Key Points
- •
A qualitative determination of left ventricular systolic function can sufficiently guide point-of-care decisions and can be accurately accomplished by providers after brief, focused training in cardiac ultrasound.
- •
Qualitative assessment of left ventricular systolic function should be categorized as hyperdynamic, normal, reduced, or severely reduced based on evaluation of endocardial excursion, myocardial thickening, and septal motion of the anterior leaflet of the mitral valve in multiple views.
- •
Determination of left ventricular diastolic function, regional wall motion abnormalities, and structural abnormalities requires additional training.
Background
Left ventricular (LV) systolic dysfunction can cause or significantly complicate acute illness. In undifferentiated shock, point-of-care LV assessment has been shown to increase accuracy in diagnosis and treatment decisions through a qualitative approach to classifying LV systolic function. The skills required to perform limited ultrasound imaging of the left ventricle can be easily acquired and applied by noncardiologists after focused training in cardiac image acquisition and interpretation.
Interpretation of Left Ventricular Systolic Function
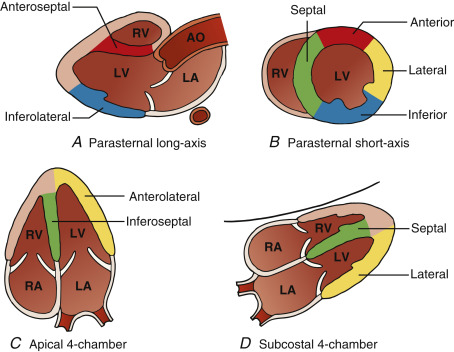
Under normal conditions, the left ventricle is the largest and most muscular chamber of the heart and can be readily identified from a variety of vantage points using transthoracic cardiac ultrasound. Common views include the parasternal long-axis, parasternal short-axis, apical 4-chamber , and subcostal 4-chamber views (see Chapter 13, Cardiac Ultrasound Technique ).
Traditional quantitative methods of determining LV function, including Simpson’s biplane method or fractional area of change, are not necessary in point-of-care cardiac ultrasound. These methods require additional training and time-consuming measurements that are prone to error and do not necessarily lead to higher accuracy. Thus, a qualitative approach to determining LV systolic function at the point of care has been embraced.
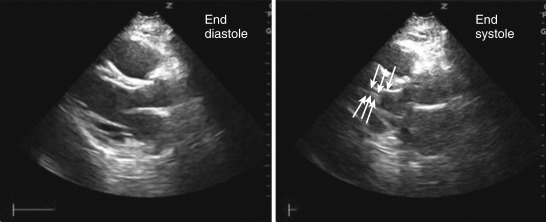
Numerous studies have demonstrated the feasibility and accuracy of point-of-care cardiac ultrasound applied in a qualitative fashion to guide management of acutely ill patients. In many of these studies, a qualitative, visually estimated left ventricular ejection fraction (LVEF) was comparable to a quantitative, calculated LVEF using comprehensive echocardiography as the gold standard. When visually estimating LV systolic function, attention is paid to all LV segments with particular focus on three characteristics ( Figure 14.1 ):
- 1.
Endocardial excursion . Does the endocardium move symmetrically toward the center of the LV chamber during systole?
- 2.
Myocardial thickening . Does the myocardium increase in thickness by approximately 40% in all LV segments during systole?
- 3.
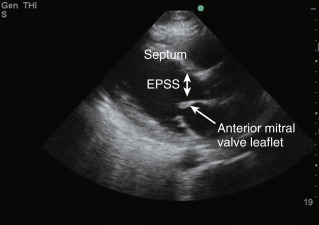
Septal motion of the anterior leaflet tip of the mitral valve (E-point septal separation). Does the anterior leaflet tip of the mitral valve come within 1 cm of the septum, which corresponds with an ejection fraction >40%?
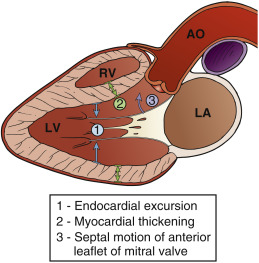
This approach easily permits broad classification of LV systolic function into four discrete categories: (1) hyperdynamic LV function, (2) normal LV function, (3) reduced LV function, and (4) severely reduced LV function. With the focus on broad gradations of LV systolic function, this qualitative schema has benefits of being intuitive to use and clinically relevant to integrate into care of patients with acute cardiac or respiratory failure.
Normal LV Systolic Function
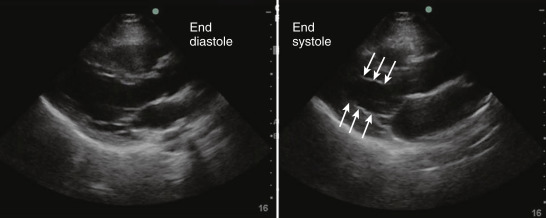
In patients with normal LV systolic function, the myocardium can be seen thickening in all segments with the endocardium moving toward the center of the LV chamber in systole. In views where the mitral valve is seen, the leaflets can be seen opening freely and approaching walls of the LV ( Figure 14.2 ). It is important to remember that the LV empties incompletely under normal conditions. The diameter of the mid-LV chamber measured at the endocardial borders decreases by approximately 30–40% during systole, leaving on average between 30% and 50% of blood volume in the LV at end-systole ( Figure 14.3 and ![]() ).
).
Hyperdynamic Left Ventricle
Identifying a hyperdynamic LV can be useful during assessment of acute, unexplained hypotension or dyspnea and can represent hypovolemia or peripheral vasodilation (e.g., septic illness). In such settings, endocardial excursion and thickening of the LV is increased, leading to near or actual end-systolic obliteration of the LV cavity ( Figure 14.4 and ![]() ). Although a hyperdynamic LV frequently suggests hypovolemia and/or vasodilation, other etiologies that can severely decrease preload or afterload should be considered, many of which will have accompanying abnormal findings easily gleaned from a focused point-of-care exam. Examples include massive pulmonary embolism, severe mitral regurgitation, or cardiac tamponade. Furthermore, high output failure due to various etiologies such as thyrotoxicosis, anemia, or infection can also be considered.
). Although a hyperdynamic LV frequently suggests hypovolemia and/or vasodilation, other etiologies that can severely decrease preload or afterload should be considered, many of which will have accompanying abnormal findings easily gleaned from a focused point-of-care exam. Examples include massive pulmonary embolism, severe mitral regurgitation, or cardiac tamponade. Furthermore, high output failure due to various etiologies such as thyrotoxicosis, anemia, or infection can also be considered.
Reduced and Severely Reduced LV Function
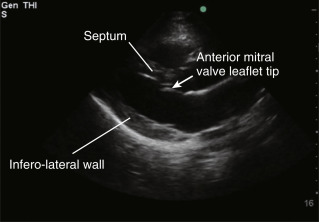
Reduced LV systolic function exhibits less myocardial thickening and endocardial excursion compared to normal. One can appreciate that the mitral valve opening is diminished and anterior leaflet tip does not approximate the septal wall ( Figure 14.5 and ![]() ). When the LV systolic function becomes severely reduced, very limited movement of the endocardium and severely diminished thickening of the myocardium are appreciated. The mitral valve opens minimally due to a very limited inward flow from the left atrium and tethering of the mitral valve by the dilated LV chamber.
). When the LV systolic function becomes severely reduced, very limited movement of the endocardium and severely diminished thickening of the myocardium are appreciated. The mitral valve opens minimally due to a very limited inward flow from the left atrium and tethering of the mitral valve by the dilated LV chamber.
As introduced above, grading LV systolic function is common in point-of-care ultrasound and focuses on a qualitative approach with discrete grades of LV function, rather than a quantitative approach with a continuous scale of LVEF. For a dysfunctional LV, decreased function is typically described as either reduced or severely reduced and can be derived from assessing three important parameters: (1) endocardial excursion, (2) myocardial thickening, and (3) mitral valve excursion.
Diminished endocardial excursion and myocardial thickening are somewhat intuitive to interpret as representing reduced LV systolic function, but mitral valve excursion in the assessment of LV function, also known as E-point septal separation in classic echocardiography vocabulary, bears some explanation. Conceptually, as the diseased LV dilates the mitral valve leaflets become tethered by the fixed length of their taught chordae tendineae. Such tethering at end-systole coupled with a low stroke volume results in the early diastolic sign of limited opening of the anterior leaflet tip of the mitral valve. This is best appreciated from the parasternal long-axis view (see Figure 14.5 and ![]() ). A qualitative estimate of >1 cm distance from the anterior mitral valve leaflet tip to the septal wall at full opening can diagnose reduced LV systolic function with an EF <40% with a sensitivity, specificity, and accuracy of 69%, 91%, and 89%, respectively. This type of assessment has been shown to be easy to implement at the bedside after brief training. It is important to remember that detection of LV systolic dysfunction by point-of-care ultrasound requires thoughtful integration into clinical management, as its impact and relevance to any given patient and/or disease state vary by individual.
). A qualitative estimate of >1 cm distance from the anterior mitral valve leaflet tip to the septal wall at full opening can diagnose reduced LV systolic function with an EF <40% with a sensitivity, specificity, and accuracy of 69%, 91%, and 89%, respectively. This type of assessment has been shown to be easy to implement at the bedside after brief training. It is important to remember that detection of LV systolic dysfunction by point-of-care ultrasound requires thoughtful integration into clinical management, as its impact and relevance to any given patient and/or disease state vary by individual.
Assessment of LV Function from Common Views
Parasternal Long-Axis View
Cardiac ultrasound imaging traditionally starts from the parasternal window. The parasternal long-axis (PLAX) view visualizes the left ventricle through its anteroseptal and inferolateral walls, with the apex commonly out of view ( Figure 14.6 ). The parasternal long-axis view is easily learned, and this single view may be considered part of a screening examination in certain circumstances. Being perpendicular to the endocardium, this view lends itself well to assessing myocardial thickening and endocardial excursion of the LV walls ( ![]() ), as well as excursion of the anterior leaflet of the mitral valve. The anterior leaflet tip should nearly contact the septum in diastole when LV systolic function is normal and in absence of structural valve disease (see Figure 14.2 ). When LV systolic function is reduced, the distance between the septum and anterior leaflet tip of the mitral valve increases as the LV dilates and diastolic blood flow is diminished ( Figure 14.7 ) .
), as well as excursion of the anterior leaflet of the mitral valve. The anterior leaflet tip should nearly contact the septum in diastole when LV systolic function is normal and in absence of structural valve disease (see Figure 14.2 ). When LV systolic function is reduced, the distance between the septum and anterior leaflet tip of the mitral valve increases as the LV dilates and diastolic blood flow is diminished ( Figure 14.7 ) .