The thoracic aorta may be affected by various disorders including aneurysms, dissections, intramural hematomas, penetrating atherosclerotic ulcers, and acute aortic injury. Specific pathophysiologic details of these entities are beyond the scope of this chapter and are reviewed elsewhere in this book. This chapter focuses on the surgical and endovascular interventions used to treat the diseased thoracic aorta. The initial part of the chapter discusses the most common postoperative complications that may be seen after thoracic aortic repair, regardless of the surgical procedure. The chapter then details the different types of thoracic aortic surgical procedures, beginning with operations on the ascending aorta, followed by operations on the aortic arch, and finishing with endovascular procedures performed on the descending thoracic aorta. For each specific surgical procedure, the expected appearance of the postoperative aorta, as well as the appearance of common complications, will be described; the cardiovascular imager must be familiar with both normal and abnormal features, to interpret images of the postoperative aorta correctly.
Indications for Treatment
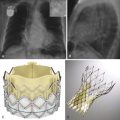
A consensus statement was published on the indications for open surgical and endovascular intervention in the thoracic aorta. The indications were based on data that demonstrated, in certain groups of patients, that the risk of mortality from untreated aortic disease outweighs the risk of intervention. Indications for intervention in the ascending thoracic aorta include the following: evidence of rupture; a diameter greater than 5.5 cm for the general population or greater than 5.0 cm in patients with Marfan syndrome, other connective tissue disorder, or a bicuspid aortic valve; aneurysm growth of more than 0.5 cm per year; or any aneurysm that is symptomatic. Indications for intervention in the descending thoracic aorta include a diameter of more than 6.5 cm in the general population or more than 6 cm in patients with Marfan syndrome and other connective tissue disorders.
Open Surgical Procedures in the Thoracic Aorta, Including their Complications
Most patients who have undergone open procedures of the thoracic aorta are often evaluated with computed tomography (CT), although magnetic resonance imaging (MRI) is an excellent alternative when necessary. Details on CT protocols are beyond the scope of this chapter; however, some fundamental and general concepts are described. Although no universally accepted protocol exists, in general, two CT acquisitions are recommended: an initial CT acquisition without intravenous contrast and a second CT acquisition after the administration of intravenous contrast material; imaging for the enhanced CT is most often obtained during the arterial phase. The purpose of the non-enhanced CT is to identify postoperative material that appears hyperdense and that could be misinterpreted as extraluminal contrast material on enhanced CT (e.g., anastomotic felt along the anastomosis). Moreover, nonenhanced CT can demonstrate a high-attenuation hematoma within the aortic wall; after the administration of intravenous contrast material, the high density of the hematoma may be obscured by the adjacent contrast. However, in the evaluation of the postoperative aorta, most of the information is obtained after the administration of intravenous contrast material. Acquiring images during the arterial phase is important because life-threatening complications such as pseudoaneurysm and dissection may be identifiable only during this phase. Cardiac gating can be helpful when precise assessment of the aortic valve, coronary arteries, and coronary bypass grafts is required. However, most assessments are currently performed without cardiac gating because most complications can be identified on nongated images.
When assessing the postsurgical aorta, radiologists and other clinicians must be aware of several components to avoid misinterpreting normal postoperative structures as pathologic. Synthetic grafts, often made from polyethylene, are smooth-walled, round structures that appear slightly hyperdense on unenhanced CT ( Fig. 24-1 ) and are relatively hypodense to the enhanced blood pool on contrast-enhanced CT. Anastomoses of the graft to the native aorta are generally identified by a sharply demarcated change in caliber of the vessel; these changes in caliber are often most easily identified on multiplanar reformations, particularly reformations that demonstrate the vessel in its long axis. The anastomoses are also almost always marked by felt pledgets, strips, or rings that buttress the suture lines; these objects are hyperdense on both noncontrast and contrast-enhanced CT. Confirmation that the area of the felt objects is of high density on the noncontrast CT can prevent the misinterpretation of these foci as small pseudoaneurysms, a common pitfall. Furthermore, felt rings and strips tend to be located along the entire circumference of the anastomosis rather than being positioned along a single wall, as is often the case with pseudoaneurysms ( Figs. 24-2 and 24-3 ).



Finally, aortic grafts generally fall into one of two types: inclusion grafts or interposition grafts. In an inclusion graft, a synthetic graft is positioned within the diseased aortic lumen, and the native aorta is wrapped around the graft; therefore, a potential space exists between the graft and the native aortic wall. An interposition graft replaces the diseased portion of the aorta; the diseased portion of the aorta is resected, and the graft is sewn from end to end to the remaining portion of the aorta. Most recent and current surgical procedures are interposition procedures. However, patients who have had remote surgical procedures may still present for CT with inclusion grafts. Therefore, radiologists must have an understanding of inclusion graft anatomy to interpret these examinations properly.
General Complications of Open Thoracic Aortic Operations
Radiologists must be familiar with the normal appearance of the aorta immediately after surgery, to differentiate normal postoperative findings from postoperative complications. Many of the normal postsurgical findings are described in the following subsections. Additionally, several general complications of open thoracic aortic procedures are also described.
Sterile and Infected Perigraft Fluid Collection
Sterile postoperative perigraft fluid collections may be seen as a result of evolving postoperative hematoma or as a result of an inflammatory reaction elicited by the synthetic graft material. Sterile perigraft fluid collections are common postoperative occurrences that can resolve or remain stable over time ( Fig. 24-4 ). Data suggest that a large amount of perigraft hematoma (>1.5 cm in thickness) on initial postoperative imaging is associated with an increased risk of pseudoaneurysm formation at the anastomosis. Radiologic features that suggest superinfection of a perigraft collection include rim enhancement after contrast administration, increasing air within the collection, a fistulous connection to adjacent structures, and extension into other mediastinal compartments.

Perigraft Gas Collections
The presence of mediastinal, perigraft air is an expected normal postsurgical finding that can persist for several weeks. However, the persistence of air for more than 8 weeks or an increasing amount of mediastinal air is highly suggestive of a developing infection or fistula (i.e., bronchial or esophageal) formation.
Sternal Osteomyelitis
Sternal osteomyelitis is a relatively common complication after median sternotomy. The infection can spread into the adjacent mediastinum and can result in mediastinitis. The radiologic findings of osteomyelitis include bone destruction, severe demineralization, change in orientation of the sternal wires, or frank sternal dehiscence. These findings are more conspicuous on CT than on radiography; furthermore, CT delineates other findings associated with osteomyelitis such as periosteal reaction, osseous sclerosis, and adjacent fluid collections ( Fig. 24-5 ). When the CT appearance is nonspecific but osteomyelitis is of clinical concern, nuclear medicine studies with radiolabeled leukocytes may provide additional information.

Specific Surgical Procedures Involving the Ascending Aorta
Supracoronary Grafts
Any repair that spares the aortic root (or sinuses of Valsalva) is generically called a supracoronary graft. If a repair involves both a supracoronary graft and an aortic valve replacement (thus sparing the sinuses of Valsalva), it is often referred to as the Wheat procedure (originally described by Wheat in 1964) ( Fig. 24-6 ). Because the aortic root is spared, a supracoronary repair maintains the normal integrity of the coronary arteries. Therefore, a supracoronary repair is technically less complicated and avoids potential complications involving the coronary arteries (e.g., coronary pseudoaneurysm).

Potential complications of supracoronary reconstruction include the development of dissection or aneurysm involving the native aortic root. These complications occur most frequently in patients with connective tissue disorders or inflammatory processes such as aortitis. An additional possible complication is the development of a pseudoaneurysm at the anastomosis with the. native aorta. The development of a pseudoaneurysm is the result of weakening of the surgical anastomosis; this may be caused by infection.
Complications of supracoronary repair are often identified in asymptomatic patients undergoing routine surveillance CT or MRI. Determining the possible presence of an aortic root aneurysm may be difficult because the normal size of the aortic root varies depending on gender and age. If, however, on serial examinations, the native aortic root changes in appearance or diameter, concern regarding a complication such as aneurysm formation should be raised. Aortic dissection involving the sinuses of Valsalva classically manifests with an intraluminal flap on cross-sectional imaging ( Fig. 24-7 ). This is an emergency finding because dissection in this portion of the aorta may involve the coronary arteries and may place the patient at risk of myocardial infarction. Finally, a pseudoaneurysm at the anastomotic site usually appears as an extraluminal mass on noncontrast CT. After intravenous contrast administration, pseudoaneurysms usually enhance markedly, although they may have nonenhancing components related to the presence of peripheral thrombus ( Fig. 24-8 ).


Composite Artificial Graft
When the aortic abnormality involves the sinuses of Valsalva, such as in patients with annuloaortic ectasia, the aortic reconstruction includes the aortic root. Two of the most common surgical techniques that involve the aortic root are the Bentall and Cabrol procedures ( Figs. 24-9 and 24-10 ). In these operations, the aortic. valve is incorporated into the synthetic aortic graft; therefore, the aortic valve and the graft are implanted as a single unit. Because the sinuses of Valsalva are being replaced, the coronary arteries must be reimplanted onto the graft. The Bentall and Cabrol procedures differ from one another in the method by which the coronary arteries are reanastomosed to the aortic graft. In the Cabrol procedure, the coronary arteries are sewn onto a conduit that, in turn, is anastomosed to the ascending aorta. When the coronary conduit takes a retroaortic course, the wall of the conduit may mimic an intimal flap. Therefore, the radiologist must recognize the presence of the coronary conduit to. avoid misinterpreting this normal appearance as a dissection or a pseudoaneurysm.


In the Bentall procedure, the coronary arteries are directly implanted onto the ascending aortic graft. The original Bentall procedure had a high rate of complications involving the anastomoses of the coronary arteries onto the aortic graft. Therefore, the surgical procedure was revised; in the revised Bentall procedure, referred to as the button Bentall procedure, the coronary arteries are excised from the native aorta with a rind of native aortic wall, called a button. The button of native aortic tissue is then sewn to the ascending aortic graft. The button procedure has become the most common. method for attaching the coronary arteries onto an ascending aortic graft. The button may cause the origin of the coronary arteries to appear slightly dilated on CT ( Fig. 24-11 ); the radiologist must be familiar with this normal appearance so as not to confuse the prominent button with an aneurysm or pseudoaneurysm, a common pitfall.

Postoperative complications of the Bentall procedure include pseudoaneurysms at the coronary anastomoses ( Fig. 24-12 ) (which are much less common with the button Bentall modification) and at the aortic anastomoses ( Fig. 24-13 ). Patients with Marfan syndrome are particularly prone to develop coronary pseudoaneurysms. In addition to pseudoaneurysm formation, patients who have undergone the Cabrol procedure are also at risk of complications related to the coronary conduit. On CT, thrombosis of the Cabrol coronary conduit may be diagnosed when contrast enhancement within the graft is lacking on contrast-enhanced CT ( Fig. 24-14 ). Intimal hyperplasia of the conduit may appear on CT as low-density thickening of the conduit wall. Kinking of the conduit, with or without associated thrombosis, may also be seen. Because of the potential complications involving the coronary graft, the Cabrol procedure is now rarely performed; it is generally restricted to patients for whom a button Bentall is precluded, such as patients whose coronary arteries are difficult to mobilize.



Biologic Grafts
As an alternative to synthetic grafts, biologic grafts may be used in aortic reconstruction. Both cadaveric and autologous grafts have been used. The Ross procedure is an autograft that includes the pulmonic valve and proximal pulmonary trunk; this pulmonary autograft is used to reconstruct the aortic root, with subsequent placement of a cadaveric or composite graft to reconstruct the pulmonary arterial trunk. This technique is most frequently used in children with aortic root disease because the autograft is thought to have favorable hemodynamics, a lower risk of endocarditis and thrombogenicity, and a higher growth potential.
Intrinsic complications of the Ross procedure include dilation of the aortic root ( Fig. 24-15 ) with resultant valvular insufficiency, pseudoaneurysm formation, and ascending aortic dissection. All these complications are easily identified on CT or MRI, or both.

Aortic Valve-Sparing Procedures
Aortic valve-sparing procedures comprise a group of operations designed to preserve the aortic valve cusps in patients who have aortic root aneurysms with or without aortic insufficiency. This type of surgery is particularly useful in patients who have annuloaortic ectasia, in whom the aortic root is dilated but the aortic valve leaflets are normal. Several variations of this type of surgery are described in the literature, including the original supra-annular remodeling technique that was first performed by Yacoub and that keeps the aortic valve in situ. One of the most widely performed aortic valve-sparing surgical procedures was developed by David and Feindel. In this operation, the aneurysmal portion of the ascending aorta and sinuses of Valsalva are excised, but the aortic valve leaflets and some arterial wall are left attached to the left ventricular outflow tract. The aortic valve and the coronary arteries are then reimplanted inside a Dacron graft ( Fig. 24-16 ). These aortic valve-sparing surgical procedures recreate the aortic sinuses and sinotubular junction, which is thought to improve hemodynamics; furthermore, the procedures allow for nearly normal cusp motion.

The most common intrinsic complication of aortic valve-sparing procedures is the development of aortic insufficiency. This complication can be assessed and quantified with echocardiography or cardiac MRI. Aortic dissection and pseudoaneurysm formation have also been reported.
Surgical Procedures Involving the Aortic Arch
Any surgery involving the transverse aorta requires cerebral protection to prevent cerebral embolism or infarction. Many methods are used to maintain perfusion to the brain during aortic surgery, and these methods are beyond the scope of this chapter. In general, surgical procedures involving the aortic arch require the patient to undergo deep hypothermic circulatory arrest and either retrograde or antegrade cerebral perfusion.
Hemiarch Procedure
Disorders confined to the transverse aorta are exceedingly rare. Much more commonly, the aortic arch is involved in disease that extends from the ascending aorta into the descending aorta or that involves the entire thoracic aorta. When an ascending aortic aneurysm extends into just the proximal transverse aorta, thus sparing the arch vessels and distal transverse aorta, a hemiarch replacement may be performed. In this surgical procedure, the distal ascending aorta and proximal transverse aorta are removed; the remaining transverse aorta is beveled to leave the arch vessels intact. The graft that extends from the ascending aorta into proximal transverse aorta is then sewn onto the native aortic cuff.
Total Arch Replacement
Elephant Trunk Procedure
Patients with extensive aortic aneurysms that involve the ascending, transverse, and descending aorta require complex surgical reconstruction, of which the “elephant trunk” (ET) technique is a commonly used example. The ET technique was originally described by Borst in 1983 and has undergone modifications since its introduction. The ET procedure is a two-stage operation that eventually results in total arch replacement. The first stage consists of an ascending aortic interposition graft that extends across the transverse aorta and has a free-floating distal end; the free-floating distal end of the graft dangles within the native descending aortic lumen. The “elephant trunk” designation is derived from the appearance of the unattached distal end of the graft as it floats within the lumen of the native descending aorta. During the first stage procedure, the arch vessels must be relocated. Frequently, the arch vessels are debranched from the native transverse aorta and are reattached to a trifurcated synthetic graft, which, in turn, is anastomosed to the ascending aortic graft. In the second stage of the ET procedure, the descending aorta is repaired by either an open or an endovascular approach, and the unattached distal end of the graft is anastomosed to a descending aortic graft ( Fig. 24-17 ). When the second stage is performed by an endovascular approach, the combination of an open surgical first stage and an endovascular second stage is referred to as a hybrid ET procedure.