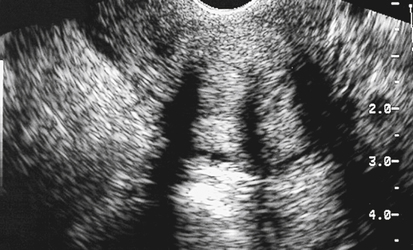
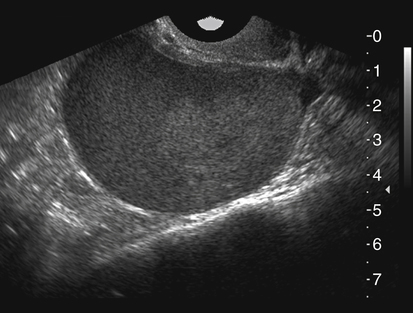
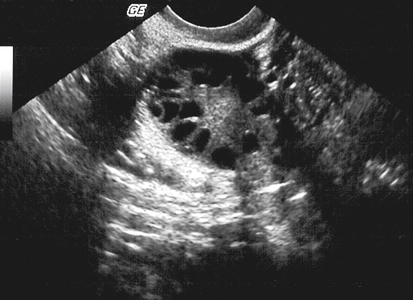
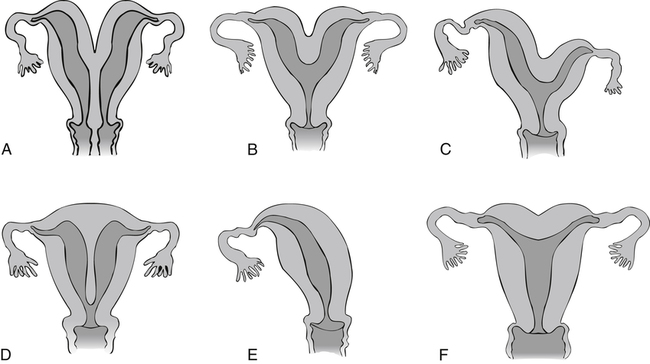
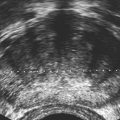
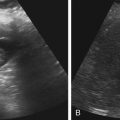
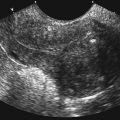
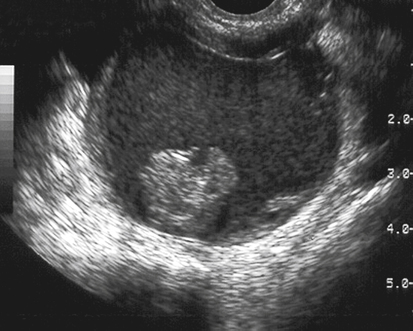
• List and describe the ovarian factors that can lead to infertility. • Differentiate the sonographic appearances of ovarian causes of infertility. • Describe the normal embryologic development of the uterus. • Identify various congenital uterine anomalies. • Describe the sonographic features that differentiate the types of congenital uterine anomalies. • Discuss the role of sonography in evaluating the ovaries and endometrium during assisted reproductive technology procedures. This chapter discusses factors linked with infertility that may be identified sonographically. The most common ovarian factors linked with infertility are explored, and differentiations of congenital uterine anomalies are discussed. Tubal factors associated with infertility are discussed in Chapter 15. Endometriosis is the result of functioning endometrial tissue being located outside the uterus. The condition is hormonally stimulated during the reproductive years and can affect 25% to 35% of infertile women.1,2 Besides infertility, symptoms of endometriosis include pelvic pain, dyspareunia, abnormal uterine bleeding, and dysmenorrhea; however, some patients may be asymptomatic. Endometriosis can be localized or diffuse. The ovaries are the most common place for endometriosis to occur, although endometrial implants may be located anywhere in the body. Endometriosis can be treated medically, with hormones or hormone suppression therapy, or surgically, depending on the extent of disease and the desired outcome. The purpose of treatment may be to decrease or alleviate symptoms of pain associated with endometriosis or to improve the chances of pregnancy with removal of endometrial implants that may be impeding ovulation or obstructing fallopian tubes. Surgery is the better option if endometriosis is moderate to severe, although recurrence of the disease is possible. Patients who no longer desire fertility may elect hysterectomy and bilateral salpingo-oophorectomy to decrease symptoms of the disease. The localized form of endometriosis, endometrioma, appears as a mass involving the ovary and is also known as a chocolate cyst. The classic sonographic appearance is a well-defined, thin-walled mass containing low-level, internal echoes with through transmission. Endometriomas can be unilocular or multilocular and are frequently multiple in number. Other sonographic appearances include masses with thick walls, internal septations, or fluid/debris levels in the dependent portion of the lesion (Figs. 16-3 to 16-8). Endometriomas are most easily characterized transvaginally with better definition of the degree of internal echoes compared with transabdominal scanning. Endometrioma is also discussed in Chapter 17. Polycystic ovarian syndrome (PCOS) is an endocrine disorder that produces anovulation and results in infertility. Women with PCOS often have high levels of androgen hormones and may be resistant to the effect of insulin. Among women with PCOS, 80% are obese and are at risk for development of diabetes.3,4 PCOS is a cause for infertility in approximately 6% of women of reproductive age. Clinical symptoms include infertility, early pregnancy loss, hirsutism, acne, and amenorrhea; however, some patients with PCOS have no symptoms. The diagnosis is generally made with evaluation of the clinical presentation and hormone levels; sonographic criteria also are helpful in confirming the condition (Box 16-1). In addition, patients with PCOS may incur the risks associated with unopposed estrogen and may be monitored for endometrial carcinoma and breast cancer. Sonographic examination of PCOS may reveal bilateral ovaries that contain multiple small follicles. The follicles are usually located in the periphery of the ovary and are 0.5 to 0.9 cm in size. The follicles produce a sonographic appearance of a “string of pearls” (Figs. 16-9 and 16-10). The ovaries also have an increase in stromal echogenicity (Fig. 16-11). The size of the ovaries may be normal or enlarged. Sonographic criteria for diagnosis of PCOS include presence of 12 or more follicles measuring 2 to 9 mm or increased ovarian volume greater than 10 mL.3,4 Congenital uterine anomalies can be a contributing factor in infertility and adverse pregnancy outcomes. The uterus and fallopian tubes develop from paired müllerian ducts that fuse, and then the uterine septum formed from the fusion is reabsorbed. Development of the uterus occurs between 7 and 12 weeks of gestation.5 Anomalies that occur may be caused by failure of development of one or both of the müllerian ducts (uterine agenesis, unicornuate uterus), failure of fusion of the müllerian ducts (uterus didelphys, bicornuate uterus), or failure of the sagittal septum to reabsorb (Fig. 16-12). Septate uteri are associated with infertility, miscarriage, preterm birth, and fetal malpresentation (e.g., breech). Unicornuate, bicornuate, and didelphic uteri are associated with preterm birth and fetal malpresentation.6 The sonographic appearance of uterus didelphys is of two separate endometrial echo complexes. A deep fundal notch is present, separated widely with a full complement of myometrium (Figs. 16-13 to 16-16). Two cervices and vaginas should be visualized. The initial impression of uterus didelphys may suggest a normal uterus with an adjacent pelvic mass, especially if the uteri are asymmetric. This appearance is related to an obstructed hemivagina causing hematocolpos or hematometracolpos.
Infertility
Endometriosis
Sonographic Findings
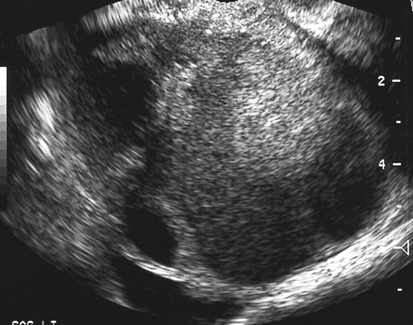


Polycystic Ovarian Syndrome
Sonographic Findings

Congenital Uterine Anomalies
Uterus Didelphys
Sonographic Findings

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Infertility