- Request the correct investigation
- Use a systematic approach to interpretation—ABCs
- Fundamental principles to avoid errors—Rules of two
- Always ASK for help—if in doubt!
Emergency medicine often brings together critically ill patients and inexperienced and tired doctors—a dangerous combination at the best of times with potentially serious clinical and medicolegal consequences. Virtually any medical condition can present in the emergency department (ED) and so the volume of medical knowledge needed to manage these patients satisfactorily is enormous.
There have been major technological advances in the past decade which have had a major impact on the management of patients in the ED, not least picture archiving and communication systems (PACS), digital radiography (replacing conventional plain to X rays), portable ultrasound (US; which is now readily available and often, but not often enough, performed by clinicians in the ED) and multidetector computed tomography (MDCT) in the ED. Despite all these advances, plain to X rays (whether conventional or digital) remain the mainstay of initial and successful management of most sick and traumatised patients in the ED.
- Plain to X rays (conventional or digital)
- Portable US
- MDCT
- MRI
The correct selection of imaging modality, rapid acquisition and the accurate interpretation of these investigations is often the key to quick and successful management of patients in the ED. Unfortunately these investigations are often done and interpreted by medical staff who have little, if any, training in radiology and the usual safety net of a specialist radiological service is not available at the time of presentation, when it is most needed. This leads to delays and invariably results in increased morbidity and mortality! The selection of the correct imaging modality on admission saves time and saving time, saves lives! Ideally there should be a seamless 24/7 service.
MDCT—initial imaging modality of choice in the ED
| Head injuries/headaches or epilepsy | Skull X-ray (SXR) no longer done. CT head ± contrast |
| Facial injuries | MDCT with multiplanar reconstructions (MPR) and 3D are essential |
| Chest pain (suspected aortic aneurysm (AA), myocardial infarction (MI), pulmonary embolus (PE) or pneumothorax (Px)) | Triple rule out CT scan |
| Severe abdominal pain (obstruction) | CT has replaced abdominal X-ray (AXR) |
| Renal/ureteric colic | CT kidneys, ureters and bladder (KUB) has replaced Intravenous urogram (IVU) in ED |
| Suspected leaking abdominal aortic aneurysm (AAA) | CT has replaced US and AXR |
| Suspected gastrointestinal (GI) bleeding | Initially CT angiography instead of angiography |
| Major trauma (adults) | Whole body CT instead of chest X-ray (CXR), AXR and US |
Figure 1.1 (a) Anteroposterior shows minimal overlap of proximal interphalangeal joint (PIPJ) of little finger; (b) lateral shows obvious dislocation of PIPJ.

The Rules of Two (Ro2) is a helpful, simple set of guidelines, which relate to who, what, when and how to radiograph and how to get help or get out of trouble and therefore minimise the chances and the consequences of errors.
The ABCs systematic assessment is a simple systematic approach, which starts with basic essential normal radiographic anatomy, common normal variants, which may mimic pathology and in particular how to interpret imaging using a systematic approach, which is logical and easy to remember and therefore hopefully helps to minimise interpretive errors.
Rules of Two
These rules represent a simple set of guidelines, most are obvious, some relate to specific clinical problems, but most are common sense useful general principles which should help in avoiding errors in interpretation and management of patients in the ED.
Figure 1.2 (a) Anteroposterior shows no obvious abnormality; (b) lateral shows oblique fracture of fibula.

- Two views—one view is always one view too few
- Two abnormalities—if you see one abnormality, always look for a second
- Two joints—image the joint above
- Two sides—if not sure or difficult X ray, compare with other side
- Two views too many—CT (and rarely US) has replaced plain X rays in many clinical situations
- Two occasions—always compare with old films IF available
- Two visits—bring patient back for repeat examination
- Two opinions and two records—always ask a colleague if not sure and record findings
- Two specialists—always get your ED specialist and also a radiologist’s opinion
- Two investigations—always consider whether US, CT or MRI would help in diagnosis
Rule 1—two views (‘One view is always one view too few’)
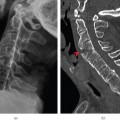
Two views should be taken, preferably perpendicular to each other (Figure 1.1). This applies to all radiographs except the chest, abdomen and pelvis. It is not uncommon for a fracture or an abnormality to be visible only on one view (Figure 1.2).
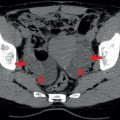
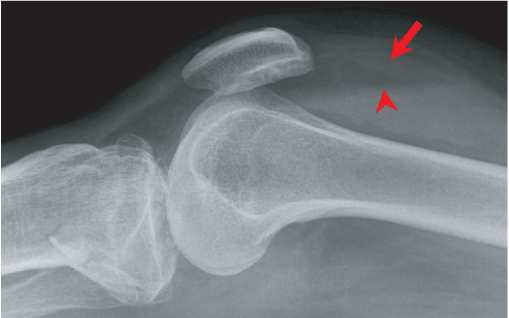
In addition, if the two views fail to show an injury when there is a radiological suspicion of an injury (such as the presence of a fat pad sign (Figure 1.3) in the elbow or a lipohaemoarthrosis (Figure 1.4) of the knee or if the findings don’t fit in with the clinical presentation, then further views are warranted.
Figure 1.3 Lateral elbow: anterior (arrow) and posterior fat pads (arrowhead). Anteroposterior view was normal so additional views of radial head were requested.
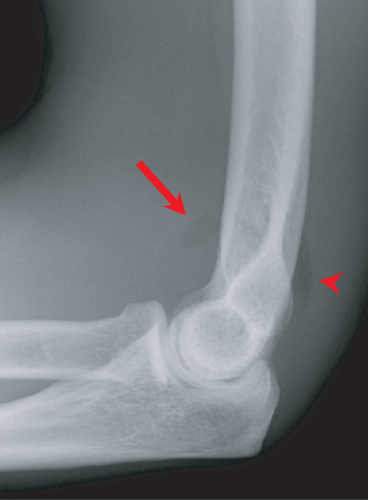
Figure 1.4 Lateral horizontal beam: lipohaemoarthrosis fat above (arrow); blood below (arrowhead).
Rule 2—two abnormalities
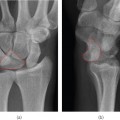
Do not stop looking after detecting one abnormality; always keep looking for a second abnormality. There may be more than one fracture (Figure 1.5) or there may be an underlying predisposing abnormality, such as metastases (Figure 1.6). In addition, if there is a fracture in a ring-like structure such as the pelvis (Figure 1.7), mandible (Figure 1.8), radius/ulna or tibia/fibula, there will usually be a second fracture (a polo mint will always break in two places; see Figure 1.9).
Figure 1.5 Salter–Harris II of proximal tibia (large arrow for fracture of proximal tibial metaphysis, arrowhead for separation of epiphyseal growth plate) and fracture of shaft of proximal fibula (small arrow).
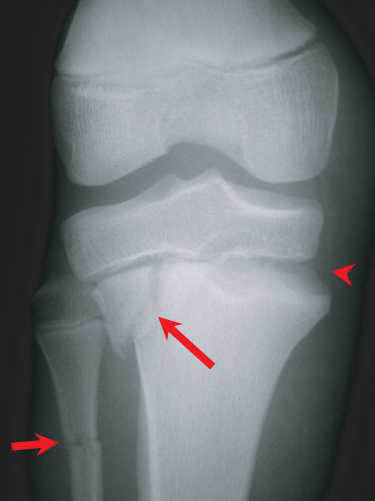
Figure 1.6 Fracture of proximal humerus (arrow) with subtle lytic metastases (arrowheads).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree