Overview
As with other larger joints, ultrasound is most useful when the patient’s symptoms are localized to a relatively specific area. More diffuse symptoms suggest internal derangement due to meniscal, cruciate and cartilage injuries. These are diagnosed by MRI with relative ease and, although there have been efforts to use ultrasound to depict these structures, it is not sufficiently reliable for general diagnostic use. Until meniscal or cruciate injury can be confidently excluded, ultrasound will always play a subservient role to MRI. This is not true of trauma to the extraarticular structures, though the possibility of combination injuries within the joint must always be borne in mind. Patients with isolated injuries of the patellar tendon, quadriceps tendon and iliotibial band (ITB) can be reliably assessed. The medial collateral and lateral collateral ligaments are also readily accessible to ultrasound examination, though are more often associated with meniscal injury. Masses, both cystic and solid, are common around the knee and ultrasound affords a cheap and reliable method of investigation.
The anterior knee is best examined with the patient recumbent and the knee extended. A dynamic examination can be added later, but the extended knee relaxes the extensor mechanism and does not compress any abnormal vessels that may present. This position can also be used to examine the medial structures and the ITB with ease. The posterolateral corner, proximal tibiofibular joint and posterior structures are best examined with the patient prone.
Position 1: Anterior Knee
Imaging Goals
- 1.
Identify the patellar tendon and Hoffa’s fat pad.
- 2.
Identify all four components of quadriceps.
- 3.
Locate patellofemoral ligaments and review the retropatellar surface.
Technique
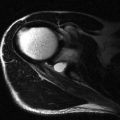
The patellar tendon is very readily assessed with ultrasound ( Fig. 21.1 ). It has the striated predominantly reflective appearance typical of normal tendon tissue. The low-reflective areas represent the tendon fibres and the brighter material is the interspaced connective tissue. In long axis, the tendon measures approximately 5 cm. In cross section, it is considerably wider than it is thick, cross-sectional dimensions 26 × 4 mm are typical. It is convex in both its anterior and posterior margins. There is no tendon sheath but a paratenon is present.

The normal appearance of the proximal attachment of the patellar tendon is quite variable. Sometimes it is a similar dimension to the tendon itself whilst in other individuals it broadens to a triangular shaped insertion. Some of these variations may be related to the patient’s level of activity. The distal tendon more commonly shows some broadening at the insertion onto the tibial tubercle. There are transitional changes between the fibrous structure of the tendon and the bone, which can sometimes be seen with high-resolution ultrasound. The fibrous tendon transitions through fibrocartilage, hyaline cartilage and, finally, bone. Where the tendon lies close to the proximal tibia, some entheseal cartilage may be apparent on the undersurface of the tibia with sesamoid cartilage present on the tendon side. These different cartilage components are more readily visible in some patients than in others but it is rare to see all components together.
The tibial enthesis is also accompanied by two bursae: the superficial and the deep infrapatellar bursa. Fluid is more commonly seen in the deep infrapatellar bursa. Gentle flexion and extension of the knee while examining the bursa in the axial plane makes the fluid more readily visible. The tendon’s superficial relationship is usually subcutaneous fat, although in its upper portion a small quantity of fluid may be identified in the prepatellar bursa and inferiorly in the superficial component of the infrapatellar bursa. The posterior relation of the patellar tendon is Hoffa’s fat pad. This has a bright reflective appearance typical of fat. It is fairly homogeneous, containing a few blood vessels only.
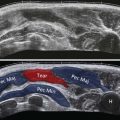
The other important tendon of the extensor mechanism is the quadriceps tendon. This has several components and care must be taken not to concentrate only on the most obvious central component. To demonstrate these different parts, it is best to begin with the probe in long axis centrally positioned over the upper border of the patella ( Fig. 21.2 ). The typical bright, striated appearance of the central part of the tendon will be seen beneath. Often three or four distinct bands are visualized with interspaced reflective connective tissue. The upper bands represent the contribution from rectus femoris and the lower the components of vastus intermedius. There are contributions from vastus medialis and lateralis, which also have separate insertions on the superomedial and superolateral patella. With the knee fully extended, some kinks may be evident in the tendon, leading to areas of altered reflectivity. These disappear when slight flexion is applied, although the knee must be returned to full extension prior to assessing Doppler activity. Deep to the tendon, there is a triangle of fat, the suprapatellar fat pad. This fat pad is separated from the prefemoral fat by the synovial knee joint. A small quantity of fluid is not infrequently identified within the joint.

The probe is then moved laterally, the upper end of the probe a little more than the lower end, to align along the tendon of vastus lateralis ( Fig. 21.3 ). This has a broader insertion along the superolateral aspect of the patella with fibres contributing to both the central tendon and the lateral retinaculum. The probe is finally moved medially, once again the proximal end more than the distal end, to align along the tendon of vastus medialis ( Fig. 21.4 ). The musculotendinous junction of vastus medialis is lower than vastus lateralis and the tendon arises from the deep rather than the superficial component of its parent muscle. The muscle fibres visible here make up the vastus medialis obliquus.


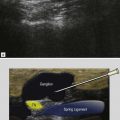
Both patellofemoral ligaments should be examined in turn and each followed posteriorly to where they form the medial collateral ligament and the ITB respectively. They are traced forwards to their insertions along the medial ( Fig. 21.5 ) and lateral border of the patella ( Fig. 21.6 ). The retropatellar surface can also be examined, although not in its entirety. The medial facet is easier to see and gentle medial pressure on the lateral border of the patella improves visualization. This is particularly useful when patellar dislocation is suspected and cartilage injury in this location may be found. The presence of fluid within the joint improves visualization. The patella can be tracked during flexion and extension using ultrasound, although more accurate techniques have been described particularly using MRI. Patellar maltracking is best assessed with the quadriceps under tension. This can be achieved either by attaching weights to the patient’s shin that they then have to lift or asking the patient to extend the knee against the resistance of the examiner’s hand.


Position 2: Medial Knee
Imaging Goals
- 1.
Identify the medial collateral ligament and meniscus.
- 2.
Identify semimembranosus and its complex insertion.
- 3.
Locate the pes anserine tendons.
Technique
The principal ligament on the medial aspect of the knee is the medial collateral ligament. This is examined first in its long axis by placing the probe over the medial aspect of the knee and locating the joint space ( Fig. 21.7 ). This is achieved by following the bony contour either of the femur distally or tibia proximally. Move the probe to approximately the midpoint of the medial aspect of the joint and the medial collateral ligament will be found. It is composed of two layers; the more important superficial layer is usually the first to be recognized. This arises several centimetres above the joint from a triangular shaped attachment to the medial femoral condyle. It inserts approximately 5 cm below the joint where the tibial attachment is thinner than the femoral attachment. It has the typical ultrasound appearance of a ligament with clearly defined striations. The most common site of injury of the ligament is proximal, close to the femoral origin. The deep component of the ligament is a much thinner structure composed of two parts. The proximal part is the meniscofemoral ligament and the distal part is the meniscotibial ligament. As would be expected from their names, these ligaments are attached to the medial meniscus.