Fig. 29.1
Degenerative changes in the lumbar intervertebral discs. Human lumbar spine fixed in 10 % neutral buffered formalin for 1 week is shown. Individual lumbar segments were prepared, taking care to preserve the posterior elements. (a) Mostly intact annulus with minor lamellar disorganization in a minimally degenerated disc with the absence of fissuring. (b) Lamellar disorganization in a degenerated lumbar disc with presence of radiating tear extending to the outer 1/3 of the annulus. There may be some loss of the nucleus on this gross dissection of the human spine (With permission from Baylis Medical Company © Copyright)
Temperatures reached during biacuplasty or IDET may be sufficient to cause nerve destruction which occurs at 42–45 °C or higher [25–27]. However, evidence from the basic science studies to demonstrate neuroablation by delivered heat as the mechanisms of action for discogenic pain relief remains unavailable until this date.
The temperature profiles of the latest intradiscal heating procedure and one with most promising clinical data, intradiscal biacuplasty, were investigated in both porcine and human cadaveric lumbar discs. Histological examination could not detect signs of tissue degradation due to heating or changes in the collagen structure in both degenerated and nondegenerated intervertebral discs [28, 29].
Intradiscal Electrothermal Therapy (IDET)
The first effective minimally invasive therapeutic alternative to fusion surgery or arthroplasty came in the form of intradiscal electrothermal therapy (IDET) [30, 31]. IDET is performed using a thermal catheter, resistive coil (SpineCATH, Smith & Nephew Endoscopy, Andover, MA), that is percutaneously introduced to the interface between the posterior annulus and nucleus under multiplanar fluoroscopic control (Figs. 29.2a–d and 29.3a, b).
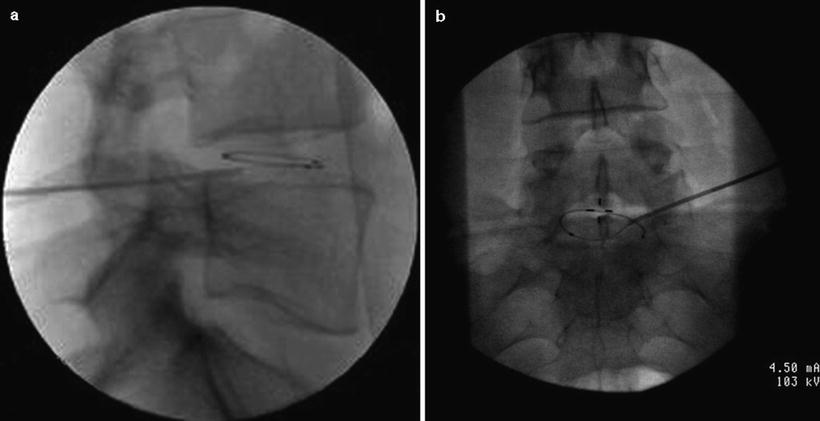
Fig. 29.2
Diagram of the heat-delivering electrodes within the intervertebral disc and approximate temperature that can be produced during four different minimally invasive procedures aimed to treat discogenic pain. (a) Intranuclear radio frequency. The RF electrode is positioned in the middle of the nucleus. Temperature achieved may not be sufficient to denervate posterior annulus when the heat source is inside the nucleus. (b) Intradiscal electrothermal therapy (IDET). Resistive coil is placed between the annulus and nucleus and along the posterior annulus. Optimal temperature dissipates several millimeters and may affect a very limited area of the annulus. (c) DiscTRODE™ (radio-frequency electrode) is positioned within the posterior annulus. (d) Intradiscal biacuplasty. Radio-frequency electrodes are positioned inside the posterior annulus to achieve optimal bipolar heating and possible nociceptor denervation (With permission from Baylis Medical Company © Copyright)
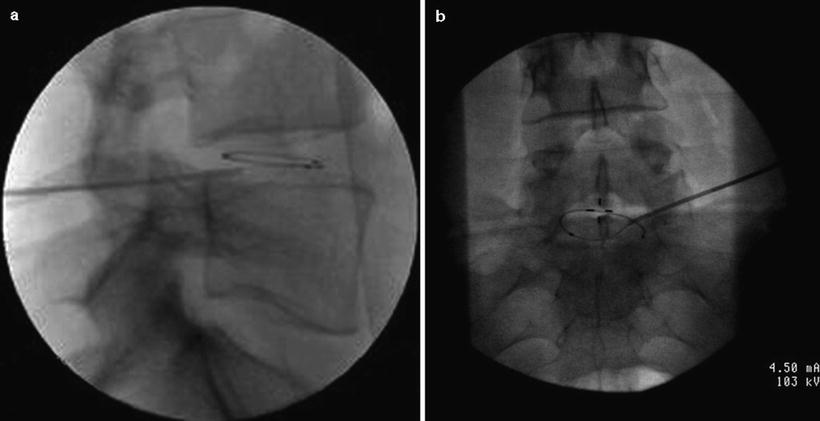
Fig. 29.3
The fluoroscopic views of the final electrode position during IDET procedure used for the treatment of discogenic pain. IDET resistive coil properly positioned just between annulus and nucleus of the lumbar intervertebral disc. (a) Lateral view of the final coil position within L4–5 lumbar disc. (b) Anterior view of the IDET coil when cranial tilt of the fluoroscope is used to clearly show a full circle of the coil placed inside the disc at the interphase between the annulus and nucleus (With permission from Baylis Medical Company © Copyright)
There are dozens of prospective case series and reports and a single, randomized, controlled trial that provided data on the IDET efficacy ([30–41]; Table 29.1). However, one, randomized, controlled trial and several published case series failed to demonstrate any clinical benefit of the IDET procedure [37, 41]. The first randomized, sham-controlled trial provided class I evidence that IDET is an efficacious annuloplasty procedure in properly selected patients [36]. It seems that IDET could provide rather long-term pain relief as evidenced at 1-year and 2-year follow-ups ([30–41]; Table 29.1). When used in general population of the patient with lower back pain, it seems that those with overlapping inflammatory arthritides or nonspinal conditions that may mimic lumbar discogenic pain and those patients with multilevel degenerative disc disease do not benefit from the IDET annuloplasty [39, 42, 43]. It seems that the variation in patient selection and provided heating techniques are thought to account for most of the differences seen in clinical results [30, 31, 36, 37, 39, 41–50]. Pauza and colleagues’ use of provocation discography, rather than MRI/discography combined criteria for the patients enrollment, may have contributed to high number of patients needed to treat – five to achieve >75 % improvement in one patient [36]. Overweight patients [42] and patients receiving workers’ compensation benefits [43, 50] represent additional patient subsets that are unlikely to benefit from the IDET.
Table 29.1
Pertinent studies on various types of annuloplasties when used for the treatment of discogenic lower back pain
Author name | Year | Type of intervention | Indications of procedure | Patients (#) | Type of study | Outcomes | Complications | Conclusions |
|---|---|---|---|---|---|---|---|---|
Assietti et al. [32] | 2010 | IDET | Single-level DDD and discogenic pain, >60 % disc height | 50 | Prospective | VAS 68 % decrease, ODI from 59.0 ± 7.6 % to 20.1 ± 11 % at 24 m | None | Safe and effective |
2008 | Biacuplasty | Single- or two-level DDD and discogenic pain, >50 % disc height | 15 | Prospective pilot | 7 of 13 >50 % VAS, ODI to 17.5, and SF-36-PF from 51 to 67 at 12 m | None | Safe and effective | |
Kvarstein et al. [35] | 2009 | DiscTRODE™ | Chronic LBP, discogenic pain | 23 | Prospective randomized, double-blind | No improvement study or sham at 12 m | None | Do not recommend use of discTRODE |
Pauza et al. [36] | 2004 | IDET | DDD and discogenic pain, >80 % disc height | 64 | Randomized sham-controlled prospective | 56 % >2 VAS change, 50 % patients >50 % relief at 6 m | None | Safe and effective |
Freeman et al. [37] | 2005 | IDET | Multilevel DDD, workers’ comp included | Randomized sham-control prospective | Oswestry unchanged | None | Ineffective | |
Jawahar et al. [38] | 2008 | IDET | DDD and discogenic pain, >80 % disc height, WC patients | 53 | Prospective | VAS reduction 63 %, ODI 70 % | None | Useful in carefully selecting WC patients |
Kapural et al. [39] | 2004 | IDET | Single- or two-level DDD and discogenic pain, >50 % disc height vs. multilevel DDD | 34 | Prospective matched study | 1,2-DDD >50 % improvement in VAS and PDI | None | IDET procedure effective only in one- or two-level DDD |
Karaman et al. [40] | 2011 | Biacuplasty | Single- or two-level DDD and discogenic pain., >50 % disc height | 15 | Prospective observational | 78.6 % >10 points Oswestry; >2 points VAS | None | Safe and effective |
Technique
The IDET procedure is performed under local anesthesia and mild intravenous sedation in sterile conditions. IV antibiotics, most frequently 1 g of cefazolin or 1 g of vancomycin, should be given 30–60 min before the procedure. Patients are positioned prone using midabdomen support to correct for the lumbar lordosis. Using local anesthesia, a 17-gauge needle is inserted under fluoroscopic guidance into the targeted disc. Through that same needle, a catheter with thermal resistive coil is navigated until positioned appropriately within the disc. The key is to position such catheter across all of the semicircumference delineated by the interphase of the posterior annulus and nucleus (Fig. 29.3a, b). The thermal resistive coil generates gradual rising temperature inside the disc up to 90 °C in 0.5 °C increments. The temperature is then maintained at 90 °C for 4 min according to manufacturer protocol (Smith & Nephew, London, UK). Patient is then brought to the recovery area and discharged home with instructions regarding functional rehabilitation program. The goals of such rehabilitation after the annuloplasty are pain control and reduction of inflammation, providing early supervised stretching and mobilization of tissue. In order to achieve functional restoration, addressed are extensor muscles, which may be deconditioned, as well as abdominals, trunk rotator, and trunk/hip flexors. During that time interval of 4–6 weeks, manual manipulative therapy is avoided.
Intradiscal Biacuplasty
Intradiscal biacuplasty employs bipolar RF electrodes to heat posterior annulus of the intervertebral disc. Although recently described, it could be the most promising of all annuloplasty methods [33, 34, 51]. This method works specifically by concentrating RF current between the active electrodes placed on the tip of two straight probes (Fig. 29.4a, b). The larger area of the posterior annulus is ablated by internally cooling the electrodes [29, 52] (Figs. 29.2a, b and 29.4a, b). Two intradiscal electrodes are first placed bilaterally in the posterior annulus of the intervertebral disc, and then generator temperature is increased gradually over a period of 10 min to 50 °C with final heating for another 5 min. Additional two monopolar lesions over 2.5 min are then produced bilaterally at 60 °C in order to extend lesion laterally and to achieve appropriate temperature increase to extended area of posterior annulus. During this time, the patient should be awake and communicating to the physician.
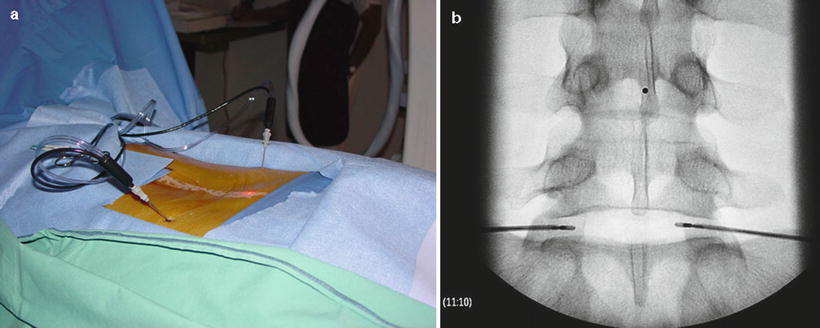
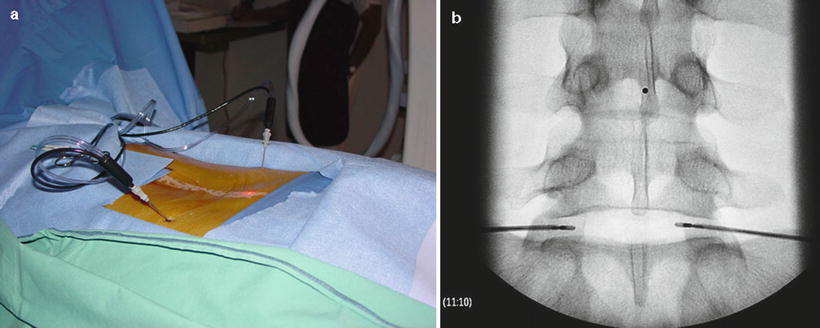
Fig. 29.4
Intradiscal biacuplasty electrodes properly positioned in bipolar fashion via introducers inside the patient’s back (a) and shown in anterior-posterior view inside L5–S1 lumbar intervertebral disc (b). Note that the electrodes are positioned in the middle of the disc and away from the end plates and bony structures (With permission from Baylis Medical Company © Copyright)
The first case report on biacuplasty documented significant improvements in functional capacity and VAS pain score at 6 months following the procedure with no perioperative complications. Later, three prospective case series involving 8, 15, and 15 patients, respectively, were completed, during which significant pain relief and improvement in the function were achieved at 3, 6, and 12 months after biacuplasty [33, 34, 40, 53]. In the European case series [53] involving eight patients, there was an average of 50 % pain reduction at 3 months with an overall good patient satisfaction. No patients reported any post-procedural pain, often associated with other therapies, and there were no reported complications. During the prospective pilot study involving 15 patients, reported were improvements in several functional capacity measures after the procedure with no complications [33, 34]. Improvements in Oswestry index were sustained from 23.3 at baseline to 16.5 points at 1 month and stayed same at 12 months. The prospective, randomized sham study is being currently completed in order to accept or refute results achieved during pilot study.
The latest prospective, observational study showed that 78.6 % of the patients had Oswestry score improvement of 10 points or more with 57 % of the patients having 50 % or more pain relief at 6 months after the procedure [40]. Authors concluded that their data are in agreement with other two studies data published earlier [33, 40, 53].
Intradiscal biacuplasty seems to provide several improvements over the IDET. There is minimal disruption to the native tissue architecture, and thus the biomechanics of the spine is less affected. The relative ease of electrode placement eliminates the need to thread a long resistive coil like in IDET procedure. Lower peak heating temperatures within the disc annulus compared to IDET do allow better patient tolerance. In addition, internal cooling of the probes limits excessively high temperatures in the disc that may cause tissue adherence [29, 52].
Technique
The procedure is completed under fluoroscopy with the patient lying in the prone position. Light sedation and analgesia can be provided for relaxation and pain control before and during the procedure, but the patient should be able to communicate with physician throughout the procedure. Two 17-G TransDiscal introducers are introduced to annulus bilaterally (Fig. 29.4a, b




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree