Anatomy, embryology, pathophysiology
- ◼
Jaundice refers to the clinical sign of hyperbilirubinemia (>2.5 mg/dL), often manifesting with yellowing of the cutaneous surfaces, sclerae conjunctiva, and oral mucosa.
- ◼
Largely subdivided into nonobstructive (prehepatic and hepatic etiologies) and obstructive (posthepatic etiologies).
- ◼
Prehepatic causes:
- ◼
Hemolytic anemia.
- ◼
Hypersplenism.
- ◼
Artificial heart valves.
- ◼
Sepsis and low perfusional states.
- ◼
- ◼
Hepatic causes:
- ◼
Hepatocellular injury (e.g., viral hepatitis, drug-induced hepatitis, cirrhosis).
- ◼
Infiltrative disease (malignancy, steatohepatitis).
- ◼
Inherited conditions (e.g., Gilbert syndrome, Crigler-Najjar syndrome, etc.).
- ◼
- ◼
Posthepatic or obstructive jaundice:
- ◼
Benign causes:
- ◼
Choledocholithiasis.
- ◼
Biliary stricturing (infectious/inflammatory/iatrogenic causes, such as primary sclerosing cholangitis, posttrauma, postsurgical).
- ◼
Extrabiliary compression (e.g., Mirrizzi syndrome, fluid collections, pancreatic pseudocysts).
- ◼
- ◼
Malignant causes:
- ◼
Pancreatic, gallbladder, hepatocellular, and biliary malignancies.
- ◼
Portal lymphadenopathy (metastatic, infectious, or primary lymphoproliferative disorder).
- ◼
- ◼
Techniques
Ultrasound
- ◼
Ultrasound (US) is the preferred initial diagnostic modality for the assessment of the hepatobiliary system, particularly in the setting of acute right upper quadrant pain.
- ◼
US has a sensitivity of 48% to 100% and specificity of 64% to 100% for acute cholecystitis.
- ◼
The sensitivity of US in detecting gallstones is excellent (sensitivity >95%).
- ◼
The sensitivity of US in detection of biliary dilatation is 55% to 91%, demonstrating improved sensitivity with higher serum bilirubin and longer duration of jaundice.
- ◼
Common hepatic duct: Measured inner-inner wall, should measure less than 7 mm in patients under 60 years of age and less than 10 mm in patients older than 60 years of age.
- ◼
Common bile duct (CBD): In patients in their 40s, the normal value is about 4 mm, with the normal mean diameter increasing 1 mm per decade. The upper normal limit is 8.5 mm (or 10 mm postcholecystectomy).
- ◼
- ◼
US has similar sensitivity to computed tomography (CT) for detecting choledocholithiasis (75% in the dilated ducts, 50% in the nondilated ducts).
- ◼
US can be used for hepatocellular disease screening (such as hepatocellular carcinoma [HCC] screening, performed every 3–6 months).
Computed tomography/computed tomography-cholangiography
- ◼
Routine CT abdomen pelvis can evaluate the hepatobiliary system with a large field of view, with highly precise imaging during 3+ phases of hepatic enhancement.
- ◼
Optimal acquisition timing, in conjunction with thinner collimation, allows for improved lesion detection, lesion characterization and careful staging of various malignant etiologies (e.g., pancreatic malignancy, hepatic metastases, etc.).
- ◼
Routine contrast enhanced CT is moderately sensitive for the detection of choledocholithiasis (sensitivity 65%–88%).
- ◼
Routine contrast enhanced CT offers rapid and accurate staging.
- ◼
CT cholangiography:
- ◼
Biliary tree imaging for evaluation of postoperative bile leaks, strictures, choledocholithiasis, obstructing lesions and delineation of the biliary anatomy.
- ◼
Uses oral or intravenous (IV) cholangiographic contrast agents (e.g., IV meglumine iotroxate/Biliscopin).
- ◼
Contraindicated in severe hepatic, thyroid or renal dysfunctions, bilirubin less than 30 mmol/L, or iodinated-contrast allergies; radiation exposure.
- ◼
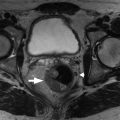
Magnetic resonance cholangiopancreatography ( fig. 19.1 )
- ◼
Noninvasive way to visualize intra-/extrahepatic biliary system and pancreatic duct.
- ◼
Performed on a 1.5 T or higher magnetic resonance imaging (MRI) scanner, using phased-array body coils.
- ◼
Requires 4 hours of fasting before the examination to reduce gastrointestinal secretions, minimize gallbladder motility/motion artifact and optimize gallbladder filling.
- ◼
Other modified techniques include:
- ◼
Secretin-stimulated magnetic resonance cholangiopancreatography (MRCP): Allows temporary dilation of the pancreatic duct, thus improving exocrine pancreatic reserve assessment and enhancing diagnostic capabilities of MRCP in pancreatic disorders.
- ◼
Functional MRCP: Improves anatomic delineation and enhancing of abnormal pancreaticobiliary variations and evaluation of pancreatic exocrine function.
- ◼

Protocols
Evaluation of GB anatomy:
- ◼
Axial and coronal breath-hold steady state fast spin echo (SE) T2-weighted images.
- ◼
Axial respiratory-triggered fat-suppressed T2-weighted imaging.
- ◼
Axial T1-weighted gradient-echo breath-hold in phase and out of phase.
- ◼
- ◼
MR cholecystography.
- ◼
Oblique radial steady state fast SE T2 weighted.
- ◼
Oblique right and left anterior steady state fast SE.
- ◼
Three-dimensional fat-saturated MRCP.
- ◼
- ◼
Contrast enhanced MR cholecystography.
- ◼
0.05 to 0.1 mL/kg of gadolinium injected over 1 to 2 min at 2 mL/s.
- ◼
- ◼
Dynamic contrast enhanced study.
- ◼
0.1 mmol/kg of gadolinium based contrast agent, at 2 mL/s, to cover the liver (run before, at 25 s, 60 to 70 s and 120 s after bolus administration).
- ◼
Specific disease processes
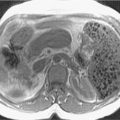
Choledocholithiasis
- ◼
Stone within the bile duct, either originating from the gallbladder or in situ in the biliary ducts ( Fig. 19.2 ).