography (CT) is most commonly used after trauma to the shoulder to evaluate the full extent of osseous abnormalities. Multidetector CT examination with sagittal and coronal reconstructions is often used to evaluate the extent of humeral head and neck fractures. The precise number of fracture fragments, the amount of articular surface step-off, displacement, and the angulation of fracture fragments can accurately be determined with CT examination. Each of these variables is important in relation to the treatment choice and in determining the prognosis for recovery. CT examination is also the study of choice in suspected sternoclavicular joint injuries and accurately depicts subtle fractures and dislocations. The scapula is a complex anatomic structure composed of the body, coracoid and acromion processes, and the glenohumeral articular surface. Suspected scapular fractures are typically evaluated with CT examination, which shows the full extent of injury. Fractures limited to the body of the scapula are usually treated conservatively, whereas fractures of the coracoid or acromion processes or the glenohumeral articular surface may require surgical intervention. After glenohumeral dislocation, CT examination is the study of choice to show the size and position of a glenoid rim fracture fragment, which is important in presurgical planning.
IMPINGEMENT: ROLE OF OSSEOUS OUTLET AND ACROMION
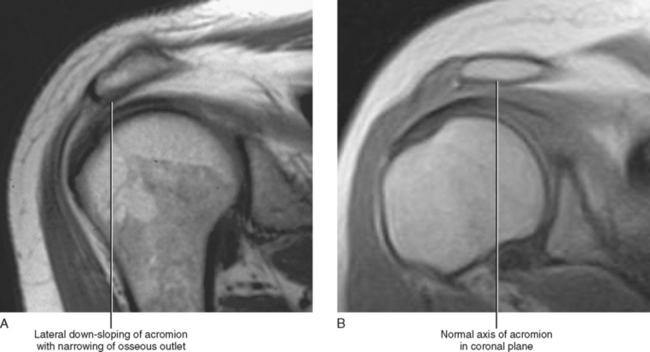
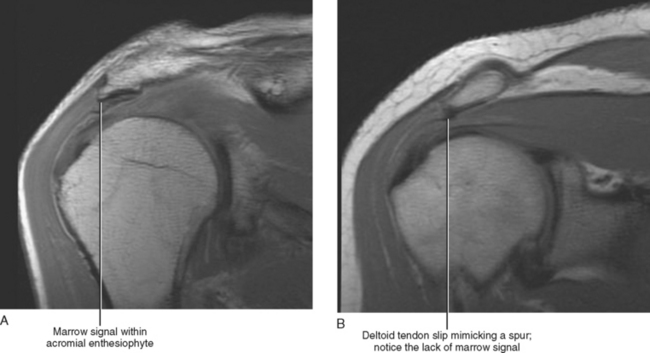
Numerous radiographic and MR findings have been described that are associated with the clinical syndrome of impingement. The acromion, the acromioclavicular (AC) joint, and the coracoacromial ligament should be thoroughly evaluated for these specific configurations, anatomic variants, and abnormalities (Table 7-1).
Table 7-1 MR Evaluation of the Osseous Outlet and Acromion
| Anatomic Part | Abnormality | Preferred MR Imaging Plane |
|---|---|---|
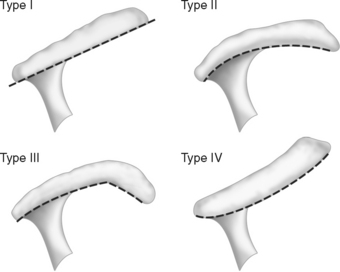
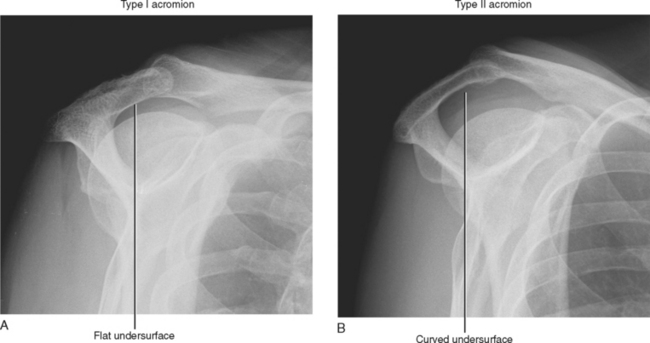
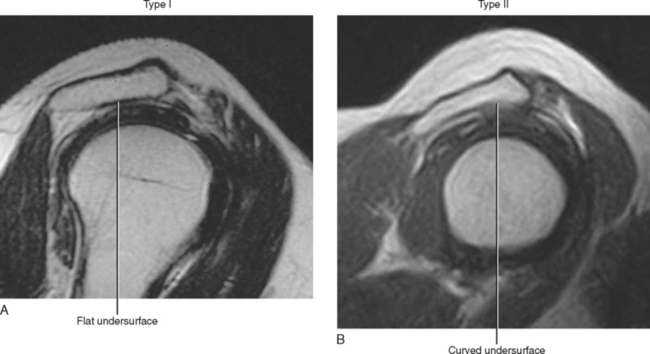
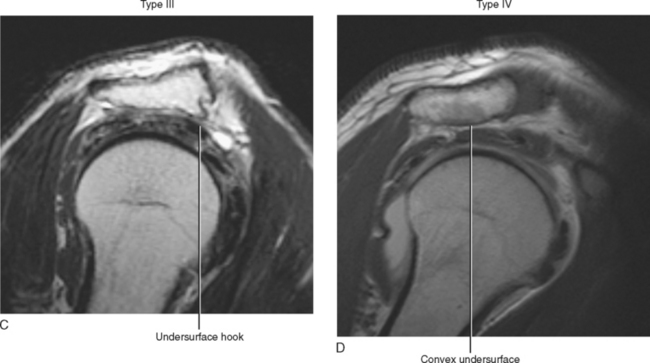
| Acromion | Type or configuration of undersurface (Types I, II, III, IV) | Sagittal; 1–2 images peripheral to AC joint |
| Anterior down-sloping | Sagittal | |
| Lateral down-sloping | Coronal | |
| Enthesiophyte formation | Sagittal/coronal | |
| Os acromiale “double AC joint” sign | Axial—primary Sagittal/coronal—secondary | |
| Acromioclavicular (AC) joint | Osteoarthritis (mass effect on underlying cuff) | Coronal/sagittal |
| AC joint separation (grades I, II, III) | Coronal | |
| Osteolysis of distal clavicle | Coronal | |
| Coracoacromial ligament | Thickening | Sagittal |
| Calcification | Sagittal |
Acromion
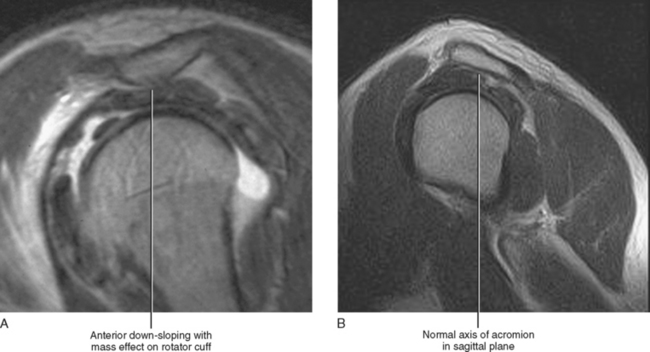
Figure 7-4 Anterior down-sloping of the acromion. A, Anterior down-sloping narrows the acromial-humeral distance and can be a cause of rotator cuff impingement. Evaluation for anterior down-sloping is performed using the sagittal MRI plane. Anterior down-sloping describes the axis of the acromion in the sagittal plane and is independent of the configuration of the undersurface of the acromion as described in Figures 7-1 and 7-2. B, Normal acromial axis in the sagittal imaging plane.
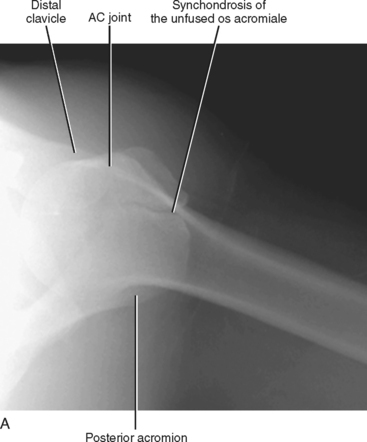
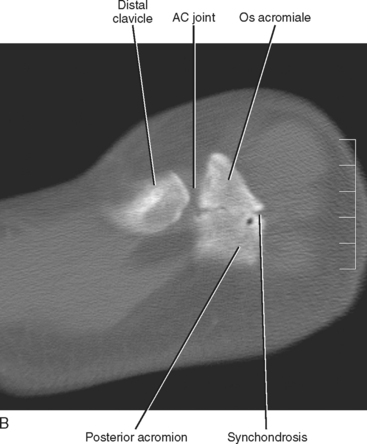
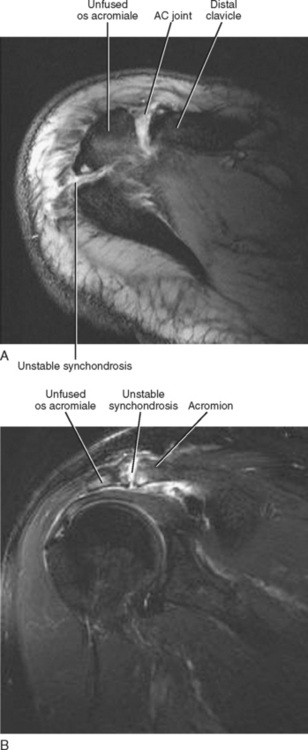
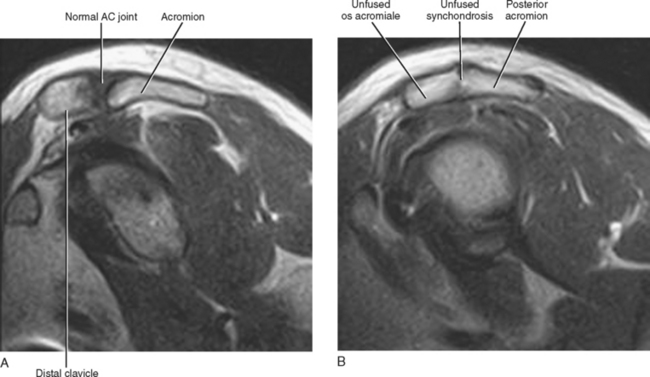
The MR appearance of an unfused os acromiale is variable depending on which ossification center fails to fuse. The unfused os acromiale is best depicted on axial images (Fig. 7-8). However, the most superior axial image obtained on MRI of the shoulder often begins below the level of the acromion; as a result, if one relies solely on the axial images, an unfused os acromiale may be overlooked. Therefore, the oblique sagittal and oblique coronal images should also be evaluated for an unfused os acromiale. An unfused os acromiale on sagittal or coronal images often demonstrates an appearance similar to that of the AC joint and may be misinterpreted as the AC joint. Simultaneous visualization of the AC joint and the unfused os acromiale on the same image gives the appearance of a “double AC joint,” and has been referred to as the double AC joint sign. More often, the unfused os acromiale appears as a second AC joint (Fig. 7-9) on an image two to three slices posterior to the true AC joint. The presence of fluid within the synchondrosis or edema surrounding the synchondrosis seen on MR imaging usually indicates pseudarthrosis or fibrous union and is an indication of probable instability.
An unfused os acromiale can occasionally mimic an acromial fracture. The two entities can be differentiated because the accessory ossicle usually appears triangular with sclerotic margins and forms a synchondrosis that is always oriented perpendicular to the long axis of the acromion. An acute fracture, on the other hand, is usually oriented at an oblique angle relative to the long axis of the acromion and demonstrates nonsclerotic irregular margins (Fig. 7-10).
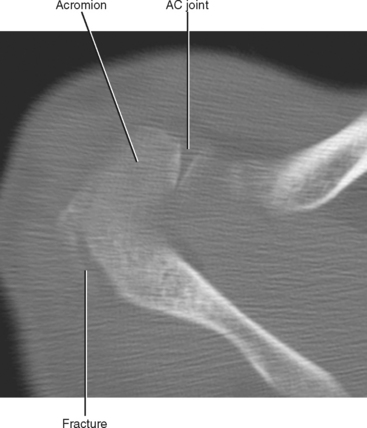
Figure 7-10 Acromiale fracture. Axial CT image demonstrates a minimally displaced fracture of the posterior acromion. The fracture shows an oblique orientation relative to the long axis of the acromion, and the margins of the fracture fragments are nonsclerotic and slightly irregular when compared with an unfused os acromiale (see Figs. 7-7A and B).
Acromioclavicular Joint
Abnormalities of the AC joint are common and are often detected while imaging the shoulder. Osteoarthritis is a very common entity in patients over 40 years of age, whereas in the young athletic individual, post-traumatic AC joint separation and osteolysis of the distal clavicle are common entities. These conditions occasionally mimic one another, but can usually be differentiated on the basis of history and imaging findings (Table 7-2).
Table 7-2 Acromioclavicular (AC) Joint Osteoarthritis versus Osteolysis Distal Clavicle
| Osteoarthritis | Post-traumatic Osteolysis | |
|---|---|---|
| Patient | Typically > 40 | Young athlete |
| Symptoms | Minimally symptomatic or asymptomatic | Painful |
| Etiology | No history of trauma | Acute trauma: Repetitive microtrauma (weight-lifters) |
| Location of involvement | Both sides of joint | Isolated to distal clavicle |
| Radiographic findings | ||
| MR findings |
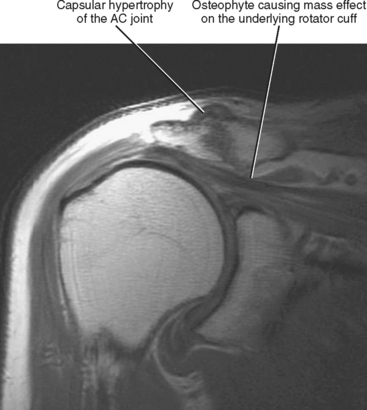
Osteoarthritis of the AC joint typically involves both sides of the joint, and imaging findings include capsular hypertrophy, joint effusion, and adjacent soft tissue edema. Osteophyte formation, subchondral marrow signal change, and subchondral cyst formation can also occur on both sides of the joint. The differential diagnosis for marrow edema on both sides of the AC joint includes recent AC joint separation, osteoarthritis, and inflammatory arthritis. Osteoarthritis of the AC joint is often asymptomatic or minimally symptomatic when compared with post-traumatic osteolysis of the distal clavicle, which can be quite painful. Osteoarthritis of the AC joint can be a source of extrinsic impingement on the rotator cuff; however, the AC joint does not play as crucial a role as does the anterior acromion with regard to impingement. The portion of the cuff immediately underlying the AC joint is less rigidly confined than the portion of the cuff underlying the anterior acromion, and degenerative osteoarthritis of the AC joint may result in the appearance of mass effect on the underlying cuff on MRI when there are no clinical symptoms of impingement. Degenerative changes of the AC joint with its associated mass effect on the underlying cuff are best appreciated on sagittal and coronal MR images (Fig. 7-11). Large joint effusion and pericapsular edema are signs that are often associated with synovitis of the AC joint and are associated with an increased incidence of symptomatic AC joint osteoarthritis.
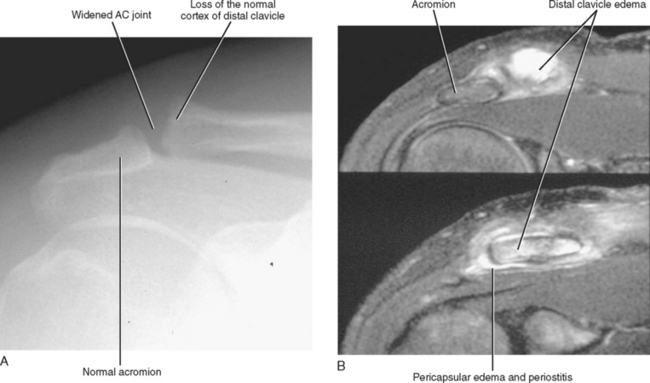
Post-traumatic osteolysis of the distal clavicle is a painful condition that typically occurs after mild to moderate acute trauma to the AC joint or after repetitive microtrauma, as seen in weight lifters and other athletes who experience repetitive stress to the AC joint. Clinically, osteolysis differs from osteoarthritis in that it usually occurs in the young athlete and results in moderate to severe pain, whereas osteoarthritis occurs in the older patient population with no history of trauma or repetitive stress and is minimally painful or asymptomatic.
Initial radiographs in post-traumatic osteolysis demonstrate soft tissue swelling of the AC joint, demineralization, and loss of the cortical margin of the distal clavicle (Fig. 7-12A). The AC joint may appear widened during the acute phase, but over time the distal clavicle usually reconstitutes, at least in part. Chronic changes of subchondral sclerosis and subchondral cystic change isolated to the distal clavicle are common. Early in post-traumatic osteolysis, MRI demonstrates marrow edema isolated to the distal 1 to 3 cm of the clavicle and may demonstrate loss of the normal cortical black line. Findings of a small joint effusion, capsular hypertrophy, and pericapsular edema of the AC joint are often present. Late findings may include widening of the AC joint, mild capsular hypertrophy, and cortical irregularity or subchondral sclerosis involving the distal tip of the clavicle (Fig. 7-12B).
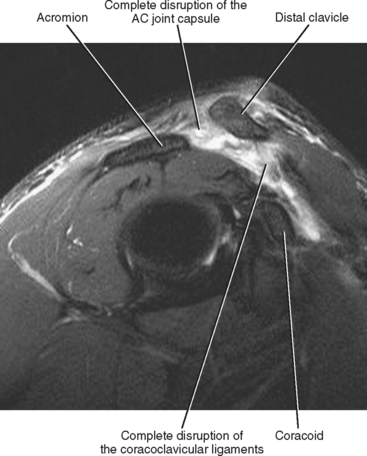
After trauma to the shoulder, the AC joint should also be evaluated for evidence of fracture and AC joint separation. A fracture is seen on MRI as a dark line on both T1- and T2-weighted images with surrounding marrow edema. Separation of the AC joint is graded on a three-point scale (Fig. 7-13).
Grade I injury: Mild strain of the AC joint; the AC and coracoclavicular (CC) ligaments remain intact. Radiographs of the shoulder are normal, and MRI shows only mild pericapsular edema of the AC joint. The symptoms are mild, treatment is conservative, and the patient usually recovers spontaneously.
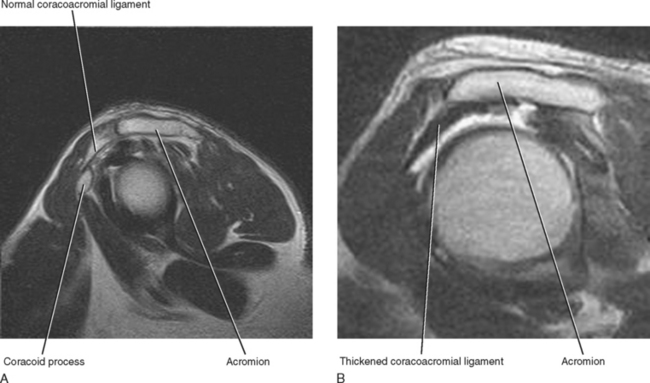
Coracoacromial Ligament
The coracoacromial ligament is a stout and sturdy ligament that forms a portion of the osseous outlet and acromion, covering the anterior fibers of the supraspinatus tendon and the rotator interval as it extends from the coracoid process anteriorly to the acromion posteriorly. The ligament is best visualized on oblique sagittal MR images and is usually no more than 2 to 3 mm-thickness (Fig. 7-14A). Thickening, hypertrophy, or calcification of the coracoacromial ligament can result in extrinsic impingement on the anterior portion of the rotator cuff (Fig. 7-14B). A thickened ligament is usually treated with either debridement or release at the time of subacromial decompression. In the younger patient, partial debridement of the ligament is preferable because this helps to prevent superior migration of the humeral head, whereas in the older patient the ligament is usually completely released.
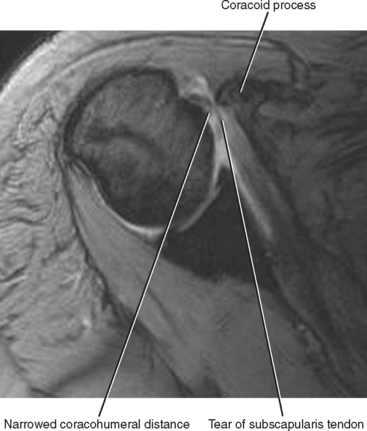
Coracohumeral Impingement (Subcoracoid Impingement)
Coracohumeral impingement is an uncommon cause of rotator cuff impingement that results from the entrapment of the subscapularis tendon within a narrowed coracohumeral space. The normal coracohumeral distance is approximately 11 mm as depicted on axial MR images. A coracohumeral distance of less than 7 mm may result in entrapment of the subscapularis tendon between the humeral head and the coracoid process, eventually leading to a tear of the tendon (Fig. 7-15). In the case of coracohumeral impingement, successful surgical management requires not only repair of the subscapularis tendon but also correction of the narrowed coracohumeral distance. An isolated tear of the subscapularis tendon should prompt an evaluation of the coracohumeral distance to avoid missing this underlying cause of impingement.
ROTATOR CUFF
The rotator cuff is composed of four separate muscles and their tendons. Each muscle originates along either the anterior or posterior margin of the scapula and then extends toward and completely covers the humeral head with tendons inserting onto either the greater or lesser tuberosities of the humeral head. The rotator cuff contributes to the motion of the upper extremity and also plays an important role in stabilizing the humeral head within the glenoid fossa during movement of the glenohumeral joint. The rotator cuff is often referred to as an active stabilizer of the rotator cuff.
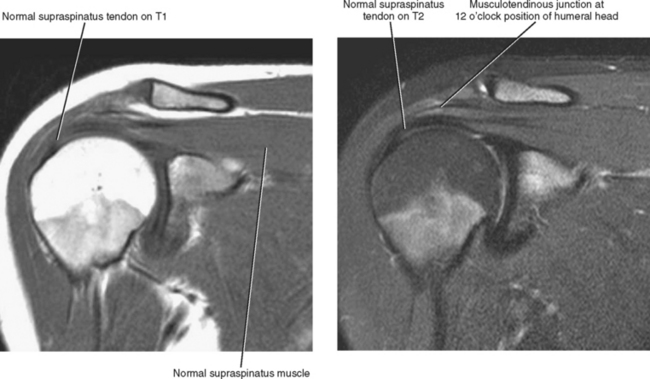
MR Appearance of the Normal Rotator Cuff
The supraspinatus muscle and tendon are best evaluated on the oblique coronal and sagittal imaging planes (Fig. 7-16); the axial images, however, also provide important information regarding the status of the supraspinatus. The normal muscle should completely fill the supraspinatus fossa and should demonstrate intermediate T1 and T2 signal. Without fatty atrophy, the muscle should demonstrate a bulk that is relatively similar to that of the infraspinatus and teres minor muscles, as seen on the oblique sagittal images. The supraspinatus muscle tapers from central to peripheral with the normal musculotendinous junction situated at approximately the 12 o’clock position of the humeral head. The infraspinatus and teres minor muscles are also best evaluated on the oblique sagittal and oblique coronal images, and these two muscles should completely fill the infraspinatus fossa. They also taper peripherally with their musculotendinous junctions located at a level similar to that of the supraspinatus muscle. On coronal images, the supraspinatus tendon can easily be differentiated from the infraspinatus because the supraspinatus tendon is oriented horizontally, whereas the infraspinatus tendon is oblique in orientation.
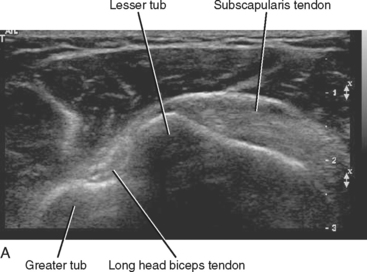
Ultrasound Appearance of the Rotator Cuff
A complete description of the technique for ultrasound examination of the rotator cuff is beyond the scope of this chapter. However, knowledge of the normal MR appearance of the cuff can aid in the understanding the normal ultrasound appearance of the cuff. The examination often begins by scanning in the transverse imaging plane along the anterior surface of the shoulder to identify the key landmark of the long head of the biceps tendon within the intertubercular groove covered by the subscapularis tendon. Imaging then proceeds in a systematic manner to evaluate the musculotendinous units of each rotator cuff muscle in both the transverse and longitudinal planes. The normal rotator cuff tendon demonstrates a typical bandlike appearance of medium-level echoes located deep to the deltoid muscle. A thin stripe of bright echoes just superficial to the rotator cuff tendon represents the normal subacromial subdeltoid bursa. Muscle is hypoechoic in appearance. The biceps tendon is seen as an oval-appearing area of bright echoes located within the intertubercular groove. The bony surface of the humerus results in a rim of bright echoes (Fig. 7-17).
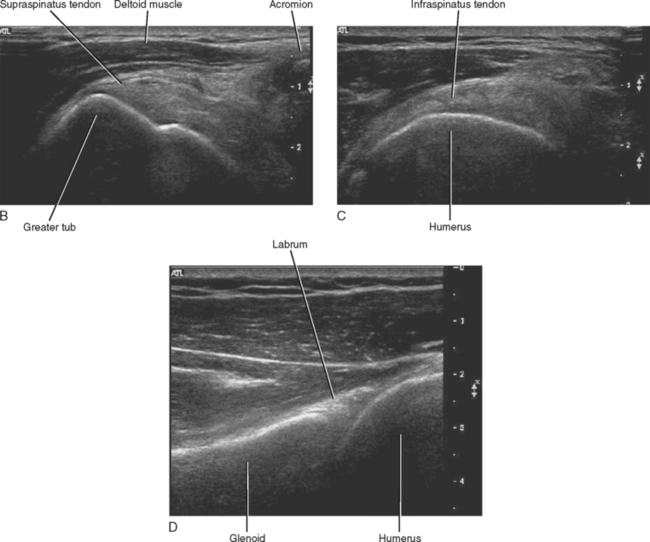
Sonographic signs of a rotator cuff tear include:
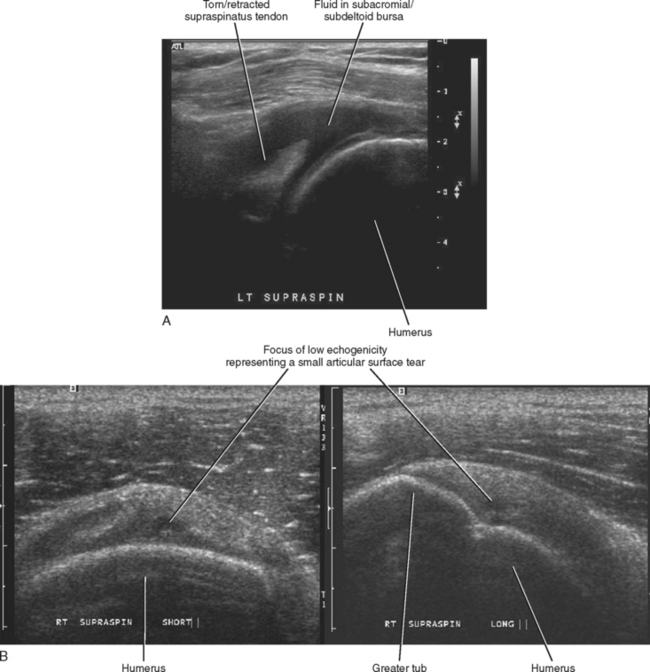
Tendinosis may manifest as focal or diffuse areas of tendon thickening with altered echogenicity, either increased or decreased. A secondary sign of rotator cuff pathology may include fluid within the subdeltoid bursa (Fig. 7-18).
MR Appearance of Rotator Cuff Pathology
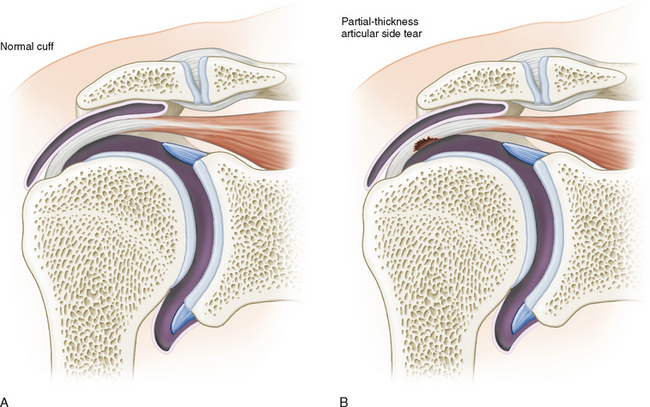
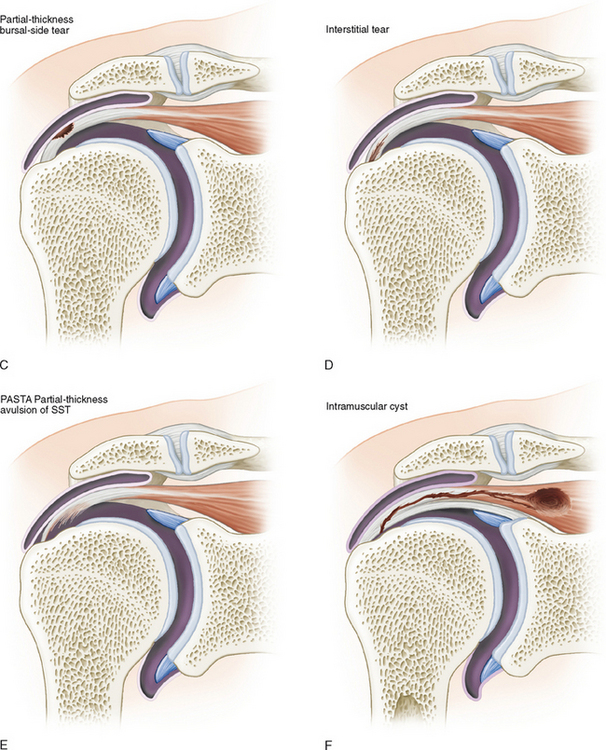
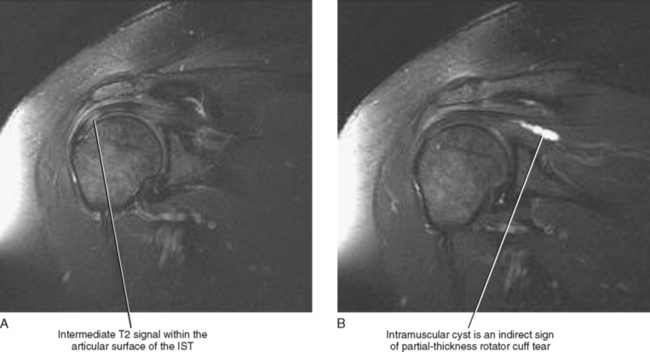
The sensitivity and specificity of MRI in the detection of rotator cuff tears range from 88% to 100%. Supraspinatus and infraspinatus pathology is best demonstrated on T2-weighted coronal and sagittal images, whereas subscapularis pathology is best evaluated on axial T2-weighted sequences. Rotator cuff pathology can be classified as discussed in the following text (Table 7-3 and Fig. 7-19).
Table 7-3 MR Appearance of Rotator Cuff Pathology
| Cuff Pathology | Appearance on MRI |
|---|---|
| Normal tendon | Dark on T1 and T2 |
| Tendonopathy | Thickening of tendon |
| Intermediate signal T1/T2 | |
| Calcific tendinitis | Globular decreased signal T1/T2 within tendon; often with surrounding soft tissue edema |
| Thickened tendon; intermediate signal T1/T2 | |
| “Blooming” artifact on gradient echo | |
| Partial-thickness tear | Fluid signal/gadolinium extending partially through tendon superior to inferior |
| Bursal/articular/interstitial | |
| Associated intramuscular cyst | |
| No retraction of tendon | |
| Full-thickness tear | Fluid extending completely through tendon top to bottom |
| Retraction of tendon | |
| Gap/discontinuity in tendon | |
| Musculotendinous retraction | Measured as the length of the medial-to-lateral tendon gap |
| Fatty atrophy | Grade—mild/moderate/severe |
| Streaks of high signal on T1—irreversible | |
| Loss of muscle bulk relative to other rotator cuff muscles on sagittal imaging—reversible |
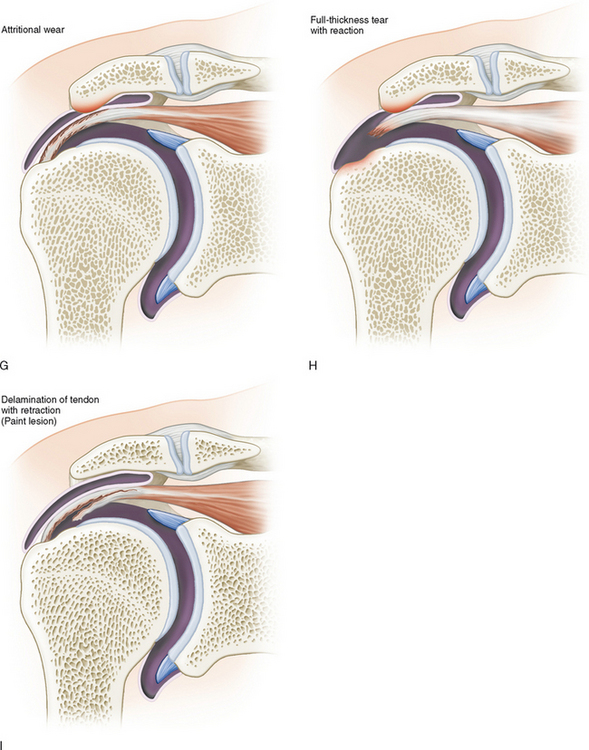
On MRI, tendinopathy appears as intermediate signal intensity within the substance of the tendon on both T1- and T2-weighted images (slightly less bright than water on T2 images). The tendon may also demonstrate mild to moderate thickening (Fig. 7-20). Histologically, the increased signal represents mucoid degeneration of the tendon.
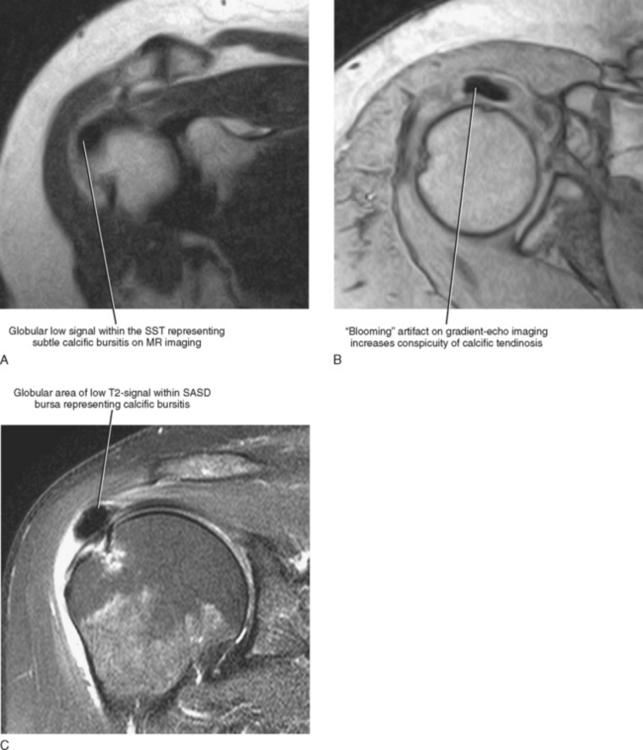
Hydroxyapatite deposition disease can occur within the rotator cuff tendon, calcific tendinitis, or within other periarticular soft tissues including the glenohumeral ligaments and adjacent bursa, calcific bursitis (Fig. 7-21). These calcifications are best detected on radiographs but may also be identified on MRI as focal areas of globular decreased signal on both T1- and T2-weighted images. Calcific tendinitis is often associated with intense inflammatory changes of the adjacent soft tissues, resulting in surrounding increased signal on T2-weighted images. On MRI, it may be difficult in some cases to detect the calcification and to distinguish calcific tendinitis from noncalcific tendinitis. Gradient-echo imaging can be helpful in this regard, since “blooming” artifact seen on gradient-echo images exaggerates the size and appearance of the calcification.
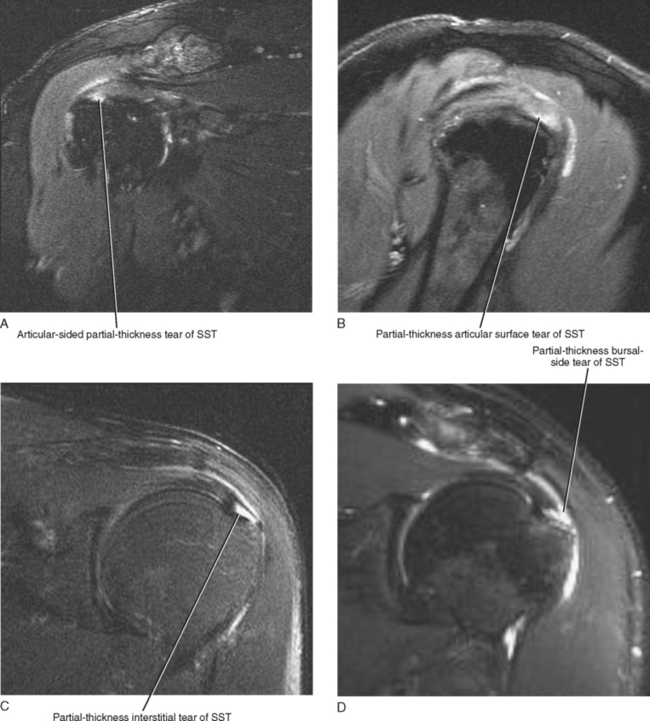
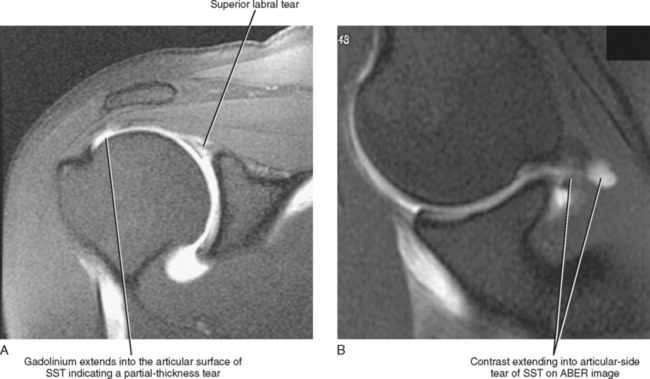
A partial-thickness tear of the rotator cuff is defined as a tear that extends partially through the thickness of the tendon from superior to inferior. MR imaging demonstrates fluid signal intensity on T2-weighted images extending partially through the thickness of the tendon. The tear may involve the bursal or articular surface, or the interstitial portions of the tendon (Fig. 7-22). A partial-thickness tear may occasionally be difficult to differentiate from tendinopathy, especially when partial healing has occurred with granulation tissue filling the tendon defect. The granulation tissue may demonstrate intermediate signal intensity on T2-weighted images, mimicking tendinopathy.
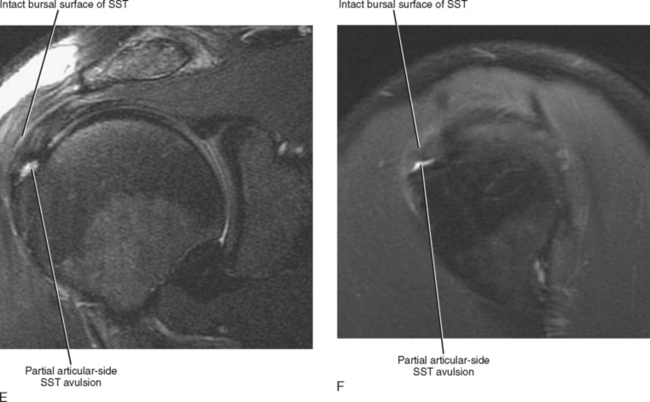
One helpful indirect MRI sign that can help in establishing the diagnosis of a partial-thickness rotator cuff tear is the presence of an intramuscular cyst. Joint fluid can track through the defect of a partial-thickness articular surface tear of the rotator cuff tendon and then dissect in a laminar fashion through the tendon and form a cyst within the substance of the rotator cuff muscle. These intramuscular cysts can easily be differentiated from paralabral cysts because they are contained within the fascia of the rotator cuff muscle, best demonstrated on sagittal T2-weighted images. An intramuscular cyst has a high association with partial-thickness tearing of the rotator cuff, just as a paralabral cyst has a high association with a labral tear. The presence of an intramuscular cyst can help differentiate between tendinopathy and a partial-thickness tear of the rotator cuff (Fig. 7-23). Two other imaging tips that can help differentiate between tendinopathy and a partial-thickness articular surface tears of the rotator cuff are the use of direct MR arthrography and ABER (abducted and externally rotated) imaging (with or without intra-articular contrast). Both techniques improve the conspicuity of partial-thickness articular surface tears of the rotator cuff (Fig. 7-24).
A partial articular-side supraspinatus tendon avulsion or “PASTA” lesion is a subset of partial-thickness tears that has been recently described in the orthopedic literature. The tear represents a partial-thickness articular-side avulsion of the supraspinatus tendon at its most anterior attachment site. This type of tear deserves special attention and should be accurately described on MRI because the recommended treatment for this subset of tendon tears differs from the standard partial-thickness tears previously described. A transtendon suture technique is performed to preserve the intact portion of the tendon while firmly reattaching the torn portion of the tendon to the humeral footprint. On MRI, a small articular-side avulsion is seen as fluid signal extending into the articular surface of the supraspinatus tendon at its anterior attachment site with partial avulsion of the tendon at this level and represents a subset of the articular surface partial-thickness tears (see Fig. 7-22E and F).
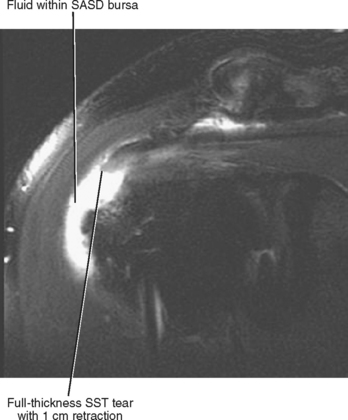
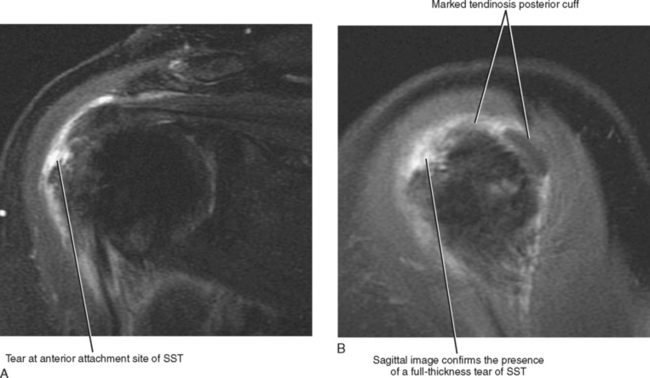
A full-thickness tear of the rotator cuff is defined as a tear that extends completely through the thickness of the tendon from superior to inferior. MR demonstrates bright fluid on T2-weighted images extending through the entire thickness of the tendon (Fig. 7-25). There may be retraction of the torn tendon end. Sagittal and axial images can be very helpful in differentiating a partial-thickness from a fullthickness tear, especially when the tear is located at the level of attachment to the humeral head. Small full-thickness tears often involve the most anterior aspect of the supraspinatus tendon immediately adjacent to its attachment to the greater tuberosity. It is important to evaluate the supraspinatus tendon on the most anterior coronal image to avoid missing a small full-thickness tear at the most anterior bone-tendon interface (Fig. 7-26). The extent of tear should be measured and reported in both the anteroposterior and medial-lateral directions. A tear that is larger in the anteroposterior direction is often repaired using a tendon-to-bone suture technique, whereas a tear that is greater in the medial-lateral direction may be amenable to repair using a mattress type tendon-to-tendon repair technique.
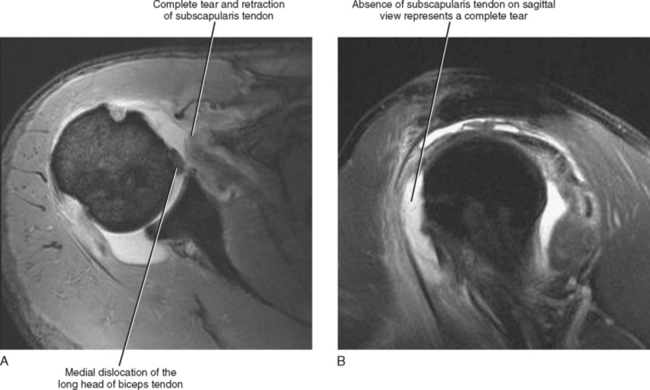
Tears of the subscapularis tendon are best depicted on axial and sagittal images and are often associated with subluxation or dislocation of the biceps tendon out of the intertubercular groove (Fig. 7-27). The subscapularis tendon is typically seen covering the anterior portion of the humeral head on the sagittal imaging plane. Fluid within the expected location of the subscapularis tendon anterior to the humeral head indicates a complete tear with retraction of the torn tendon end.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree