Abrupt interruption of the internal carotid artery without a balloon test occlusion (BTO) carries a 26% risk of cerebral infarction. BTO is a test used to decrease this risk by evaluating the efficacy of the collateral circulation. Clinical tolerance of parent vessel occlusion can be assessed by a BTO with several variables, including the clinical examination, angiographic assessment, stump pressure, induced hypotension, perfusion scanning, transcranial Doppler ultrasonography, and neurophysiologic monitoring. This review discusses the indications, methods, predictive value, and complications of BTO.
Key points
- •
Parent vessel occlusion (PVO) may be required in wide-neck giant aneurysms, pseudoaneurysms, traumatic vascular injuries, carotid blowout, and carotid fistulas.
- •
Clinical tolerance of PVO can be assessed by a balloon test occlusion (BTO) with several variables, including the clinical examination, angiographic assessment, stump pressure, induced hypotension, perfusion scanning, transcranial Doppler ultrasonography, and neurophysiologic monitoring.
- •
A good rule of thumb is to place the balloon at or near the level of the proposed occlusion.
- •
Two of the most useful variables during a BTO to determine whether a patient will tolerate a PVO are the clinical examination and venous phase assessment on the angiogram.
- •
Primary collaterals are those related to the circle of Willis (anterior communicating artery and posterior communicating artery), whereas secondary collaterals consist of retrograde flow within the ophthalmic artery, external carotid artery branches, and leptomeningeal collaterals.
Introduction
The evolution of endovascular technology has allowed for the treatment of complex vascular pathologies. Advances in stent and coil technology are at the heart of this treatment; however, parent vessel occlusion (PVO) remains a viable option in treating certain vascular diseases. Endovascular PVO with detachable balloons dates back to the early 1970s and was first reported by Serbinenko.
Wide-neck giant aneurysms, pseudoaneurysms, traumatic vascular injuries, carotid blowout, and carotid fistulas are examples of conditions that may require PVO. A patient harboring a head and neck cancer may also require PVO as preoperative preparation before tumor resection. Carotid artery occlusion is a simple procedure, but avoiding immediate or delayed hemodynamic cerebral ischemia remains a challenge.
The main complications associated with PVO are thromboembolic or related to immediate or delayed hemodynamic ischemia. Linskey and colleagues reported 254 patients who underwent PVO without a balloon test occlusion (BTO). The ischemic complication rates were high, with 26% of patients suffering a cerebral infarct and 12% of the patients experiencing mortality related to the infarct. Thromboembolic complications are treated with anticoagulation; however, immediate or delayed hemodynamic ischemia is best treated by determination of which patients will develop this state before PVO. BTO is one method by which an interventionalist can evaluate whether a patient is able to tolerate a PVO. Those patients who fail the BTO require a revascularization procedure before PVO. This review discusses the indications, methods, predictive value, and complications of BTO.
Introduction
The evolution of endovascular technology has allowed for the treatment of complex vascular pathologies. Advances in stent and coil technology are at the heart of this treatment; however, parent vessel occlusion (PVO) remains a viable option in treating certain vascular diseases. Endovascular PVO with detachable balloons dates back to the early 1970s and was first reported by Serbinenko.
Wide-neck giant aneurysms, pseudoaneurysms, traumatic vascular injuries, carotid blowout, and carotid fistulas are examples of conditions that may require PVO. A patient harboring a head and neck cancer may also require PVO as preoperative preparation before tumor resection. Carotid artery occlusion is a simple procedure, but avoiding immediate or delayed hemodynamic cerebral ischemia remains a challenge.
The main complications associated with PVO are thromboembolic or related to immediate or delayed hemodynamic ischemia. Linskey and colleagues reported 254 patients who underwent PVO without a balloon test occlusion (BTO). The ischemic complication rates were high, with 26% of patients suffering a cerebral infarct and 12% of the patients experiencing mortality related to the infarct. Thromboembolic complications are treated with anticoagulation; however, immediate or delayed hemodynamic ischemia is best treated by determination of which patients will develop this state before PVO. BTO is one method by which an interventionalist can evaluate whether a patient is able to tolerate a PVO. Those patients who fail the BTO require a revascularization procedure before PVO. This review discusses the indications, methods, predictive value, and complications of BTO.
Technique for BTO
Several techniques have been described for performing a BTO. The underlying principle is to evaluate the efficacy of the intracranial collateral circulation in maintaining perfusion of the affected vascular territory during temporary occlusion of the main arterial supply. Clinical tolerance of PVO can be assessed by a BTO with several variables including: the clinical examination, angiographic assessment, stump pressure, induced hypotension, perfusion scanning, transcranial Doppler (TCD) ultrasonography, and neurophysiologic monitoring. Most centers use several of these variables in assessing the clinical safety of PVO.
Standard technique
Informed consent is obtained from the patient. In cases in which clinical examination is to be assessed, the patient is awake and the procedure is performed under local anesthetic. Benzodiazepines should not be used because they can interfere with memory functions and related tasks. The patient is told that they will be asked questions evaluating their memory, speech, motor, sensory, and analytical skills (calculations) while the procedure is being performed.
A 6-French femoral sheath is introduced into the femoral artery using a single wall puncture technique. Although either femoral artery can be used for access, we prefer to puncture the femoral artery opposite to the side of disease. This precaution ensures that any complication associated with the BTO, PVO, or femoral sheath placement affects only 1 extremity. A baseline activated clotting time (ACT) is drawn, and the patient is given 70 to 100 units per kilogram (U/kg) of heparin. An ACT is drawn 10 minutes after administration of heparin and then every 15 minutes as needed. The goal ACT is approximately 2.5 times the patients’ baseline to prevent procedure-related thromboembolic complications.
A 4-French diagnostic catheter is used to perform a 4-vessel cervical and cerebral angiogram in the anteroposterior and lateral projections. Next, a 6-French guide catheter is introduced into the common carotid artery (CCA). A nondetachable balloon catheter is then introduced and positioned in the distal cervical segment of the internal carotid artery (ICA). A good rule of thumb is to place the balloon at or near the level of the proposed occlusion. Low position of the balloon can cause a carotid sinus reflex, leading to significant bradycardia. This is the main reason BTO is not performed from the CCA, because this leads to a decreased pressure within the carotid sinus, which reflexively causes an increase in arterial blood pressure (ABP). Such a reflex can give a confounding clinical result because the ABP could be lower in a normal state. Although we have not experienced significant alteration in ABP or heart rate during a BTO, we are always prepared with temporary pacer wires as well as atropine in case the situation were to arise.
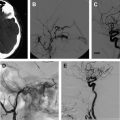
The balloon is inflated with angiographic confirmation of complete occlusion of the vessel in question. The balloon is inflated for a total duration of 30 minutes and a neurologic examination is performed by the operator every 5 minutes ( Fig. 1 ). If there are any changes in the patient’s neurologic examination, then the balloon is immediately deflated and cerebral angiography is performed. If the patient is under general anesthesia for the procedure, 12-lead electroencephalogram (EEG) monitoring maybe helpful. Some investigators puncture the contralateral femoral artery and perform a cerebral angiogram of the contralateral ICA and 1 vertebral artery to evaluate the collateral circulation with the balloon inflated.
The technique for vertebral artery occlusion is similar to that described for the ICA. For tumor disease and posttraumatic lesions of the vertebral artery, BTO is performed proximal to the level of the lesion. For vertebral arteriovenous fistulae, BTO is performed over the site of the fistula or just proximal to it ( Fig. 2 ). In the case of an aneurysm, the level of occlusion depends on the location of the aneurysm and whether the therapeutic goal is to reduce flow in the aneurysm or occlude the parent vessel.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree