Classification
At present, there is no universally accepted thoracolumbar spine injury classification system. The ideal classification system would include a uniform methodology for injury description, a determination of stability, and facilitate clinical decision making.
Boehler published the first classification of thoracolumbar spine injuries in 1929.
3 Based on radiographic studies of World War I spine injury patients, together with mechanism of injury, five injury categories were described: compression fractures, flexion-distraction injuries, extension fractures, rotational injuries, and shear fractures. In 1938, Watson-Jones furthered Boehler’s work by advocating that the integrity of the posterior ligamentous complex (PLC) was necessary to maintain spinal stability.
4In 1970, Holdsworth introduced the “ column concept” of spinal stability, a biomechanical interpretation of injury mechanisms implied from radiographic studies.
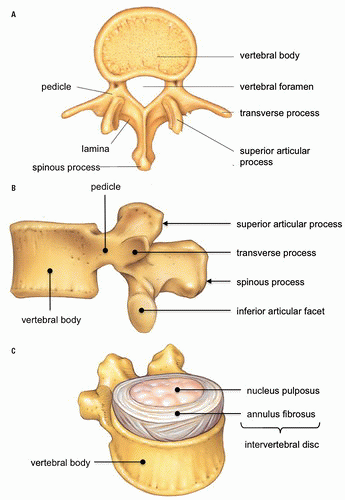
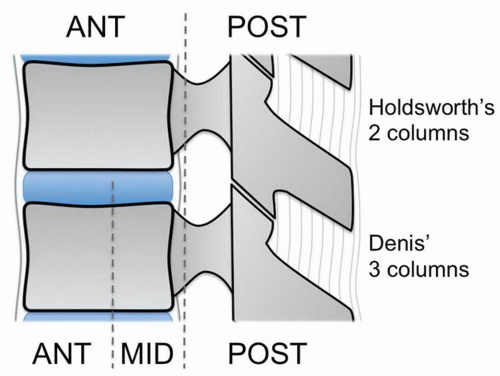
5 In his conception, the vertebra is divided into an anterior and posterior column (
Fig. 7.5). The anterior column consists of the vertebral body, intervertebral disk, anterior longitudinal ligament (ALL), and posterior longitudinal ligament (PLL). The posterior column comprises the facets, neural arch, and posterior ligament complex (interspinous and supraspinous ligaments, facet capsule, and ligamentum flavum). The integrity of the posterior column served as the major determinant of spinal stability. Holdsworth’s classification categorized thoracolumbar spine fractures into anterior compression fractures, fracture dislocations, rotational fracture dislocations, extension injuries, shear injuries, and burst fractures. According to Holdsworth, burst fractures were structurally stable as they were confined to the anterior column. Subsequent e xperimental studies
were unable to produce instability with only PLC disruption. Instability required, in addition to PLC disruption, rupture of the PLL and a portion of the annulus fibrosus.
Based on CT findings and newer experimental instability determinants, Denis modified the Holdsworth two-column model. In 1983, he published a review of 412 thoracolumbar spine injury patients and introduced the concept of the pivotal middle column defined as “the posterior longitudinal ligament, the posterior annulus fibrosus, and the posterior wall of the vertebral body” (
Fig. 7.5).
6 Consequently, Denis’ anterior column consists of “the anterior longitudinal ligament, the anterior annulus fibrosus, and the anterior part of the vertebral body.” The posterior column, as in Holdsworth’s model, is formed by the posterior bony arch and PLC.
Denis described four major types of spinal injuries along with their mechanisms: compression fractures, burst fractures, seat belt type (flexion distraction), and fracture-dislocations (
Table 7.2). Instability, according to the Denis’ three-column model, occurs with failure of two adjacent columns. The middle column represents the key to stability, as it fails either in association with the anterior column, the posterior column, or both. Denis also considered neurologic injury to be a marker of instability and used both mechanical and neurologic features to rate injury severity: first degree for isolated mechanical instability, second degree for isolated neurologic injury, and third degree for combined mechanical and neurologic instability.
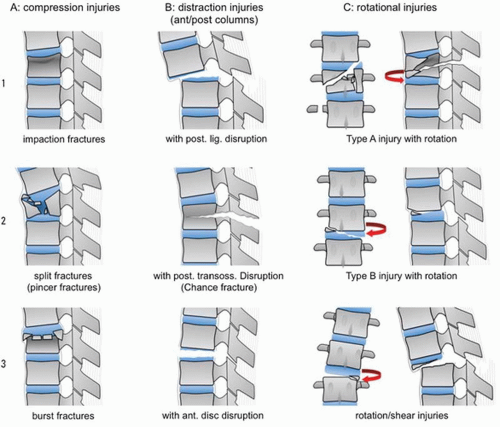
6The classification proposed by Magerl et al. in 1994 groups all thoracic and lumbar spine fractures into three primary types that have a progressive relationship to one another based on increasing severity of the fracture pattern and degree of soft tissue involvement (
Fig. 7.6).
7 This classification emphasizes the recognition and importance of ligamentous injury, particularly in the type B and C fractures.
Type A fractures are, in this schema, all the result of axial loading with or without an element of flexion. Type A fractures are limited to the vertebral body with loss of anterior vertebral body height but without posterior ligament complex injury or anterior translation. Type A fractures correspond to simple compression fractures due to hyperflexion.
Type B injuries involve both anterior and posterior columns and are associated with distraction of adjacent vertebrae due to ligamentous injury anteriorly (uncommon, hyperextension) or posteriorly (common, hyperflexion). In typical hyperflexion injuries, the posterior column injury is usually bony as in the Chance fracture or, less commonly, ligamentous as in the “soft tissue” Chance. Anterior translation is common in type B injuries.
Type C injuries include the characteristics of type B with the added element of rotation/shear and are by definition unstable. These injuries most closely correspond to the dislocations or fracture-dislocations of traditional classifications.
Each of these three main fracture types is divided into three groups, which are further divided into three subgroups, and finally into specifications (
Table 7.3). Together, the Magerl classification scheme is comprehensive, but also complex, as it catalogues 53 thoracolumbar injury patterns. Injuries are stratified from least severe A1 to most severe C3. No defined criteria for stability are inherent in the Magerl classification. In designing this classification, Denis’ three-column concept is abandoned in favor of Holdsworth’s two columns.
Stability
Predicting thoracolumbar spine fracture stability from an imaging study is difficult. Stability depends on the integrity of the vertebral bodies, including costal and sternal contributions in the thoracic segment, the ligaments, and joints of the spine. The practical definition of stability by White and Panjabi states that a stable spine is able to withstand physiologic loads without producing mechanical deformity or progressive neurologic injury or pain.
8 From both clinical and radiologic perspective, the three-column concept of Denis is most widely applied for determining thoracolumbar spine stability. According to Denis, failure of two or three columns yields instability, with disruption of the middle column representing the key contributing factor.
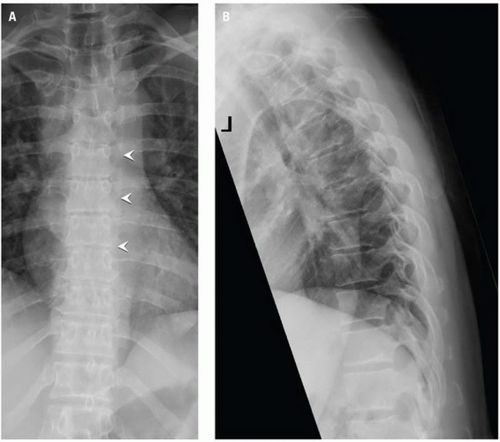
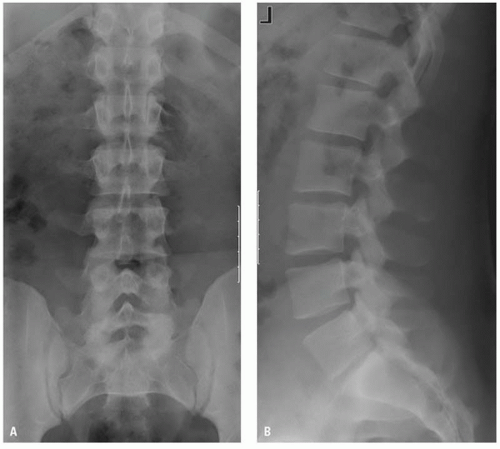
To simplify the imaging approach to stability, six radiologic signs of spinal instability
have been described: (1) displacement, (2) wide interspinous space, (3) abnormal facet joints, (4) posterior vertebral body line disruption, (5) wide interpediculate distance, and (6) wide intervertebral disk space (
Table 7.4). The presence of any one of these features indicates major injury to the supporting bone, ligaments, or joints and is felt to be sufficient to diagnose instability. Although originally described for radiographs, these features are applicable to, and in many cases, better seen with CT.
The common major fracture patterns described by Denis are compression, burst, flexion distraction (or Chance-type fractures), and fracture dislocations.