16 Intra-abdominal Lymph Nodes The prognosis and treatment of a patient with malignant disease depend on the tumor stage, which is determined by the size of the primary tumor, the presence of metastases, and possible metastatic lymph node involvement. Tumor staging is especially relevant for predicting whether curative treatment, which usually means radical surgical resection, will be possible or whether palliative measures should be initiated. Despite its exquisite soft-tissue contrast, MRI unfortunately cannot differentiate between benign and malignant lymph node enlargement because normal and malignant lymph nodes have similar T1 and T2 relaxation times and proton densities.1 Nodal size therefore remains the sole MRI criterion for identifying metastatic involvement, and it is generally accepted that lymph nodes with a short-axis diameter ≥ 10 mm are likely to be malignant. Metastases in normal-sized lymph nodes escape detection with current MRI technology. Reported MRI sensitivities for detecting lymph node metastasis with currently available techniques and without specific contrast agents depend on the patient population investigated and the size threshold used and range from 0–89% with specificities of 44–100 %.2–10 Despite these limitations, which also hamper the other cross-sectional imaging modalities, MRI has some advantages over CT. These derive not from the higher soft-tissue contrast or multiplanar capability of MRI but from the fact that it is superior in defining local tumor stage, especially in patients with malignant neoplasms of the true pelvis. It has been shown that nodal metastatic spread is unlikely in tumors confined to the organ of origin but should be expected once a tumor has spread beyond that organ. A radiologist interpreting the MRI appearance of lymph nodes must therefore always take into account the local tumor stage (see Chapters 10–13). Ultra-small superparamagnetic iron oxide (USPIO) nanoparticles for intravenous injection hold promise for improving noninvasive lymph node evaluation in the future.11,12 These particles have completed clinical trials and are expected to be approved for clinical use. Abdominal lymph node evaluation alone is not an absolute indication for MRI. Apart from lymph node size, which can also be estimated by CT, there are no proven MRI criteria for identifying metastatic abdominal lymph nodes. Suspiciously enlarged lymph nodes are accurately depicted with CT, which is the primary staging modality for most abdominal tumors, assessment of abdominal lymph nodes in patients with extra-abdominal primary tumors (e. g., malignant melanoma, breast cancer), and systemic disease (e. g., Hodgkin disease). The following presentation therefore refers to those lymph node stations that are depicted on MR images acquired for the local staging of primary tumors in the true pelvis or abdomen (Table 16.1). These are specifically tumors for which local staging by MRI is superior to CT, i. e., tumors of the female reproductive system and some urologic tumors (prostate, urinary bladder) (see Chapters 10–13). In testicular cancer, no local staging is done and the retroperitoneal lymph nodes, the first site of nodal metastasis, are assessed in the setting of an abdominal CT scan. In patients with upper abdominal malignancy, the retroperitoneal lymph nodes have to be evaluated for metastasis from tumors of the kidneys and upper urinary tract (renal cell carcinoma, transitional cell carcinoma of the renal pelvis or ureter), adrenal glands, pancreas, and stomach. Lymph nodes in the hepatoduodenal ligament and celiac region may be involved in patients with tumors of the liver and bile ducts, stomach, or pancreas. Ovarian tumors tend to metastasize to omental and mesenteric lymph nodes. All of these lymph node regions must be evaluated for lymphadenopathy in patients with malignant melanoma or lymphoma. A dedicated MRI examination for lymphadenopathy is not indicated in patients with Hodgkin or non-Hodgkin lymphoma. In these patients, the lymph nodes are only evaluated if MRI is performed to identify possible organ involvement. Imaging is indicated for follow-up and monitoring of treatment outcome after surgery and/or radiotherapy or chemotherapy. In this setting, MRI is the preferred imaging modality, especially for gynecologic tumors. The images are evaluated for possible tumor recurrence after surgery or the response to radiotherapy or chemotherapy. Again, the radiologist should also note any enlarged lymph nodes. The spectrum of indications for nodal MRI is changing. State-of-the-art MRI scanners that support whole-body imaging (automatic table feed, multichannel phasedarray coil systems, parallel imaging techniques) have expanded the role of MRI in tumor evaluation and lymph node staging.13 With these new techniques, it is possible to image the area of the primary tumor, e. g., the pelvis in cervical cancer, as well as the entire abdomen to search for lymphadenopathy, especially in the retroperitoneum, with a minimum of extra time. Finally, the use of USPIO as a lymphotropic contrast agent for intravenous injection might improve the accuracy of nodal MRI in the future. One such substance has undergone extensive clinical trials and approval for clinical application is expected (see below). Within the abdomen, different imaging strategies are required for assessing lymph nodes in the upper and midabdomen as opposed to those in the pelvis. Administration of an antispasmodic agent (e. g., butylscopolamine or glucagon) is important to minimize peristaltic artifacts. A body or torso phased-array coil is recommended for assessment of both abdominal and pelvic lymph nodes.5 Axial images allow good evaluation of abdominal and pelvic lymph nodes. These may be supplemented by coronal images for evaluation of retroperitoneal nodes or oblique coronal images for the nodes along the external iliac vessels; the second plane serves to define the relationship to the major vessels and to estimate the ratio of short-to-long axis diameter. The coronal plane also enables very good visualization of mesenteric and omental lymph nodes. The peripancreatic or perigastric lymph nodes can be evaluated on sagittal images obtained in patients undergoing dedicated MRI of these organs. Alternatively, secondary reconstructions in any plane can be generated from a 3D dataset. Very rarely, a double oblique imaging plane may be needed to improve delineation of a suspicious lymph node (Table 16.1). Table 16.2 lists the pulse sequences that enable good evaluation of lymph nodes in different regions. Since it is usually not necessary to obtain both T1w and T2w images for detecting enlarged lymph nodes, the weighting that affords the best anatomic detail resolution should be chosen. For a high SNR, breath-hold imaging should be performed without fat suppression; however, free-breathing T2w sequences with multiple signal averages should be acquired with fat suppression (spectral saturation or inversion prepulse) to reveal lymph nodes as very-high-signal-intensity structures. Upper abdomen: Axial T1w or T2w sequences of the kidneys, adrenal glands, pancreas, liver, and stomach usually allow good identification of enlarged lymph nodes, especially when performed during breath-holding (T1w GRE, T2w single-shot TSE). Alternatively, the upper and mid-abdomen can be depicted with excellent quality using respiratory-triggered T2w sequences (e. g., respiratory bellows, respiratory cushion, or navigator echo technique) after administration of a spasmolytic agent. Additional coronal or sagittal images should also be acquired with a breath-hold sequence to shorten scan time and eliminate motion artifacts, which may particularly degrade coronal images (e. g., T1w GRE, T2w single-shot TSE). Pelvis: Pelvic MRI should include a high-resolution sequence with T1 to proton density (PD) weighting acquired after administration of a spasmolytic agent and covering the region from the aortic bifurcation to the pelvic floor. This sequence offers excellent depiction of pelvic lymph nodes. If available, the sequence should be performed as a fast or turbo spin-echo sequence (FSE or TSE) with a short effective TE (Table 16.2). Both oral and intravenous contrast media can improve delineation of abdominal and pelvic lymph nodes. One lymph-node-specific agent has completed the clinical trial phase and holds promise for improving lymph node MRI in the future (see p. 336 ff). Oral Contrast Media The use of oral contrast medium depends on the recommendations for MRI of the primary tumor under investigation or on the region imaged and the pulse sequences used if oral contrast is given specifically to improve lymph node conspicuity. For details on timing of oral contrast administration, see Chapter 5. No oral contrast medium is needed for evaluating abdominal lymph nodes if the system hardware (1.0–1.5 T) supports fast breath-hold imaging (e. g., T1w GRE, T2w single-shot TSE), which minimizes respiratory and peristaltic artifacts. In the true pelvis, respiratory artifacts are less of a problem and the FSE or TSE sequences typically used to image this region provide excellent image quality when an antispasmodic agent has been given to reduce peristalsis. Although scanning takes a few minutes, good delineation of pelvic lymph nodes is usually achieved, except in very slender or cachectic patients, in whom the lack of intra-abdominal fat may preclude differentiation of lymph nodes from bowel loops. In these cases oral contrast administration is indicated for abdominal and pelvic scans, even with state-of-the-art MRI techniques. Image quality may be poorer on less sophisticated MR scanners with longer scan times for a complete abdominal examination because multiple signal averaging sequences are necessary. Thus, oral contrast administration is indicated for imaging of both the abdomen and the pelvis. Nonspecific Intravenous Contrast Media
M. Taupitz and D. Beyersdorff
Introduction
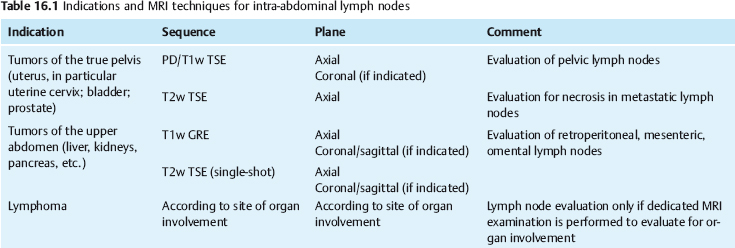
Indications
Imaging Technique
Imaging Planes
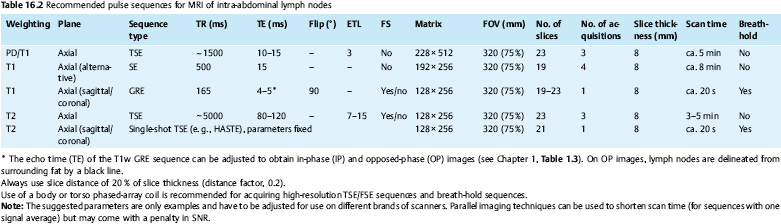
Pulse Sequences
Contrast Media
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree