Table 7.1 Types of allergic reactions and associated allergic pulmonary diseases | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Patients to be admitted to the hospital because of asthma.
Suspected pneumonia or pneumothorax.
Before mechanical ventilation.
In cases of poor response to treatment.
If methotrexate treatment is intended.
Stage 1: Acute stage (initial manifestation with cough, fever, transient pulmonary infiltrates, and bronchial obstruction).
Stage 2: Remission of clinical and immunologic parameters.
Stage 3: Exacerbation.
Stage 4: Corticosteroid dependence.
Stage 5: Fibrosis.
lung fibrosis are observed as well. Radiologic findings (▶Table 7.4) can be distinguished as transient (▶Fig. 7.3) and chronic manifestations (▶Fig. 7.4).
Table 7.2 Radiologic findings in asthma | ||||||
|---|---|---|---|---|---|---|
|
|
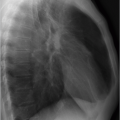
Acute hypersensitivity pneumonitis: Flu-like symptoms develop within a few hours after exposure to the allergen. If there is no further exposure to the allergen, the symptoms resolve within a few days. This stage is rarely seen on radiologic images since there is generally no indication for radiographic examination. If a radiograph has been obtained, it may show bilateral, more or less extensive, consolidation and small, rounded opacities(▶Fig. 7.5).11
Table 7.4 Radiologic findings in allergic bronchopulmonary aspergillosis
Transient findings
Chronic findings
Consolidation (often recurrence at same location)
Mucoid impaction (toothpaste or gloved finger sign)
Atelectasis
Pleural effusion
Central bronchiectasis
Fibrosis
Bronchoceles
Mycetoma (in particular in the middle fields)
Subacute hypersensitivity pneumonitis: The acute phase of the disease resolves within a few days. Then, or in the intervals between several acute flares, a discrete nodular pattern is seen on the radiograph (▶Fig. 7.6). The CT findings are virtually pathognomonic: multiple centrilobular groundglass nodules and diffuse ground-glass opacity or mosaic
pattern (▶Fig. 7.7). Occasionally, small cysts are observed as well. The findings can completely resolve in the absence of exposure to the allergen.

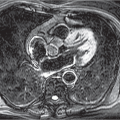
Fig. 7.3 Allergic bronchopulmonary aspergillosis. CT image. Transient findings with consolidation in right upper lobe (arrowheads); mucoid impaction in the left upper lobe (arrow).

Fig. 7.4 Allergic bronchopulmonary aspergillosis. CT images. Chronic findings. (a) Multiple areas of central bronchiectasis. (b) Besides, fibrosis (arrow) and → (arrowhead).
Chronic hypersensitivity pneumonitis: Long-lasting hypersensitivity pneumonitis can cause development of lung fibrosis (▶Fig. 7.8). If contact with the allergen persists, subacute and acute disease manifestations can coincide. While the latter entities are reversible, lung fibrosis secondary to chronic hypersensitivity pneumonitis is irreversible. This is characterized by restriction on pulmonary function tests. In radiologic findings, variable amounts of pulmonary fibrosis (honeycombing, intralobular lines, traction bronchiectasis) and ground-glass opacity are seen (▶Table 7.6). Unlike other forms of pulmonary fibrosis, chronic hypersensitivity pneumonitis is not associated with basal predominance. Likewise, there is little involvement of the costophrenic angles, whereas these are the main location affected by other forms of fibrosis (see Chapter 6). Imaging criteria for differential diagnosis are summarized in ▶Table 7.7.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree