IVIM Diffusion Model in Prostate Cancer
14.1 Introduction
Prostate cancer is the most common noncutaneous cancer type among men [1]. While the mortality rates have decreased as a result of serum prostate-specific antigen (PSA) screening in the last two decades, overdiagnosis of indolent cancer and underdiagnosis of lethal cancers remain a significant problem. Prostate magnetic resonance imaging (MRI) has been utilized to address this issue, and in large-scale studies it has been shown to improve diagnosis of lethal cancers without increasing the overdiagnosis of indolent disease [2, 3]. Widespread adoption of prostate MRI for cancer detection and staging in recent years has resulted in increasing calls for standardization in the acquisition and reporting [4]. Diffusion- weighted MRI (DW MRI) is an integral part of prostate MRI since it has been documented to improve lesion diagnosis and risk stratification.
Multiple studies [5, 6] have shown a negative correlation between the mean apparent diffusion coefficient (ADC) of tumors and their Gleason scores. The majority of the experience in prostate DW MRI literature is based on the use of ADC maps derived from the conventional monoexponential signal decay model. However, it is documented that the use of this relatively simplistic approach may not necessarily depict the diffusion characteristics of biological tissues, especially when a strong perfusion component is present in the diffusion signal. To account for these effects, the intravoxel incoherent motion (IVIM) model was proposed by Le Bihan et al. in the late 1980s [7, 8]. This biexponential model proposes that the microscopic translational motion of water in biological tissues has two components, molecular diffusion of water and microcirculation of blood in the capillary network, which is subsequently referred to as perfusion [7]. The IVIM model has been shown to better describe cancer biology in various applications, including prostate cancer, compared with the monoexponential approach [9–17]. Herein, we will discuss the clinical use of IVIM in prostate cancer diagnosis.
14.2 Prostate Cancer Detection Using the IVIM Model
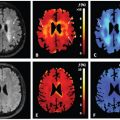
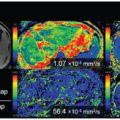
The IVIM model aims to explore DW signal decay at low b values, where both diffusion and perfusion effects are observed and may impact quantitative accuracy of ADC maps on which DW MRI relies heavily for prostate cancer detection and characterization [7, 18]. Different from conventional monoexponential signal decay DW modeling, the IVIM model can compartmentalize diffusion characteristics into quantitative metrics, such as molecular diffusion (D), microcirculation-related diffusion (pseudodiffusion, D*), and perfusion fraction (f). Several studies have explored the IVIM model and its parameters in prostate cancer detection (Fig.14.1).
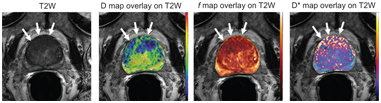
Figure 14.1 A 60-year-old man with a serum PSA of 44.81 ng/mL. An axial T2W MRI shows a large lesion in the anterior transition zone (arrows). Diffusion (D), perfusion fraction (f), and pseudodiffusion (D*) maps derived from the IVIM model (the included b values were 0, 188, 375, 563, 750, 1000, and 2000 s/mm2) confirm the presence of a large lesion in the anterior transition zone (arrows). A guided biopsy revealed a Gleason 4+4 prostate cancer within this large lesion.
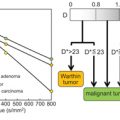
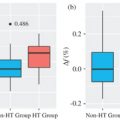
In early studies, the IVIM model was reported to be useful in differentiating prostate cancer from normal and benign prostatic hyperplasia (BPH) tissues. A study of 26 patients evaluated IVIM acquired with 10 b values between 0 and 1000 s/mm2. The results indicated that the ADC and D were significantly lower in cancer than in normal prostate and BPH and f derived from IVIM was also significantly lower in cancer than in normal prostate but not significantly different from BPH. Finally, D* was found to be similar in cancers, normal prostate, and BPH in that study. The authors indicated that a decrease in the perfusion fraction value may play a role in observed reductions of ADC values in prostate cancer, as well as decreased tissue diffusivity. Although they did not perform a stringent lesion-detection-based analysis, they observed that the IVIM model may offer additional information for tissue characterization in the prostate gland [15]. Shortly after that study another group studied the utility of perfusion fraction in prostate cancer diagnosis and compared the IVIM-derived perfusion fraction and diffusion coefficients with quantitative DCE parameters in 33 patients who underwent DW MRI acquired with five evenly spaced b values (0–750 s/mm2) followed by a targeted biopsy. They reported significant differences between normal tissue and tumor for IVIM-derived parameters, including perfusion fraction (3.7% vs. 7.2%) and diffusion coefficient (1.76 vs. 0.99), as well as DCE- derived parameters, including volume transfer constant (K trans) (0.18 min.–1 vs. 0.39 min.–1), fractional volume of extravascular- extracellular space (Ve) (26% vs. 32%), and plasma fractional volume (Vp) (3.4% vs. 8.4%). Given the moderately high correlation between IVIM perfusion fraction with K trans and Ve (r = 0.51 and = 0.46, respectively), the authors proposed that the perfusion fraction can be used to estimate the degree of tumor angiogenesis– related changes in the tissue and DCE MRI, with its requirement for intravenous gadolinium, could be eliminated; however, this is yet to be investigated by an independent study [16].
Several studies have compared ADC values derived from the standard monoexponential decay model with IVIM parameters. In one study with 53 patients, ADC values from monoexponential model were compared with anatomic T2-weighted (T2W) MRI and IVIM parameters (D, D*, and f) to distinguish prostate cancer from healthy tissue in the peripheral zone [19]. Authors reported that the T2, ADC, and D values were significantly lower in prostate cancers compared to healthy tissue whereas D
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree