Lateral elbow pain
Medial elbow pain
Lateral epicondylitis
Cervical radiculopathy
Radial tunnel syndrome
OCD lesion of the radiocapitellar joint
Synovial elbow plica
Posterolateral rotatory instability
Medial epicondylitis
Cervical radiculopathy
Flexor-pronator muscle strain/tear
Ulnar collateral ligament injury
Ulnar neuritis
Valgus extension overload
Radiographic Evaluation
Though lateral and medial epicondylitis both remain clinical diagnoses, imaging is oftentimes included in the diagnostic workup of patients with either lateral or medial elbow pain. Plain radiographs, including anteroposterior, lateral, and oblique views of the elbow, are frequently obtained and usually are normal. However, calcifications within the soft tissues about the lateral epicondyle may be noted in 22–25 % of patients with lateral epicondylitis, though this has not been found to have a prognostic implication [10].
Magnetic resonance imaging (MRI), while not an essential part of the diagnostic workup, can be a useful adjunct in assessing both conditions. In particular, MRI allows for evaluation of both the surrounding tissue structures and the intra-articular surface, which helps determine if any other potential causes of elbow pain may be present. This is especially useful in patients with medial elbow pain, as the integrity of the UCL can be determined. The typical appearance on MRI shows abnormally high signal intensity on T2-weighted and short TI inversion recovery (STIR) sequences within a thickened common extensor or flexor-pronator tendon origin for lateral and medial epicondylitis, respectively [14]. Overall, MRI has a 90–100 % sensitivity and a 83–100 % specificity for detecting epicondylitis [15]. It may be performed either with or without intra-articular gadolinium contrast injection.
Treatment Options and Outcomes
The majority of cases of both lateral and medial epicondylitis respond well to conservative management. While no consensus treatment algorithm currently exists for either condition, multiple options have been utilized previously. This includes an initial phase of rest, ice, and nonsteroidal anti-inflammatory (NSAIDs) medications. This is often followed by a course of physical therapy, the use of counterforce bracing, and/or corticosteroid injection [13]. Other modalities that have been investigated include extracorporeal shock wave (ECSW) therapy [16–18], platelet-rich plasma injection [19], and use of low-dose thermal ablation devices [20]. While most patients respond well to nonoperative management, historically noted at up to a 90 % recovery rate within 1–2 years [9, 10], surgical treatment of recalcitrant disease is sometimes required. Bot et al., however, recently found that, while most patients (90 %) obtained at least some improvement with conservative treatment for lateral epicondylitis at 1 year follow-up, only 13 % reported a full recovery at 3 months and 34 % at 1 year [21]. This may indicate an expanded surgical role in the treatment of both lateral and medial epicondylitis.
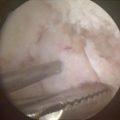
Regardless of these prior findings, a minimum of 3–6 months of nonoperative treatment is recommended prior to pursuing surgical treatment for either lateral or medial epicondylitis. Traditionally, surgical options involved open debridement of the involved tissue, such as those previously described by Bosworth in 1955 [22], as well as Nirschl and Pettrone in 1979 [10] in treating lateral epicondylitis. Percutaneous approaches for ECRB release have also been described [23, 24]. However, with the advances made in arthroscopic surgery of the elbow, there has been an increased focus on arthroscopic management of epicondylitis. Baker et al. initially reported on 40 patients (42 elbows) with recalcitrant lateral epicondylitis who underwent arthroscopic debridement of the diseased tissue, often combined with decortication of the lateral epicondyle [25]. These arthroscopic techniques have continued to evolve beyond simple debridement, with ECRB repair and plication utilizing both simple suture and suture anchor devices being described [20].
Given its increased prevalence, surgical outcomes regarding the arthroscopic management of lateral epicondylitis have been investigated more extensively than has medial epicondylitis. Several studies comparing open and arthroscopic debridement techniques for the treatment of lateral epicondylitis have been performed. While overall equivalent clinical results have been oftentimes noted, those treated arthroscopically were noted to return to work earlier without restrictions [25–28]. More recently, however, Solheim et al. noted that patients undergoing arthroscopic release had a better QuickDASH score than those that underwent an open surgical debridement [29]. An additional advantage of arthroscopic treatment is that a full intra-articular assessment of the elbow joint can be performed and any concomitant pathology addressed during the same surgical setting, as concurrent intra-articular pathology has been found in up to 44 % of cases [30].
While arthroscopic treatment of lateral epicondylitis has become more prevalent and accepted, concerns exist over the arthroscopic treatment of medial epicondylitis. This is due to the proximity of both the ulnar nerve and the medial ulnar collateral ligament to the flexor-pronator origin at the medial epicondyle. On the other hand, cadaveric models have indicated that these structures lie at a far enough distance away from the debridement site and that arthroscopic debridement for medial epicondylitis can be performed at a low risk of injury to these structures [31]. Relative contraindications to elbow arthroscopy do exist, however, including prior medial elbow surgery with ulnar nerve transposition or the presence of ulnar nerve subluxation. Absolute contraindication includes active infection.
Case Presentation: Concurrent Lateral and Medial Epicondylitis
A 38-year-old, right-hand dominant female presented with a long-standing history of elbow pain. Her pain was localized over both the lateral and medial aspects of her elbow. This had been present over the past several years, and she had been treated by her primary care physician with anti-inflammatory medications, counterforce bracing, and intermittent corticosteroid injections. Orthopedic consultation had been obtained, and a sequence of injections had been given with some temporary relief, but each time, the pain returned and thought to be more severe with each recurrence. Her pain symptoms had become constant, with worsening both at night and with lifting activities. She denied any traumatic etiology of her symptoms and had not had any previous surgical procedures to her right elbow.
Upon her initial presentation to our orthopedic clinic, her physical examination showed tenderness to palpation about both the medial and lateral epicondyle. She had full active and passive range of motion to elbow flexion and extension, as well as forearm pronation and supination. She had increased pain with active resisted wrist extension over her lateral elbow and with active resisted wrist flexion over her medial elbow. No elbow instability was present clinically, with negative varus/valgus stress testing and a negative lateral elbow pivot shift. She had full motor strength in all key groups and had no sensory deficits or complaints of numbness. She had a negative Tinel’s test over the cubital tunnel.
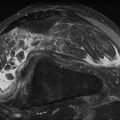
Radiographic assessment was obtained including two view X-rays of the right elbow. These were found to be normal. An MRI obtained by her orthopedic surgeon was reviewed. This revealed the presence of increased signal both within the tendinous portion of the flexor-pronator mass medially and within the common extensor mass laterally, consistent with both medial and lateral epicondylitis, as seen in Fig. 21.1a–d. Further conservative recommendations were made at her initial appointment, including a course of physical therapy, topical and oral anti-inflammatory medications, a wrist brace, and repeat corticosteroid injections to both the medial and lateral epicondyle. This course of treatment provided good initial relief, but her symptoms returned fully within 3 months. Surgical intervention in the form of elbow arthroscopy was then offered, and the patient elected to pursue.


Fig. 21.1




Coronal T1-weighted and STIR MRI images indicating increased signal intensity within the common extensor tendon origin (a, b) and the flexor-pronator mass (c, d). Additionally, the intra-articular surfaces are noted to be normal (a, b), as is the ulnar collateral ligament (c, d) (a–d: Published with kind permission. Copyright © Felix H. Savoie, III, MD)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree