- Conventional radiographs are useful in the acute setting
- Significant internal derangement can occur with normal XRs
- A lipohaemoarthrosis indicates an intra-articular fracture
- Popliteal artery injuries have to be excluded in supracondylar fractures and femorotibial dislocations
- CT should be performed for intra-articular fractures and in pre-operative planning
- If internal derangement is suspected, then MRI should be performed
- Ultrasound is rarely indicated in acute trauma except in suspected extensor injuries
Conventional radiographs (XRs) are initially performed for knee trauma but severe injuries may be present with little or no abnormality on XRs. If XRs show a lipohaemarthrosis, then CT or MRI is indicated to confirm the intra-articular fracture and potential associated injuries. If internal knee derangement is suspected, then MRI should be requested. MRI allows comprehensive assessment of soft tissue and bony injuries. CT is indicated for suspected intra-articular fractures and in pre-operative planning of complex bony injuries. In supracondylar fractures and knee dislocations, popliteal artery injuries need to be excluded, generally using CT angiography.
Anatomy
The knee is a hinge-type synovial joint formed by the articulation between the femoral condyles and tibial plateau. The two bones are separated by two C-shaped fibrocartilaginous structures: the medial and lateral menisci. The patella is a large sesamoid bone in the knee extensor mechanism. The quadriceps muscles form the quadriceps tendon, which inserts into the superior pole of the patella. The patella ligament extends from the inferior patella pole to insert onto the tibial tuberosity. The posterior surface of the patella articulates with the trochlear groove on the anterior surface of the femoral condyles and forms the patellofemoral joint (PFJ). The fibular head and posterolateral proximal tibia articulate at the proximal tibiofibular joint (Table 6.1).
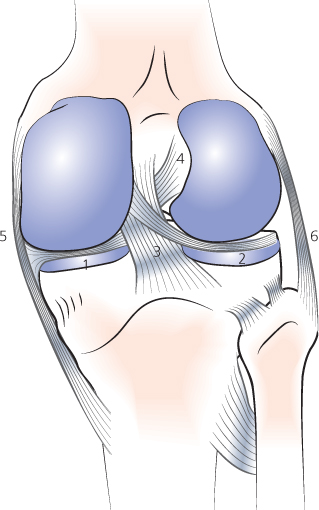
Ligaments and musculotendinous structures provide the knee with stability (Table 6.2; Figure 6.1). The knee is surrounded by multiple bursae. The suprapatellar bursa is continuous with the knee joint and distends in the presence of a joint effusion. It lies between the suprapatellar fat and prefemoral fat above the level of the patella (Figure 6.3).
Table 6.1 Timing of appearance and fusion of the secondary ossification centres about the knee.
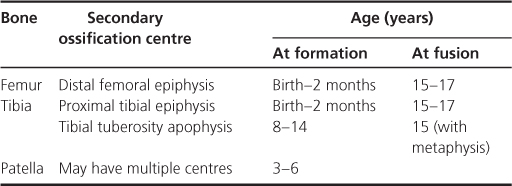
Table 6.2 Main supporting ligaments and musculotendinous structures of the knee.
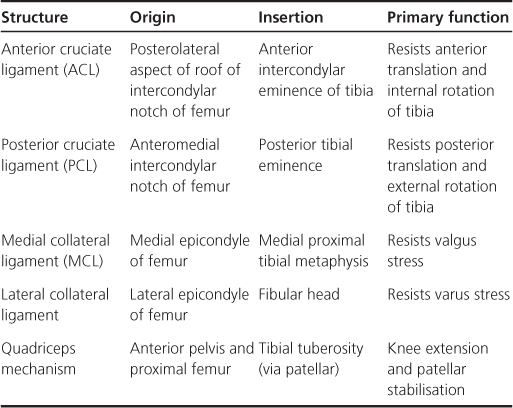
Figure 6.1 The posterior knee demonstrating normal ligaments and menisci: 1, medial meniscus; 2, lateral meniscus; 3, posterior cruciate ligament; 4, anterior cruciate ligament; 5, medial collateral ligament; 6, lateral collateral ligament.
- Anteroposterior (AP) (Figure 6.2) and lateral (lat) (Figure 6.3) projections are standard
- A skyline view (Figure 6.4) allows assessment of the patellofemoral articulation
- A tunnel or notch view is valuable to look at the intercondylar notch and to identify osteochondral fractures or intra-articular bodies
- Oblique views in internal and external rotation allow further evaluation of tibial plateau fractures and of the proximal tibiofibular joint
Figure 6.2 Normal anteroposterior radiograph of the right knee in an adult: 1, fibular head; 2 lateral tibial plateau; 3, medial tibial plateau; 4 and 5, lateral and medial tibial spines; 6, lateral femoral condyle; 7, medial femoral condyle; 8, intercondylar notch; 9, femur; 10, tibia; 11, patella.

Figure 6.3 Normal lateral knee radiograph of an adolescent. (a) 1, Fibula; 2 and 3, tibial spines; 4 and 5, lateral and medial femoral condyles (overlapping); 6, roof of intercondylar notch; 7, femur; 8, distal femoral growth plate; 9, patella; 10, tibial tuberosity; 11, fabella (sesamoid bone in the lateral head of gastrocnemius); (b) 12, quadriceps tendon (and distal muscle belly); 13, patellar ligament; 14, prefemoral fat pad; 15, suprapatella bursa; 16, suprapatella fat pad; 17, Hoffa’s fat pad.
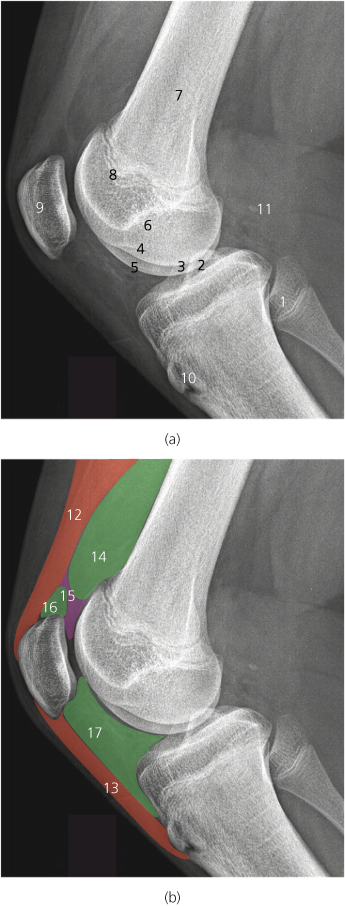
Figure 6.4 Normal skyline view of the right knee in an adult: 1, lateral patellar facet; 2, lateral trochlear facet (anterior lateral femoral condyle; 3, medial patellar facet; 4, medial trochlear facet (anterior medial femoral condyle).

ABCs systematic assessment
- Adequacy—check correct views have been obtained
- Alignment—check femorotibial alignment and patellar height
- Bones—trace the contours of all the bones
- Cartilage and joints—joint spaces should be uniform in width
- Soft tissues—change windows to look for soft tissue swelling, effusion, and fat/fluid level
Adequacy
Routine AP and lat views should be obtained. Following acute trauma, the lat view should be performed with a horizontal beam so that a fat-fluid level can be identified. View the lat view first.
Lateral view
Soft tissues (on this occasion, S before ABC!)
Separation of the suprapatellar and prefemoral fat pads (>5 mm) indicates an effusion (Figure 6.5). The presence of a fat-fluid level (lipohaemathrosis) within the joint is pathognomonic of an intra-articular fracture (causing bleeding and therefore a haemoarthrosis), with leakage of marrow fat into the joint (hence the lipohaemoarthosis) (Figure 6.6).
Figure 6.5 Lateral radiograph of the knee in a 13-year-old boy following acute knee injury. There is a large effusion (arrows). Note how the effusion separates the suprapatellar (P) from the prefemoral fat pad (F).
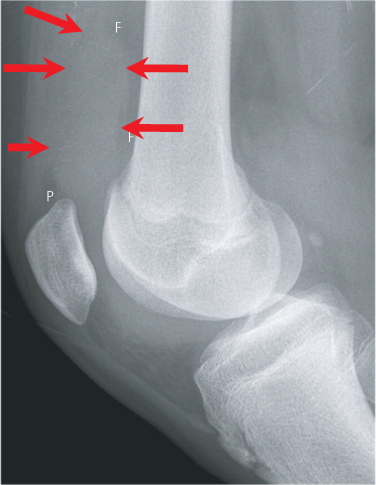
Figure 6.6 Horizontal beam lateral radiograph of the knee in a patient with a tibial plateau fracture following a road traffic accident. Note the lipohaemarthrosis (fat-fluid level—arrows), which indicates the presence of an intra-articular fracture. The comminuted tibial plateau and associated fibular head fracture are also identified.

Alignment
On a lateral view, anterior tibial displacement indicates rupture of the anterior cruciate ligament, while posterior displacement indicates rupture of the posterior cruciate ligament.
On a lateral view with the knee in 20–30° flexion, the ratio of the patella tendon length to patella length should be in the range 0.8–1.2 (Figure 6.7). A high riding patella (patella alta) may be a congenital variant or the result of rupture of the patella tendon (Figure 6.8). A low riding patella (patella baja) may be a congenital variant or the result of rupture of the quadriceps tendon.
Figure 6.7 Lateral view of a normal knee demonstrating measurement of the Insall Salvati ratio for patellar height. The ratio is measured as the patellar ligament length divided by the maximum patellar length and the ratio normally lies in the range 0.8–1.2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree