Infections and Inflammations of Bones
Lee F. Rogers
Martha A. Norris
L. F. Rogers: Department of Radiology, Wake Forest University School of Medicine, Winston-Salem, North Carolina 27157. M. A. Norris: Department of Radiology, University of Wisconsin Hospital and Clinics, Madison, Wisconsin 53792-3252.
OSTEOMYELITIS
Osteomyelitis was once a common, devastating, often crippling, and much-feared disease. Since the advent of antibiotics, it has become manageable, less common, and much less serious. The general improvement in personal hygiene, greatly improved surgical antisepsis, and early antibiotic treatment of lesions that predispose to septicemia have resulted in an appreciable reduction in the incidence of osteomyelitis.
Infections of bone have been conveniently divided into three categories reflecting the source of the infection14: (1) hematogenous osteomyelitis; (2) implantation osteomyelitis caused by bacteria implanted or introduced with an open fracture, penetrating wound, or surgical procedure; and (3) secondary osteomyelitis with the bone involvement secondary to a contiguous focus of soft-tissue infection related to peripheral vascular disease. Osteomyelitis may also be divided into acute, subacute, and chronic forms, depending on the virulence of the organism, the response of the host, and the effectiveness of antibiotic treatment.
Staphylococcus aureus is the offending organism most frequently identified. In children, in whom hematogenous infection is the rule, multiple foci of disease are relatively common, whereas in adults the infection is usually limited to a single focus. The cause is usually established by obtaining a positive blood culture, a culture from an aspiration of the adjacent joint, or a direct aspiration of the involved bone or overlying soft tissues. Early recognition and treatment with antibiotics may minimize the radiographic findings of osteomyelitis.
Pathogenesis
Hematogenous Osteomyelitis
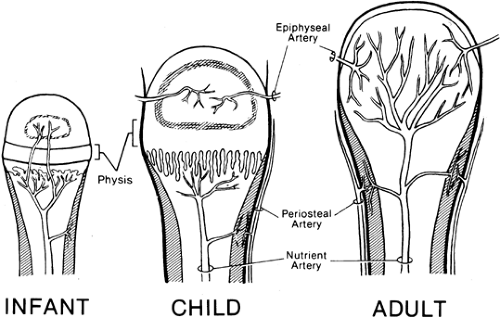
The source of bacteria in the hematogenous form is usually infections of the skin, boils or carbuncles, insect bites, infected abrasions, or, less commonly, infections of the respiratory tract. The offending organism is usually S. aureus, less commonly Streptococcus, Haemophilus influenzae, or pneumococcus. The organisms enter the bloodstream and become entrapped in the terminal vascular networks of long bones, the site and consequences depending on the age of the patient (Fig. 5-1). In childhood, these networks are located in the metaphysis just beneath the physis, and therefore the infections of childhood are most often located in and limited to the metaphyseal ends of long bones, particularly the femur and tibia14,21 (see Figs. 5-4 and 5-5). Involvement of adjacent joints is rare. Terminal vascular networks are also located in the epiphysis, but isolated infections of the epiphysis are much less common than those in the metaphysis.17 In contrast, in infants younger than 1 year of age, the vascular network commonly crosses the growth plate from the metaphysis to the epiphysis; therefore, infections in infancy are more likely to originate within the epiphysis or to extend quickly from the metaphysis into the epiphysis and then into the adjacent joint.14,21 Extension of the infection into the adjacent joint is much less likely after the age of 1½ years, except in the hip, where the metaphysis is located within the joint capsule. After the closure of the epiphysis, the terminal blood supply is located in the end of the bone. Therefore, in adults, the hematogenous infections occur at the end of the bone and may extend into the adjacent joint space. However, primary hematogenous osteomyelitis of long bones is uncommon in adults. Adults are more likely to have vertebral osteomyelitis or suppurative spondylitis, often secondary to infection or manipulation of the urinary tract.
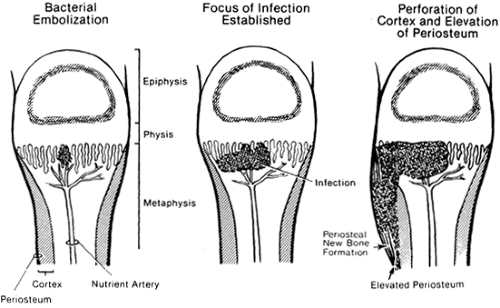
The infectious process begins in the intramedullary portion of the bone, eventually leading to the destruction
of the trabeculae, penetration of the overlying cortex through vascular foramina, elevation of the periosteum, and extension into the overlying soft tissues (Fig. 5-2).
of the trabeculae, penetration of the overlying cortex through vascular foramina, elevation of the periosteum, and extension into the overlying soft tissues (Fig. 5-2).
The periosteum is easily elevated by the extension of pus through the cortex. Because the periosteum is tightly bound to the perichondrium of the physis or growth plate, the periosteum is preferentially stripped or elevated from the metaphysis toward the diaphysis, often well beyond the extent of involvement of the intramedullary bone or marrow. The tight bond between the periosteum and perichondrium at the physis prevents extension of pus into the epiphysis or adjacent joint except at the hip, where the metaphysis lies within the joint. In contrast to that in children, the periosteum in adults is tightly adherent to the cortex and much less easily stripped. Therefore, in adults, periosteal elevation is not as marked, the extent of periosteal stripping is more limited, and involucrum formation is uncommon.
Implantation Osteomyelitis
Implantation osteomyelitis is caused by bacteria introduced into the soft tissues and bone by a penetrating wound, surgical procedure, or open fractures and dislocations (see Fig. 5-8). Blood clot, necrotic marrow, muscle, and other soft tissues provide an excellent culture medium for the localization and colonization of pathogenic bacteria. S. aureus is a common offending organism, but other gram-positive organisms such as Streptococcus and gram-negative organisms such as Pseudomonas, Proteus, or Escherichia coli may be involved.
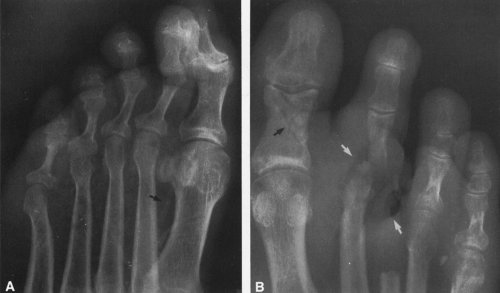
Secondary Osteomyelitis
Osteomyelitis associated with vascular insufficiency is almost always encountered in the diabetic patient and localized to the foot, affecting the phalanges and metatarsals (see Fig. 5-16). Infection of bone is always secondary to an overlying cellulitis or deep penetrating ulcer of the skin. The most common offending organism is S. aureus or Streptococcus, although gram-negative bacterial infections are also encountered.
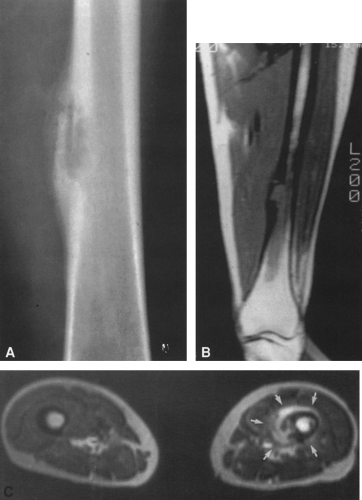
 FIG. 5-13. Chronic osteomyelitis. Cortical thickening and sclerosis involve the entire shaft, particularly distally. Some ovoid radiolucencies can be seen within the thickening. |
Infections of bone are discussed in this chapter. Infections of joints and infectious spondylitis are detailed in Chapter 3.
RADIOGRAPHIC FINDINGS IN ACUTE OSTEOMYELITIS
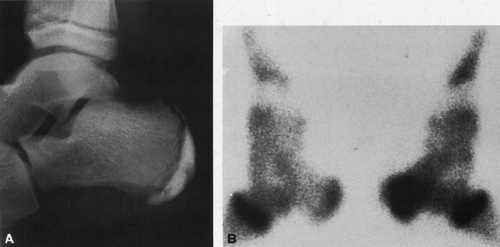
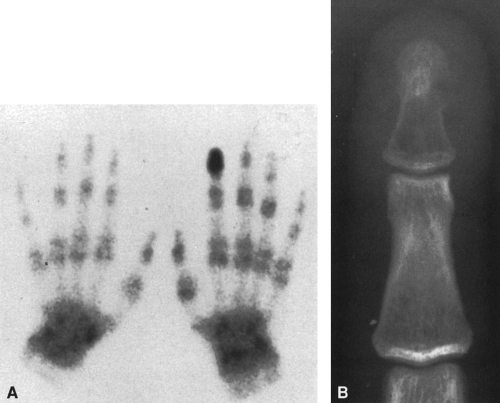
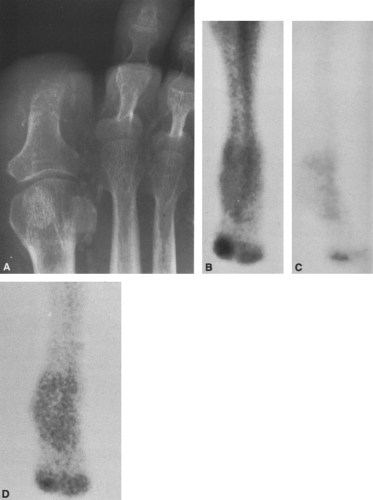
In acute osteomyelitis there is a latent period of 10 to 12 days between the time of onset of clinical symptoms and the development of definite radiographic changes in bone.14 Because it is essential that adequate therapy be instituted as early as possible, one should not wait for the development of radiographic evidence of disease before instituting appropriate treatment. Radioisotopic bone scanning is very sensitive to the changes of osteomyelitis, revealing areas of increased radioactivity at sites of infection well before there is any plain film radiographic sign of disease (Fig. 5-3). A bone scan is warranted in every case of clinically suspected osteomyelitis in which the radiographs are unrevealing.
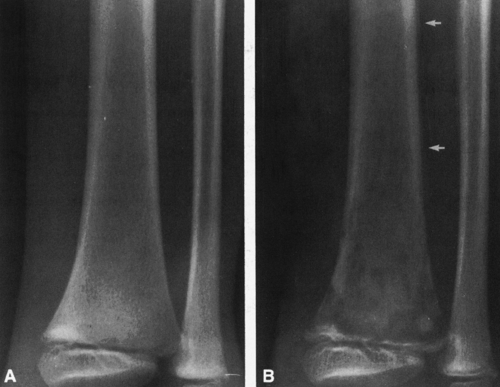
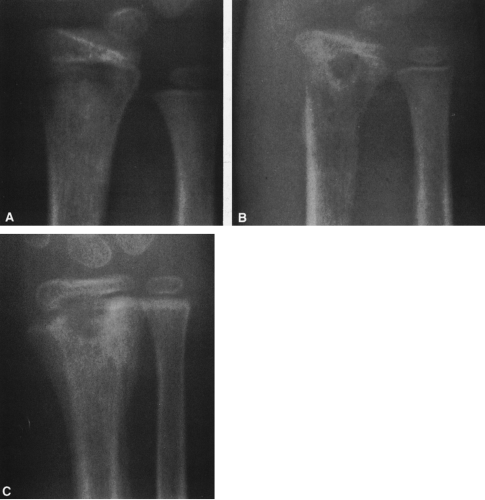
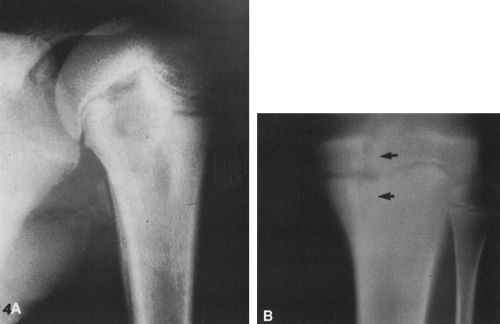
The first radiographic evidence of disease is the swelling of soft tissues, characteristically deep and adjacent to bone (Fig. 5-4; see Fig. 5-3A). The early swelling is recognized
because of displacement or obliteration of the normal fat planes adjacent to and beneath the deep muscle bundles. At first the superficial fatty layer is unaffected. In contrast, with skin infection, soft-tissue swelling is superficial and does not involve the deeper tissues adjacent to the bone. The first evidence of disease in the bone is usually an area of indefinite rarefaction or destruction in the metaphysis (Figs. 5-5 and 5-6). The area of destruction is poorly defined and has a fine, granular, or slightly mottled appearance. Associated with this or even at times preceding it is a minimal amount of periosteal new-bone formation laid down parallel to the outer margin of the cortex. The limits of the bone destruction remain poorly defined throughout the acute stage. The actual disease process is usually much more extensive than demonstrated by the radiograph.
because of displacement or obliteration of the normal fat planes adjacent to and beneath the deep muscle bundles. At first the superficial fatty layer is unaffected. In contrast, with skin infection, soft-tissue swelling is superficial and does not involve the deeper tissues adjacent to the bone. The first evidence of disease in the bone is usually an area of indefinite rarefaction or destruction in the metaphysis (Figs. 5-5 and 5-6). The area of destruction is poorly defined and has a fine, granular, or slightly mottled appearance. Associated with this or even at times preceding it is a minimal amount of periosteal new-bone formation laid down parallel to the outer margin of the cortex. The limits of the bone destruction remain poorly defined throughout the acute stage. The actual disease process is usually much more extensive than demonstrated by the radiograph.
In a short time, bone destruction becomes more prominent, causing a ragged, moth-eaten appearance of the medullary bone, with foci of destruction intermingled with areas of apparently more or less normal bone. Periosteal new-bone formation is more pronounced, and both the periosteal reaction and intramedullary destruction extend into the diaphysis (see Fig. 5-6). In the neonate, the infection commonly extends to the overlying joint, forming a suppurative arthritis (Fig. 5-7; see Figs. 3-5 and 3-6).
In the phalanges and other small bones there is little or no periosteal reaction. Bone is simply dissolved (see Fig. 5-16).
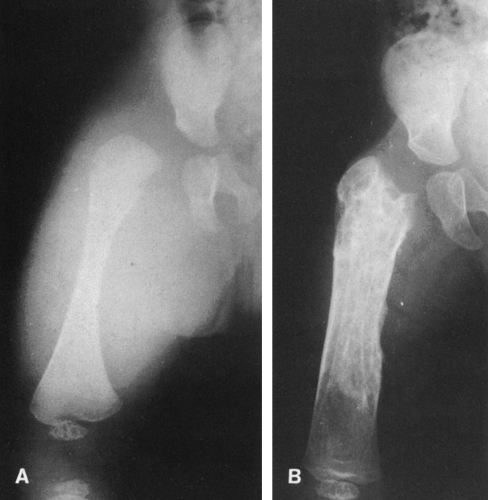
At times this proceeds internally, hollowing or shelling out the bone by destroying intramedullary trabeculae, leaving only a thin rim of cortex (Fig. 5-8).
At times this proceeds internally, hollowing or shelling out the bone by destroying intramedullary trabeculae, leaving only a thin rim of cortex (Fig. 5-8).
Radioisotopic Bone Scanning
Technetium-99m radiophosphate (see Figs. 5-3 and 5-8), gallium-67 citrate, and indium-111 leukocytes have been used to diagnose osteomyelitis and to differentiate osseous infections from those limited to the soft tissues (e.g., cellulitis).15,16 To distinguish skeletal from soft-tissue infection, a triple-phase 99mTc radiophosphate scan is performed (see Fig. 5-17). The three phases are perfusion, blood pool, and delayed images. Acute osteomyelitis is characterized by enhanced activity in the blood pool and delayed bone images, whereas septic arthritis and cellulitis demonstrate increased activity in the blood pool phase but normal or only slightly increased uptake in the delayed image. Sequential radiophosphate and gallium scanning may also be used, because increased radiophosphate uptake is nonspecific, occurring in areas of high bone turnover from whatever cause—fracture, infection, metabolic, or tumor. Gallium-67 uptake is more specific for infection. Indium-111 leukocytes deposit wherever there is an active migration of white cells, and therefore this examination is also more specific for infection.16
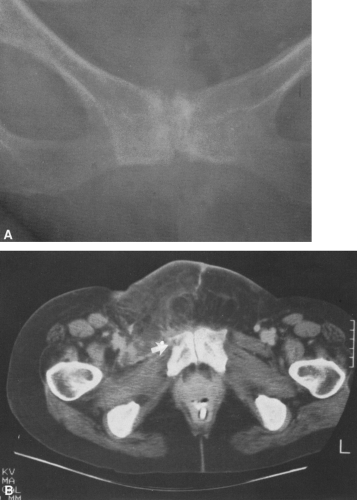
Computed Tomography
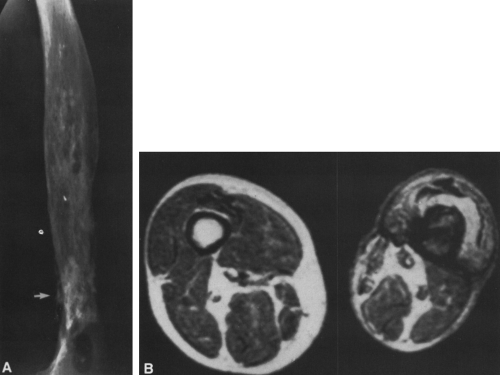
Computed tomography (CT) is a useful adjunct in the evaluation of osteomyelitis.5,7 Increased attenuation occurs within the bone marrow early in the disease, before plain film changes and simultaneously with increased radioisotopic activity. The increased attenuation is caused by the presence of edema and pus, which replaces the fat within the marrow. The attenuation of normal marrow fat is on the order of −80 to −100 Hounsfield units, increasing in
the presence of an infection to −10 Hounsfield units or higher, well within the positive range. This is similar in appearance to infiltration by tumors (see Fig. 4-43 in Chapter 4). Small bubbles of intraosseous gas may be seen within the intramedullary canal as a result of infection by gas-forming organisms. CT demonstrates to good advantage cortical destruction and associated soft-tissue changes (Fig. 5-9). Fat-fluid (pus) levels have been reported to occur within the medullary canal and adjacent bursae. CT is also advantageous in the evaluation of chronic osteomyelitis,5 allowing the detection and localization of bony sequestra, the demonstration of cortical defects leading to subcutaneous sinus tracts, and the identification of adjacent soft-tissue abscesses. Abscesses appear as sharply defined areas of low density within surrounding muscle or subcutaneous tissue.
the presence of an infection to −10 Hounsfield units or higher, well within the positive range. This is similar in appearance to infiltration by tumors (see Fig. 4-43 in Chapter 4). Small bubbles of intraosseous gas may be seen within the intramedullary canal as a result of infection by gas-forming organisms. CT demonstrates to good advantage cortical destruction and associated soft-tissue changes (Fig. 5-9). Fat-fluid (pus) levels have been reported to occur within the medullary canal and adjacent bursae. CT is also advantageous in the evaluation of chronic osteomyelitis,5 allowing the detection and localization of bony sequestra, the demonstration of cortical defects leading to subcutaneous sinus tracts, and the identification of adjacent soft-tissue abscesses. Abscesses appear as sharply defined areas of low density within surrounding muscle or subcutaneous tissue.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) has proved to be more sensitive than standard radiography, conventional tomography, or CT in the evaluation of osteomyelitis.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree