Imaging of the larynx is a challenge. Motion is a constant problem because breathing and swallowing are very difficult to control, particularly in patients with lesions that impinge on the airway. The patient’s larynx moves slightly with each breath. Despite the difficulties, imaging can still provide important information regarding potential involvement of deeper soft tissues and cartilage.
Imaging must be considered in view of the capabilities of modern endoscopy. As the technology of imaging has progressed, so too has the instrumentation available for direct visualization. Almost all of the mucosa can be examined very effectively. To be relevant, imaging must provide information that cannot be had by direct visualization. Thus the intent of the radiologist in most cases is to evaluate the deeper tissues. In some cases a bulky lesion of the upper larynx can block the view of the lower larynx, and imaging can assist in defining the caudal extent of disease. Tumors of the lowermost part of the larynx may be difficult to visualize, obscured by the vocal folds.
The radiologist must be familiar with the anatomy. The behavior of various disease processes and particularly growth patterns of cancer are extremely important. The radiologist must also be familiar with the available therapeutic options to emphasize the information that will be important in making clinical decisions. There is variability of opinion about some of the more recent surgical strategies, and it is important to work closely with the individual surgeons to ensure that the precise regions of concern are addressed.
This chapter begins with a section on anatomy, including the normal appearance in the various imaging planes. A brief discussion of the technical considerations of applying computed tomography (CT) and magnetic resonance imaging (MRI) to the task of examining the larynx is followed by sections on imaging of various pathologic conditions. The important clinical considerations in each disease will be stressed.
Anatomy
The larynx is a system of mucosal folds supported by a cartilaginous framework. Tension and movement of the mucosal folds is effected by the actions of small muscles pulling against this cartilaginous framework.
Mucosa
Clinical descriptions of lesions of the larynx emphasize the mucosal anatomy, so the mucosa is a good starting point for the present discussion.
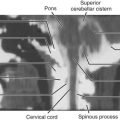
When viewed from superiorly (the view of the endoscopist), the first landmark seen is the epiglottis ( Fig. 25-1 ). The upper edge of the epiglottis represents the most superior limit of the larynx. The epiglottis is the anterior boundary of the entrance into the larynx. Anteriorly two small sulci, the valleculae, separate the free portion of the epiglottis from the base of the tongue ( Fig. 25-2 ). From the lateral margin of the epiglottis, the aryepiglottic (AE) folds curve around to reach the small interarytenoid notch. Together these structures complete the boundaries of the airway at the entrance into the larynx.


The inner mucosal surface of the larynx, or endolarynx, can be thought of as the working part of the organ. Two prominent parallel folds stretch from front to back along the lateral aspect of each side of the airway (see Figs. 25-1 and 25-2 ). These are the true and false vocal cords or folds. They are in the horizontal plane. The true vocal fold (the glottis) is the key functional component in the generation of voice and has a fine edge at the medial margin. The more superiorly placed false vocal fold has a more blunted medial surface. Separating these two folds is one of the most important landmarks in the larynx, the ventricle. The ventricle is a thin cleft between the true and false folds, stretching from the most anterior limit of the fold to a point close to the posterior limit of the larynx.
Above the false vocal fold the mucosa sweeps upward and outward to the AE folds. Inferiorly the mucosa covering of the true fold sweeps downward into the subglottic area, eventually merging smoothly with the mucosa of the trachea.
A final important mucosal landmark is the anterior commissure. This is the point where the true vocal folds converge anteriorly to attach to the inner (posterior) surface of the anterior angle of the thyroid cartilage.
The three parallel structures—true vocal fold, false vocal fold, and ventricle—organize the larynx into three regions: the supraglottis, the glottis, and the subglottis.
The true fold or cord is the glottis. The glottic region of the larynx extends from the upper surface of the true fold to a line somewhat arbitrarily chosen as being 1 cm below the level of the ventricle. The subglottic region is between this arbitrary line and the inferior edge of the cricoid cartilage, the lower margin of the larynx. There is no defined mucosal structure representing the exact boundary or separation of the glottic and subglottic regions.
The supraglottic region is the part of the larynx above the ventricle. This region includes the false folds, epiglottis, and AE folds.
Laryngeal Framework
The laryngeal cartilages represent the supporting framework of the larynx. The major cartilages include the cricoid, thyroid, arytenoid, and epiglottic cartilages ( Fig. 25-3 ). The smaller cartilages, the corniculate and cuneiform, reside in the AE fold and are not of particular importance to the radiologist.

The cricoid cartilage is the foundation of the larynx and is the only complete ring. The posterior part is larger than the anterior, giving the cartilage the appearance of a signet ring facing posteriorly. The upper margin of the cricoid slopes inferiorly toward the anterior midline. The upper margin of the larger posterior part of the cricoid cartilage reaches the level of the cricoarytenoid joint and the true vocal fold. The lower margin of the cricoid cartilage represents the lower margin of the larynx.
The thyroid and arytenoid cartilages articulate with the cricoid cartilage. The thyroid cartilage is large and can be thought of as forming a shield for most of the inner larynx. The arytenoid cartilages perch on the superior edge of the posterior cricoid cartilage.
The arytenoid cartilage is situated in the posterior larynx and vertically crosses the level of the ventricle. The vocal process at the level of the true vocal fold projects anteriorly from the lowermost part of the arytenoid cartilage. Because of its characteristic shape and position, the arytenoid cartilage can help localize the ventricle on axial scanning. This is most helpful with CT, because the vocal process may be directly visualized. The upper margin of the arytenoid is at the level of the lower false fold just above the ventricle. The vocal process is at the level of the true fold just below the ventricle. Indeed, the vocal ligament, which represents the medial margin of the true vocal fold, attaches to the vocal process.
The epiglottic cartilage, with the exception of its superior tip, is contained within the external framework of the larynx. This cartilage is made of elastic fibrocartilage and does not ossify. Grossly this cartilage has multiple perforations resembling more a mesh than a solid plate, so the epiglottic cartilage is not a major barrier to tumor spread. Inferiorly the epiglottic cartilage is connected to the inner surface of the anterior part of the thyroid cartilage by the thyroepiglottic ligament.
Muscles and Ligaments
The cartilages are connected by a system of muscles and ligaments. Several muscles are mentioned in the remainder of the chapter; one deserves special attention in a discussion of larynx imaging. The thyroarytenoid muscle (TAM) stretches from the arytenoid cartilage to the inner surface of the anterior thyroid cartilage ( Fig. 25-4 ; see Fig. 25-2 ). This muscle parallels the true fold and makes up the bulk of the true vocal fold. The characteristic shape of this muscle allows identification of the true vocal fold level at imaging.

The cricothyroid and thyrohyoid membranes span the greater part of the intervals between the cricoid cartilage, thyroid cartilage, and hyoid bone and represent, along with the cartilages, the outer limits of the larynx. Notably the cricothyroid membrane is considered to be incomplete lateral to the anterior midline.
Two membranes are found just deep to the mucosa. The conus elasticus (also called the cricovocal ligament or lateral cricothyroid ligament ) stretches from the vocal ligament to the upper margin of the cricoid cartilage. Some descriptions include the membrane attaching to the inner surface of the ring as well. This membrane or fascial layer merges with the anterior cricothyroid ligament in the anterior midline.
A similar structure is seen in the supraglottic larynx. A thin ligament called the ventricular ligament is found in the lower margin of the false fold, and the quadrangular membrane sweeps superiorly from the ventricular ligament and terminates in the AE fold.
The fan-shaped hyoepiglottic ligament stretches from the epiglottis to the hyoid and divides the supraglottic larynx into a superior (suprahyoepiglottic) area and an inferior (infrahyoepiglottic) area.
Spaces
The paraglottic space and the preepiglottic space are found between the mucosal surface and the cartilaginous outer limit of the larynx.
The paraglottic space is found laterally and represents much of the soft tissue wall of the larynx ( Figs. 25-5 and 25-6 ). Although descriptions of the paraglottic space vary, this discussion will use Tucker’s original descriptions, with the medial boundary represented by the conus elasticus and quadrangular membrane. The lateral boundary is the external skeleton of the larynx, predominantly formed by the inner cortex of the thyroid cartilage. At the level of the supraglottic larynx, the paraglottic space is predominantly filled with fat. Below the ventricle the TAM fills the paraglottic region.


A small recess of the ventricle extends upward into the paraglottic space of the supraglottic larynx. This is called the laryngeal saccule or appendix. This structure is within the paraglottic fat lateral to the quadrangular membrane.
The preepiglottic space is between the epiglottis posteriorly and the thyroid cartilage and thyrohyoid membrane anteriorly.
The hyoepiglottic ligament forms the roof of the preepiglottic and paraglottic spaces.
Imaging Considerations
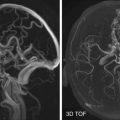
The radiologist can use either CT or MRI to image the larynx. MRI has a theoretical advantage in differentiating soft tissues, but CT has a definite advantage in speed. Radiologists at this institution begin with CT and occasionally do limited MRI to clarify a specific issue.
Multidetector CT can cover the entire larynx in just a few seconds. The thin slice thickness allows multiplanar reformatted images comparable in quality to direct imaging (see Fig. 25-6 ). Because the scan can be done so quickly, the contrast can be ideally planned for best visualization of the anatomy and the pathology. MRI can separate or distinguish various soft tissues slightly better than CT. This may allow better analysis of potential cartilage invasion and has been considered to have an advantage in defining the tumor-muscle interface.
Motion artifact is a significant problem when imaging the larynx. CT scanning avoids the problem by using fast imaging. The multidetector acquisition covers the larynx in a few seconds. The examination can be performed during slow shallow respiration, or the scan can be done with the breath held.
More elaborate schemes are required for MRI studies. At this institution the patient practices breathing with the abdominal muscles rather than the chest muscles. This is done before the examination begins, usually before the patient is put on the examination table. Specialized neck coils or surface coils are positioned so that any chest movement does not bump the coil. Although speed of imaging is always an advantage, some have recommended using multiple excitations on the T1-weighted sequence. This gives longer imaging times but averages out some of the motion.
At this institution, contrast material is usually used when imaging tumor cases. Gadolinium combined with fat suppression can emphasize tumor margins. Fat suppression with the T2-weighted images can help in the evaluation of cartilage involvement.
Imaging emphasizes the importance of the ventricle. Axial images are taken along the plane of the ventricle. The position of the ventricle is estimated in axial images by the appearance of the cartilages or by the transition from fat to muscle in the paraglottic region. The coronal images are perpendicular to the ventricle. Even if the ventricle is not actually seen, its position can be predicted by the transition from fat to muscle in the paraglottic space.
Pathology
Most laryngeal imaging is done for evaluation of tumors or for assessment of patients with trauma to the larynx. The tumors can be subdivided into mucosal and submucosal groups. In most instances the larynx is directly visualized—if not by endoscopy, at least by mirror—and the radiologist should pursue information that is not obtainable by direct visualization.
Mucosal Tumors
Most tumors evaluated by imaging are squamous cell carcinomas arising from the mucosa of the larynx. With the possible exception of extremely rare lesions arising deep within the ventricle, these tumors are almost always detected before imaging. Indeed, imaging cannot currently rule out a small malignancy and so is not a substitute for direct visualization.
The otolaryngologist can completely assess smaller lesions. The margins of a small tumor may be readily visible and no further information is required. Imaging is important for patients with moderate-sized tumors, in whom some type of voice-sparing therapy is considered. Such treatment options include partial laryngectomies, radiotherapy, or organ-sparing strategies that include radiation and chemotherapy as an initial approach. The feasibility of these therapies depends on the origin and extent of the tumor. In very extensive tumors where total laryngectomy is likely, imaging gives a baseline evaluation and helps evaluate the lymph nodes. Ultrasound has been useful in evaluating lymph nodes, and many institutions perform positron emission tomography (PET)/CT to evaluate nodes and possible distant metastases. PET/CT will also find occasional second primaries.
The precise information required by the various clinicians varies. Perhaps the most precise anatomic analysis is targeted at the feasibility of doing a surgical partial laryngectomy. Originally these voice-sparing partial laryngectomies were performed through open neck approaches. Now more partial resections are done via endoscope using lasers. Many patients who would have been candidates for open partial laryngectomies are now treated with various chemoradiation (chemoRT) organ-preserving protocols. Even though open partial laryngectomies are done much less common than previously, we still use the landmarks described for these techniques in our evaluation of larynx cancers. This approach with very slight modifications provides the information required by any of the therapeutic strategies considered.
The discussion of imaging of carcinoma of the larynx is organized based on the site of origin of the tumor.
Supraglottic Tumors.
The classic voice-sparing surgical option for supraglottic squamous cell carcinoma is the supraglottic laryngectomy ( Fig. 25-7 ). The resection is made along the ventricle, and the entire supraglottic larynx is removed, leaving at least one and usually both arytenoid cartilages. The patient retains the true folds and so generates voice in the usual manner with the normal neuromuscular mechanisms. The protective function of the supraglottic larynx, particularly the epiglottis, is lost, and the patient must learn to swallow without aspirating. The classic open surgical partial laryngectomy is done via open skin incisions, but currently larynx surgeons perform these partial resections endoscopically using lasers. The anatomic landmarks emphasizing the ventricle are the same for both approaches.

Tumor crossing the ventricle is the primary contraindication for the standard supraglottic laryngectomy ( Box 25-1 ). The incision passing along the ventricle would cut through tumor. Tumor growing along the mucosa to reach the true vocal fold may be obvious at direct visualization. Tumors may invade into the deeper tissues laterally and follow the paraglottic space around the ventricle into the lateral edge of the true vocal fold. This type of spread is unusual as an isolated phenomenon but should be checked when imaging a supraglottic tumor.
- •
Tumor extension onto the cricoid cartilage
- •
Bilateral arytenoid involvement
- •
Arytenoid fixation
- •
Extension onto the glottis or impaired vocal cord mobility
- •
Thyroid cartilage invasion
- •
Involvement of the apex of the piriform sinus or postcricoid region
- •
Involvement of the base of the tongue more than 1 cm posteriorly to the circumvallate papillae
Axial imaging parallels the ventricle and therefore is somewhat limited in precisely identifying the level of this key structure. The paraglottic space at the false vocal fold level is predominantly fat, but at the true vocal fold level is predominantly muscle. The transition between the two represents the approximate level of the ventricle. If a normal slice can be found below the tumor but still within the supraglottic larynx, the supraglottic laryngectomy is technically possible ( Fig. 25-8 ). If the tumor can be identified at the level of the vocal fold as well as in the supraglottis, the patient cannot have the standard supraglottic resection ( Fig. 25-9 ). If surgery is chosen as the therapy, the usual procedure would be a total laryngectomy although some more extensive procedures have been described, taking larger parts of the larynx (see later). As endoscopic resections advance, new strategies can extend the ability to take tumors at lower levels. Describing the most inferior extent of the tumor relative to the ventricle is very important in such cases. Alternatively these patients may be considered for organ-sparing chemoRT protocols.


On axial images, the lateral edge of the TAM should be carefully examined for the earliest evidence of transglottic (from false fold to true fold) spread. A narrow extension of the paraglottic fat is often seen along the outer (lateral) margin of the muscle (see Fig. 25-9 ). Tumor spreading around the ventricle will grow into this fat and eventually appear to “pry” the muscle away from the thyroid cartilage. Coronal images are perpendicular to the ventricle and may also be helpful in showing the relationship between tumor and the lateral aspect of the true vocal fold.
Tumor can be distinguished readily from the fat in the supraglottic paraglottic space. The interface between tumor and muscle at the true fold level is more difficult to visualize. MRI studies have the advantage of better tissue differentiation using various pulse sequences, but this advantage can be realized only if the patient is able to control motion ( Fig. 25-10 ). In our experience the ability to optimize the contrast injection with CT scanning may allow good differentiation of the tumor from muscle, diminishing the soft tissue advantage of MRI.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree