Incidental splenic focal findings are commonly encountered in clinical practice and frequently represent a diagnostic dilemma due to nonspecific imaging features. Most are benign, particularly in patients without a history of malignancy and without symptoms of fever, weight loss, or left upper quadrant or epigastric pain. Incidental malignant splenic processes are exceedingly rare. This article reviews imaging characteristics of incidental focal splenic findings, and proposes a practical approach for management of such findings, which can prevent unnecessary workup and its related drawbacks in clinical practice.
Key points
- •
Despite overlapping imaging features among benign and malignant splenic processes, certain splenic focal findings have unique imaging features that can lead to a definitive diagnosis or appropriate differential diagnosis.
- •
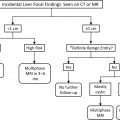
Incidental indeterminate splenic findings in patients with a history of malignancy or symptoms (epigastric or left upper quadrant pain, type B symptoms, immunocompromised) require further imaging follow-up or evaluation by MR imaging, PET/computed tomography, or tissue sampling.
- •
Incidental indeterminate splenic findings in patients without a history of malignancy or symptoms pose an exceedingly low risk for malignancy (1%). Patients with an incidental malignant mass in the spleen almost always have additional imaging findings that allow for a diagnosis of malignancy to be made. Therefore, no follow-up or evaluation is required if no additional concurrent imaging findings worrisome for malignancy are detected.
Introduction
With the increased use of cross-sectional imaging for the evaluation of a wide spectrum of clinical presentations, the discovery of incidental findings has become more common. Previously reported rates of incidental findings within the abdomen and pelvis range from 35% to 56% on computed tomography (CT) performed in the emergency department in the setting of trauma. , These findings include focal processes in the spleen, which frequently present a diagnostic dilemma as imaging features of benign and malignant entities demonstrate substantial overlap. , Consequently, the evaluation of incidentally discovered splenic focal findings relies heavily on clinical context as opposed to being primarily imaging based. Fortunately, most incidentally detected splenic focal findings are benign and of no clinical significance. Unwarranted workup or inappropriate follow-up for such findings, however, can lead to increased health care costs and expose patients to unnecessary procedures, and result in both physical risk and emotional stress.
In this article, we focus on incidental focal splenic findings that radiologists may encounter in their usual clinical practice. A practical and simplified approach to the management of incidental splenic focal findings discovered on CT or MR imaging are described, incorporating both imaging features and clinical context.
Incidental focal splenic findings
A number of focal splenic findings can be seen incidentally on CT or MR imaging. These can be broadly grouped into non-neoplastic and neoplastic, which can be further subdivided into benign and malignant entities. Understanding the typical imaging features of more commonly encountered focal splenic processes can help guide the need for further assessment or follow-up imaging.
Non-neoplastic Masses
Nonparasitic cyst
Splenic cysts can be either congenital (true cyst) or false (posttraumatic or secondary cyst). Congenital cysts are lined by epithelial cells that are thought to derive from peritoneal mesothelial cells. , False cysts, on the other hand, contain a fibrous lining and are more common than true cysts, representing 80% of all nonparasitic splenic cysts. False cysts tend to be smaller and more commonly exhibit mural calcifications compared with true cysts. Both types of cysts may be asymptomatic at the time of discovery, but a prior history of trauma can be extremely helpful in diagnosing a false cyst.
On imaging, splenic cysts typically present as well-circumscribed, homogeneous, simple fluid-containing masses. They are hypodense on CT (<10 HU) without internal or rim enhancement. Similarly, splenic cysts are homogeneously hypointense on T1-weighted images, and hyperintense on T2-weighted MR images, without enhancement on postcontrast sequences. Although the presence of thick rim calcification can differentiate a false cyst from a true cyst on imaging ( Fig. 1 ), distinction between these 2 entities is often of no clinical significance.

Abscess
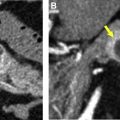
Bacterial infection in the spleen can lead to development of a pyogenic abscess. Hematogenous spread from infection of other organs is the most common cause for splenic pyogenic abscess. , Patients with a pyogenic abscess tend to be symptomatic with fever, leukocytosis, and left upper quadrant pain and, hence, these are usually not truly incidental. On both CT and MR imaging, a pyogenic abscess may present as a single cystic process, or be multiple, usually unilocular with internal fluid attenuation or signal intensity with a thick, irregular and enhancing wall. Similar to pyogenic abscesses in other organs, a splenic pyogenic abscess can contain air ( Fig. 2 ) and various amount of internal debris, resulting in increased internal heterogeneity.

Compared with bacterial infections, mycobacterial and fungal infections usually appear as multifocal or miliary abscesses within the spleen. Patients with splenic mycobacterial or fungal infection may be immunocompromised and exhibit moderate splenomegaly with multiple to innumerable nodules that are smaller than 1 cm, although micronodules may not be apparent on imaging. These foci are usually hypodense on CT without substantial internal or rim enhancement. On MR imaging, mycobacterial nodules are typically isointense on precontrast T1-weighted images and hypointense on T2-weighted images, with peripheral enhancement. Fungal microabscesses appear hypointense on T1-weighted sequences and hyperintense on T2-weighted images, and may demonstrate peripheral enhancement.
Parasitic cyst
Parasitic infection of the spleen by echinococcus can present with distinct imaging features that aid in its diagnosis. On both CT and MR imaging, hydatid cysts present as well-circumscribed cysts that may contain multiple peripheral smaller daughter cysts. The cyst contents are usually of fluid density or signal intensity. Hydatid sand and debris within the cyst may cause the cyst to be hyperdense on CT and hypointense on T2-weighted MR images. On MR imaging, daughter cysts tend to have lower signal intensity than the mother cyst on T1-weighted images. A thick hypointense rim on T2-weighted images surrounding the mother cyst can be seen, and is thought to represent collagen-rich material deposited by the host’s response to the cyst. , Both the mother cyst wall (pericyst) and the collapsed internal parasitic membrane can calcify. , The cysts do not demonstrate enhancement after intravenous (IV) contrast administration.
Sarcoidosis
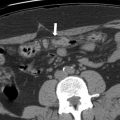
In patients with sarcoidosis, splenic involvement can be seen in 24% to 59% based on studies using fine needle splenic aspiration. , Patients with splenic sarcoidosis are usually asymptomatic, but can present with abdominal pain, fever, malaise, or rarely even splenic rupture. On imaging, splenic sarcoidosis can manifest with splenomegaly and diffuse homogeneous or nodular involvement. Abdominal lymphadenopathy is frequently visualized. Although the presence of intrathoracic findings of sarcoidosis can substantially aid in establishing the diagnosis of splenic sarcoidosis, chest radiographs have been reported to be normal in a quarter of patients with sarcoidosis presenting with splenomegaly or splenic nodules. Sarcoidosis nodules are hypodense and hypoenhancing on CT. On MR imaging, these nodules are hypointense on all sequences, with minimal enhancement on postcontrast images , ( Fig. 3 ).

Neoplastic Masses
Benign masses
Hemangioma
Hemangioma is the most common primary neoplasm of the spleen, with incidence ranging from 0.3% to 14% on autopsy series. The mass is characterized as a focal proliferation of blood vessels ranging from capillary to cavernous in size. Splenic hemangiomas can be solitary or multiple. Most patients are asymptomatic with the hemangioma or hemangiomas found incidentally; however, large hemangiomas may rarely cause hemorrhage, rupture, anemia, thrombocytopenia, or high-output heart failure.
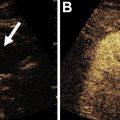
The appearance of splenic hemangiomas on noncontrast CT depends on the size of the blood vessels within, ranging from homogeneously hypodense or isodense in capillary hemangiomas, to heterogeneously hypodense and isodense in cavernous hemangiomas. , After intravenous contrast administration, capillary hemangiomas demonstrate avid homogeneous enhancement, whereas cavernous hemangiomas demonstrate heterogeneous enhancement on late to delayed-phase images. , Calcifications also can be seen. ,
On MR imaging, splenic hemangiomas are hyperintense on T2-weighted images and hypointense on precontrast T1-weighted images compared with splenic parenchyma. On postcontrast T1-weighted images, splenic hemangiomas demonstrate either homogeneous early and persistent enhancement or early peripheral enhancement that progresses centripetally or homogeneously on delayed phases , , ( Fig. 4 ). The classic peripheral nodular centripetal enhancement seen in hepatic hemangiomas may be difficult to appreciate in splenic hemangiomas due to the avidly enhancing background splenic parenchyma.

Hamartoma
Splenic hamartoma is an abnormal growth of histologically normal cells in the spleen. It consists almost entirely of red pulp. Previous autopsy series demonstrate an incidence of 0.024% to 0.13%. Similar to splenic hemangiomas, hamartomas rarely cause symptoms and may present as a solitary mass or multiple masses.
Splenic hamartoma demonstrates imaging characteristics similar to focal nodular hyperplasia in the liver. On CT, it appears hypodense to isodense on noncontrast CT. Rarely, calcification within a splenic hamartoma has been reported. , On IV contrast-enhanced CT, splenic hamartomas demonstrate heterogeneous avid hyperenhancement on the early arterial phase. The enhancement may become more uniform on delayed postcontrast phases, blending in with background splenic parenchyma. On MR imaging, splenic hamartomas are isointense on precontrast T1-weighted images, and isointense or mildly hyperintense on T2-weighted images compared with background splenic parenchyma ( Fig. 5 ). Appearance on postcontrast T1-weighted images is similar to postcontrast CT.

Lymphangioma
Lymphangioma is a benign malformation of lymphatic channels, generally more common in children, with reported 10% of pediatric lymphangiomas involving visceral organs. Lymphangiomas in other organs are frequently present when splenic lymphangioma is identified. Differentiation among capillary, cavernous, or cystic subtypes is based on the size of the lymphatic channels.
Splenic lymphangiomas present as a solitary cystic mass or as multiple well-circumscribed cystic masses, which may be multilocular with multiple thin septations. On precontrast CT, splenic lymphangiomas measure simple fluid density. Density of the fluid may increase as proteinaceous or hemorrhagic contents accumulate. On noncontrast MR imaging, lymphangiomas are typically homogeneously hypointense on T1-weighted imaging and hyperintense on T2-weighted imaging ( Fig. 6 ). The signal intensity of lymphangiomas, however, can vary on T1-weighted and T2-weighted images depending on the presence of proteinaceous and hemorrhagic contents, which may increase the signal intensity on T1-weighted images, and correspondingly decrease the signal intensity on T2-weighted images. On postcontrast CT and MR imaging, splenic lymphangiomas demonstrate no or minimal enhancement of the cyst wall or of the septations.

Littoral cell angioma
Littoral cell angioma is a rare, benign neoplasm of the spleen that consists of numerous nodules that are made of various-sized vascular channels. These vascular channels contain blood products of various ages, resulting in red to brown color on gross pathologic examination. Littoral cells, which line the splenic sinuses of the red pulp and demonstrate immunohistochemical features for both endothelial and histiocytic cells, are thought to give rise to the mass. Clinically, littoral cell angioma may present as an incidental finding or with splenomegaly. No gender predilection has been reported. Association with other neoplasms has been reported despite the benignity of littoral cell angioma.
On CT, littoral cell angioma may appear as a solitary mass or multiple, usually similar-sized masses ranging from smaller than a centimeter, to 6 cm. Although it is a circumscribed mass, littoral cell angioma is not encapsulated. The mass appears isodense to the splenic parenchyma on noncontrast CT, and is hypoattenuating on the portal venous phase. On MR imaging, it may manifest as marked hypointense masses on both precontrast T1-weighted and T2-weighted images due to hemosiderin deposition within the nodules, although signal intensity on T2-weighted images may be heterogeneously hyperintense. Peripheral arterial hyperenhancement with delayed centripetal filling on postcontrast MR images has been reported ( Fig. 7 ).