Fig. 11.1
Crohn’s disease: longitudinal ulcer. Long and linear ulcers (arrows) parallel to the mesenteric border
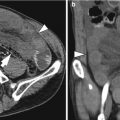
11.5.2 Crohn’s Disease: Cobblestoning Appearance – Small Bowel Follow-Through Findings
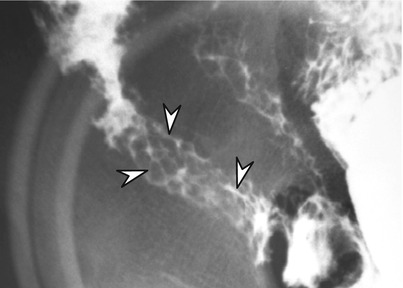
Fig. 11.2
Advanced stage of active inflammatory Crohn’s disease in a 14-year-old man. Spot radiograph from a small bowel follow-through shows the classic cobblestoning appearance in the terminal ileum. Multiple linear ulcerations (arrowheads) and polypoid elevation of remaining mucosa can produce the cobblestoning appearance
11.5.3 Crohn’s Disease: Cobblestoning Appearance – MR Enterography Findings
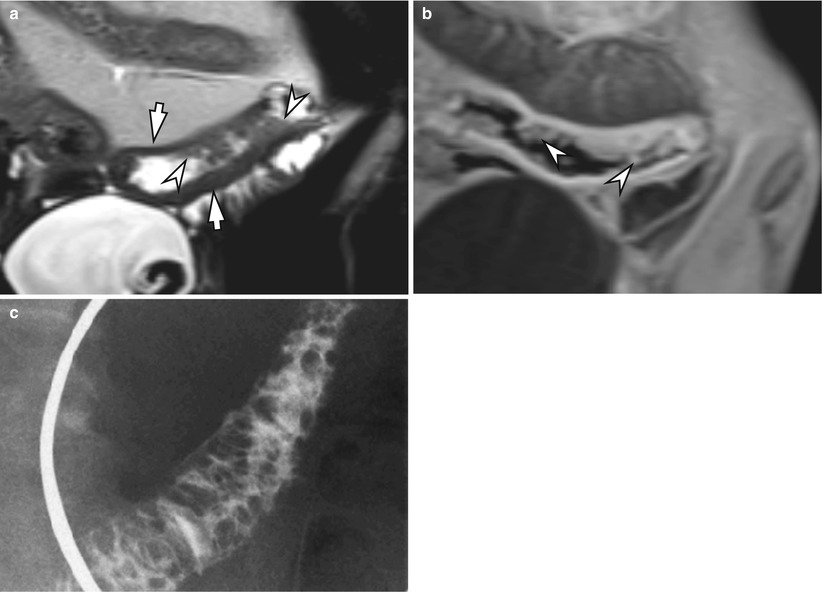
Fig. 11.3
Cobblestoning appearance in the small bowel in a 16-year-old man with Crohn’s disease. (a) Coronal T2-weighted HASTE image of the small bowel shows mural thickening (arrows) and multiple pseudopolyps (arrowheads). (b) Contrast-enhanced T1-weighted image shows transmural enhancement of the small bowel and multiple pseudopolyps (arrowheads). (c) Small bowel follow-through of the same patient reveals classic cobblestoning appearance
11.5.4 Crohn’s Disease: Pseudopolyp
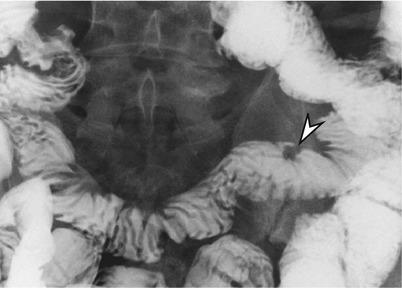
Fig. 11.4
Pseudopolyp (arrowhead) in the ileum in a 56-year-old main with long-standing Crohn’s disease
11.5.5 Crohn’s Disease: Asymmetric Wall Involvement
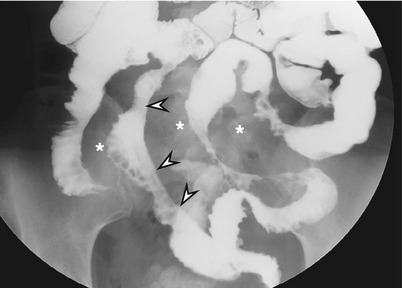
Fig. 11.5
Crohn’s disease: asymmetric wall involvement. Spot radiograph of a small bowel follow-through shows multi-segmental involvement of Crohn’s disease. Note the shortening and straightening of mesenteric border of the small bowel segment (arrowheads) with multiple pseudosacculation formation on the antimesenteric border. Note the widely separated loops of bowel due to fibrofatty proliferation (asterisks)
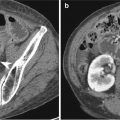
11.5.6 Crohn’s Disease: Antimesenteric Pseudosacculation
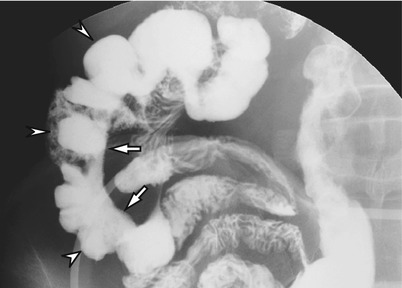
Fig. 11.6
Crohn’s disease: antimesenteric pseudosacculation. Note the straightening of the mesenteric border (arrows) of the terminal ileum. There are multiple pseudosacculations (arrowheads) in the antimesenteric border
11.5.7 Crohn’s Disease: Enteroenteric Fistula
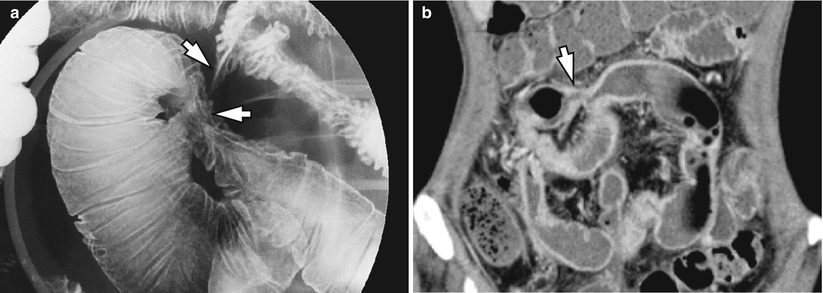
Fig. 11.7
Crohn’s disease: enteroenteric fistula. (a) Spot radiograph from an enteroclysis in a 33-year-old man with Crohn’s disease demonstrates multiple ileoileal fistulae (arrows). (b) Coronal reformatted image from a CT enterography of another patient with Crohn’s disease shows a fistulous tract (arrow) filled with neutral oral contrast
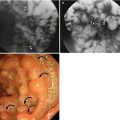
11.5.8 Crohn’s Disease: Involvement of the Ileocecal Area
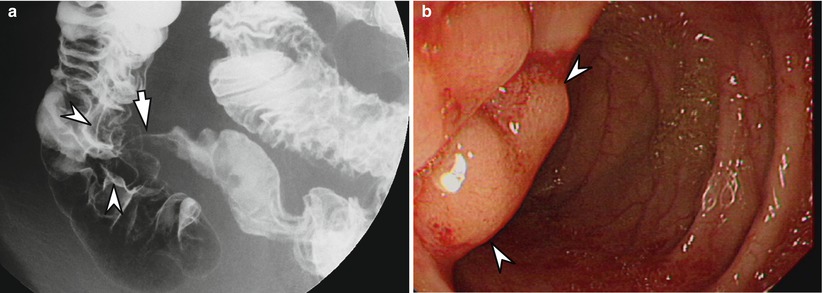
Fig. 11.8
Crohn’s disease involving the ileocecal area which may mimic tuberculosis. (a) Nodular thickening of the mucosal folds in the ileocecal region (arrowheads). Note the longitudinal ulcer in the terminal ileum (arrow) which is a characteristic of Crohn’s disease. (b) Colonoscopic image shows mucosal nodularity at the ileocecal area (arrowheads) and sparing of cecum
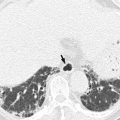
11.5.9 Crohn’s Disease: Active Inflammatory Disease – CT Findings
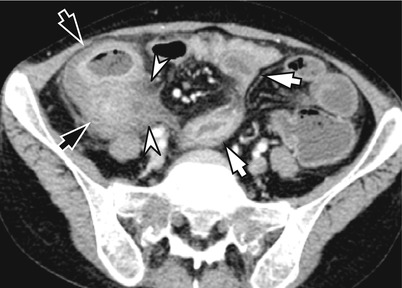
Fig. 11.9
Active inflammatory Crohn’s disease. Contrast-enhanced CT image shows mural stratification (“target sign”) in the small bowel (white arrows) and ileocecal region (black arrows). Note the mesenteric fat infiltration (arrowheads) around the affected bowel loops
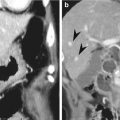
11.5.10 Crohn’s Disease: Active Inflammatory Disease – MR Findings
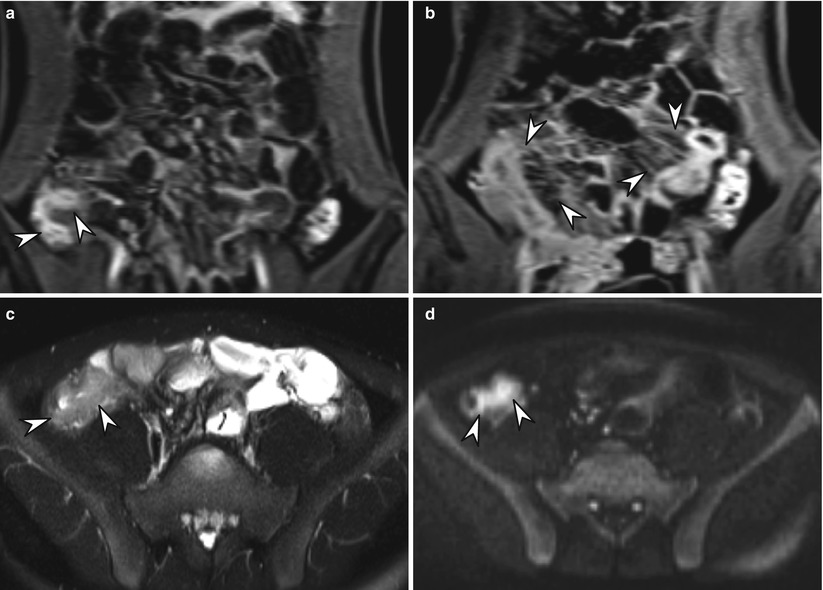
Fig. 11.10
Active inflammatory subtype of Crohn’s disease. (a) Coronal T1-weighted image after intravenous contrast enhancement shows marked mucosal enhancement (arrowheads) in the terminal ileum and cecum. (b) Note the increased vascularity in the small bowel mesentery (“comb sign”) (arrowheads). (c) Axial T2-weighted HASTE image shows mural thickening with high signal intensity (arrowheads) produced by submucosal edema. (d) On diffusion-weighted image (b = 800), actively inflamed bowel segments are seen as high signal intensities (arrowheads)
11.5.11 Crohn’s Disease: Fibrostenotic Disease – Enteroclysis Findings
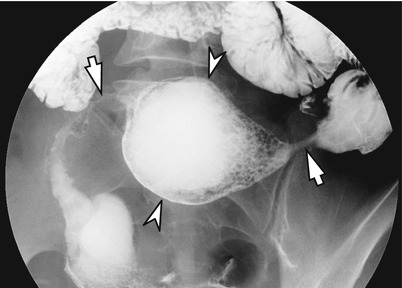
Fig. 11.11




Crohn’s disease: fibrostenotic disease. Enteroclysis of a 32-year-old patient with known Crohn’s disease demonstrates narrowed segments with aneurysmal dilation of distal ileum (arrowheads) between two stenotic segments (arrows)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree