Key Points
- ▪
IVUS can be used to characterize, with high resolution, coronary artery architecture and coronary artery plaque, and other lesional architecture.
- ▪
IVUS can be used to guide coronary stent deployment by assessing the adequacy of the stent apposition to the vessel well.
Introduction
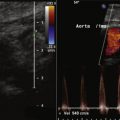
Intravascular ultrasound (IVUS) is a device used to visualize the vessel wall in a two-dimensional tomographic format. The ultrasound signal penetrates below the luminal surface, imaging the entire cross section of the vessel in real time. The current IVUS system for coronary artery imaging uses a miniaturized transducer with high-frequency ultrasound (20 to 45 MHz), achieving a resolution of 150 microns. IVUS is the first imaging modality that directly visualizes atherosclerosis and other pathologic conditions from within the vessel wall. Today, IVUS is often used in the catheterization laboratory at the time of percutaneous coronary intervention (PCI) for pre-PCI lesion assessment and post-PCI evaluation of the results.
Basic Image Interpretation
The coronary arterial wall consists of three concentric layers. The layer adjacent to the arterial lumen is called the intima and is made up of a superficial lining of endothelial cells immediately exposed to the blood. The media is composed of many layers of smooth muscle cells interspersed with connective fibers embedded in a glycoprotein matrix. The external elastic lamina separates the medial layer from the adventitia. The adventitia is fibrous in nature and has the highest density of collagen. It offers the architectural support to the vessel. IVUS images of coronary arteries generally demonstrate the three major layers of the arterial wall: intima, media, and adventitia ( Fig. 12-1 ).

Practical Intravascular Ultrasound Use in the Catheterization Laboratory
Typical IVUS indications in the catheterization laboratory include pre-PCI assessment of the lesions and evaluation of post-PCI results ( Table 12-1 ). In particular, arterial stenting has become one of the most important applications for IVUS in clinical settings. On IVUS examination, stent struts are easily visualized as a collection of bright, distinct echoes. IVUS imaging can show the apposition of the stent to the vessel wall, which is essential for achieving optimal PCI results. In bare metal stents, IVUS guidance has been shown to improve stent deployment with dramatic reduction of the risk of stent thrombosis, which ultimately leads to the diminishing need for aggressive anticoagulation in most cases.
| Pre-PCI Assessment | |
| Quantitative assessment |
|
| Qualitative assessment |
|
| Post-PCI Assessment | |
| Quantitative assessment | Minimal lumen area (minimal stent area) |
| Qualitative assessment |
|
Preinterventional Assessment
Preinterventional IVUS has been used to assess the severity and morphology of coronary artery stenosis as well as to measure reference vessel size and lesion length, especially when angiography yields equivocal or difficult-to-interpret images. Based on physiologic approaches, including fractional flow reserve, coronary flow reserve, and stress scintigraphy, the ischemic minimal lumen area threshold has been reported to be 3 to 4 mm 2 for major epicardial coronary arteries and 5.9 mm 2 for the left main coronary artery (LMCA). The presence, location, and extent of calcium can significantly affect the results of angioplasty, atherectomy, and stent deployment. Precise measurement of lesion length, vessel size, and plaque burden can also help optimize the PCI results.
Assessment of Angiographically Equivocal Lesions
Ostial Lesion
The severity of ostial lesions, especially LMCA lesions, is sometimes difficult to assess using conventional angiography alone. IVUS may help provide more accurate assessment of the severity of this lesion subset. Because of the recent increase in use of PCI with the LCMA, assessment of this artery has become an important indication for IVUS imaging. The cutoff value of significant LMCA stenosis is 5.9 mm 2 based on a previous physiologic study. Deep engagement of the catheter to the LCMA prohibits the assessment of LMCA ostium, and the operator sometimes has to purposefully disengage the catheter from the orifice of the artery ( Figs. 12-2 and 12-3 ).