Case presentation
A 14-year-old male is brought to the emergency department with severe diffuse abdominal pain. He has had multiple episodes of nonbloody but bilious emesis accompanying the pain. There has been no fever, diarrhea, or trauma. There are no sick contacts or travel. He has had decreased oral intake of both solids and fluids due to nausea over the past 5 days. Notably, his weight is 30.7 kg and height is 177 cm (body mass index of 9.6 kg/m 2 ).
Physical examination reveals a miserable appearing afebrile child lying in a fetal position in obvious discomfort. His vital signs are a heart rate of 130 beats per minute, respiratory rate of 30 breaths per minute, and a blood pressure of 127/80 mm Hg. Noticeably, the child is quite thin and appears malnourished. He is difficult to examine but he indicates that he has diffuse abdominal pain that you are unable to localize and his abdomen appears to be distended.
As you consider imaging options, his mother tells you that the child has a history of “liver problems” and was “a preemie, but did not stay in the NICU for more than a few weeks.” She is unable to elaborate further on this bit of history.
Imaging considerations
Pediatric abdominal pain is one of the most common symptoms encountered in the emergency department. Most of these children have a benign or self-limited cause, such as a viral illness or constipation. A thorough history and physical examination will often assist the clinician in determining the etiology of abdominal pain, and not all children require imaging.
Abdominal imaging should be considered in any child in whom a potentially complex surgical condition is a concern (such as appendicitis with abscess) or in whom bowel obstruction is suspected or when a diagnosis is in question and imaging will help clarify a clinical situation. This child has thin body habitus and signs of bowel obstruction.
There are several options available to the clinician.
Plain radiography
A readily available imaging modality with minimal ionizing radiation exposure, plain radiography can be useful in the pediatric patient with acute abdominal pain. Sedation is not required. Assessment of the bowel gas pattern is easily accomplished and an abnormal pattern can suggest a bowel obstruction. The presence of free air can be noted, if present, suggesting bowel perforation. Bowel wall thickening may also be seen, suggesting edema, which may be secondary to an inflammatory process, such as enteritis or colitis. Radio-opaque foreign bodies that are at high risk for producing perforation or obstruction, such as sharp objects or magnets, may be a source of abdominal pain in pediatric patients and can be easily identified.
A two-view series of the abdomen (anterior-posterior [AP] supine and left lateral decubitus views in young children, typically less than 8 years old, or AP supine and upright views in older children) is preferable to assess the bowel gas pattern and to assess for the presence of free air, bowel obstruction, and radio-opaque foreign bodies. A horizontal beam radiograph (AP upright or left side down decubitus views) is necessary to evaluate for free intraperitoneal air. On an upright view, to adequately evaluate for free air, the diaphragms must be included. On a left lateral decubitus view, the right lateral abdomen must be fully included. If an upright or left lateral decubitus view cannot be obtained, a cross-table lateral view of the abdomen, with the patient supine, may be utilized. There may be situations where a two-view abdominal series is not possible and an AP view will have to suffice.
Computed tomography (CT)
CT of the abdomen is useful in the evaluation of abdominal pain in the pediatric population. CT imaging depicts a wide range of causes of abdominal pain, including inflammatory (colitis, enteritis), infectious (abscess, pyelonephritis), surgical (bowel obstruction, appendicitis, intussusception, hernia), renal calculi, and traumatic injuries. CT is generally readily available and rapid; pediatric patients rarely require sedation to obtain a quality study. Ionizing radiation is a concern, and ALARA (as low as reasonably achievable) principles should be applied when choosing to make use of CT imaging. For conditions well evaluated by sonography, such as intussusception or appendicitis, ultrasound (US) is preferred as the first-line imaging test. Oral contrast for CT scanning is generally not indicated in the acute setting. For suspected renal calculus disease, CT imaging is performed without intravenous (IV) contrast. For most other suspected causes of abdominal pain, IV contrast is indicated. If there is any question regarding the use of IV contrast, consultation with the radiologist is recommended. Placing an IV in the pediatric patient can be traumatic; if time allows, a topical anesthetic, such as topical lidocaine (4%), can help make IV placement smoother.
Ultrasound
This imaging modality is commonly used in pediatric patients with abdominal pain, particularly when appendicitis is suspected. US is also the first-line imaging test for suspected intussusception, biliary tract disease including cholecystitis, and gynecologic, testicular, and urinary tract pathologies. The availability, rapidity of the study, and lack of ionizing radiation exposure are attractive attributes of sonography.
Imaging findings
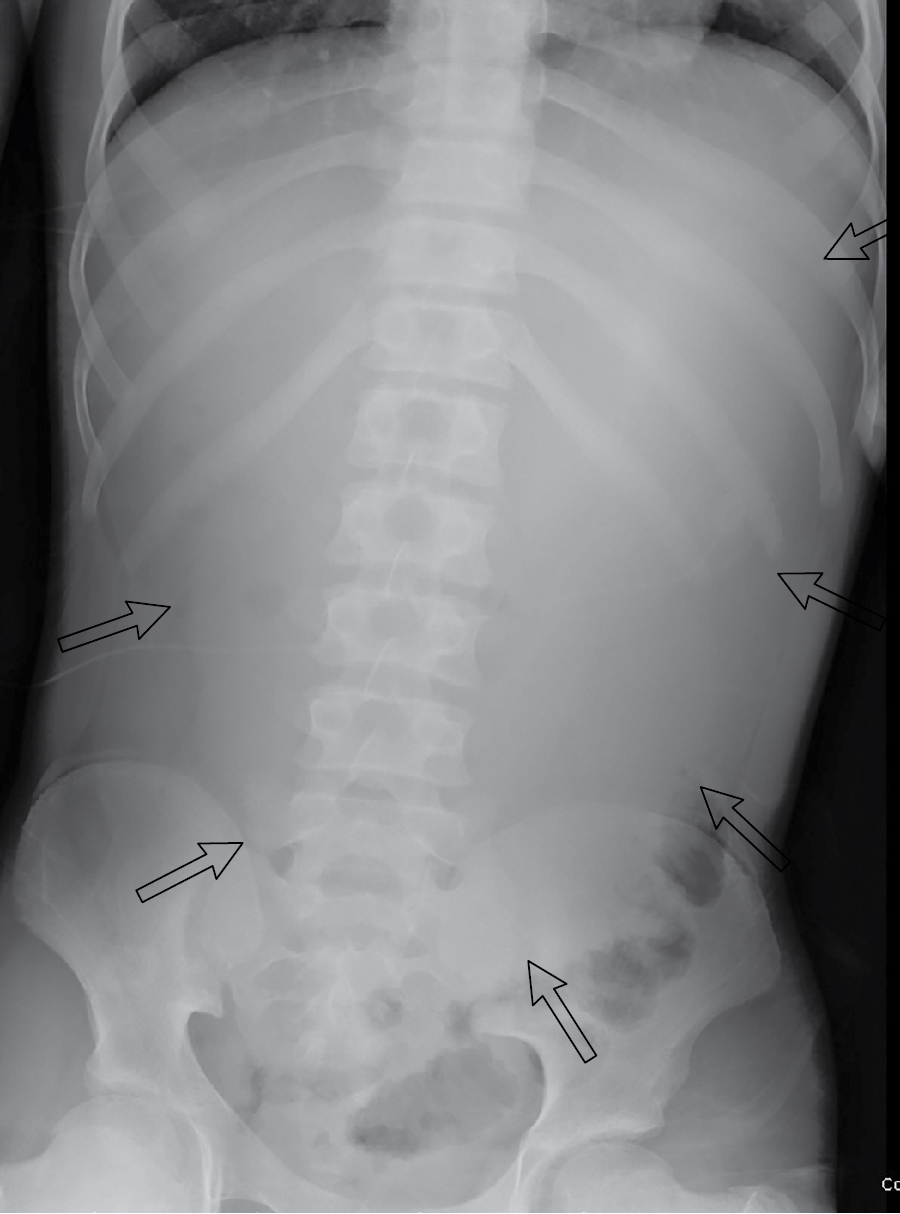
This child had plain radiographic imaging initially performed. The child was unable to cooperate for a two-view abdominal radiograph examination, despite pain medications; thus, a one-view (AP) radiograph was obtained ( Fig. 18.1 ). There is no obvious evidence of bowel obstruction, but there is a paucity of intestinal gas (a nonspecific finding), with appearance that is suspicious for fluid distension of the stomach.