Clinical Presentation
The patient is a 45-year-old female who presented in the emergency department with nausea, vomiting, severe headache, dizziness, neck pain and stiffness, severe low back pain, and lower extremity weakness. The patient was diagnosed 9 months previously with right upper lobe small cell lung carcinoma, stage IIIB, which has been treated with chemotherapy.
Imaging Presentation
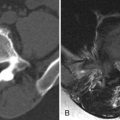
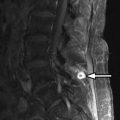
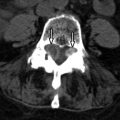
Magnetic resonance (MR) imaging of the brain and entire spinal axis was obtained. The patient has leptomeningeal contrast enhancement on the surfaces of the temporal lobes posteriorly, along the pial surfaces of the cerebellar hemispheres, along the margins of the brainstem and the cisternal segment of cranial nerve V bilaterally, and involvement of the cisternal and intracanalicular portions of cranial nerve VIII bilaterally. Diffuse leptomeningeal enhancement of the entire spinal cord and cauda equina was also apparent ( Figs. 42-1 to 42-3 ) . MR imaging findings are consistent with intracranial and spinal leptomeningeal carcinomatosis.



Discussion
Leptomeningeal metastases, also known as leptomeningeal carcinomatosis or carcinomatous meningitis , is a neoplastic condition, whereby tumor disseminates throughout the central nervous system. In the spinal canal, the tumor deposits along the surface of the spinal cord attaching to the leptomeninges. The leptomeninges anatomically includes the arachnoid and pia mater. This may occur due to tumor originating outside or inside the central nervous system (CNS).
Tumors that arise outside the CNS most commonly cause leptomeningeal metastases, and these are most commonly from primary neoplasms of the lung and breast ( Figs. 42-1 to 42-5 ), but also may occur secondary to extra-CNS melanoma, lymphoma, and leukemia. Leptomeningeal spread of tumor rarely occurs with tumors of the gastrointestinal (GI) tract, genitourinary (GU) tract, prostate cancer, mesothelioma, and myeloma. Leptomeningeal involvement by melanoma is most often from metastatic melanoma, but rarely primary leptomeningeal melanoma can occur.


In patients with extra-CNS lymphoma, leptomeningeal spread rarely occurs in patients with Hodgkin’s disease and commonly occurs in patients with AIDS-related non-Hodgkin’s lymphoma, immunoblastic lymphoma, and Burkitt’s lymphoma. In patients with myeloid malignancies, the presence of specific cytogenetic abnormalities are strongly associated with the development of leptomeningeal tumor, including translocation of chromosome 8-21 , translocation of chromosome 9-11 , deletion of chromosome 11q23 , and inversion or deletion of chromosome 16 .
Leptomeningeal spread of tumor may occur secondary to tumors originating inside the CNS, although this occurs in less than 2% of patients with primary CNS tumors overall. Primitive neuroectodermal tumors (PNET, such as medulloblastoma), primary CNS lymphoma, and glioneuronal tumors have a much higher incidence of leptomeningeal spread.
Other intracranial tumors can seed the leptomeninges producing so called drop metastases , tumors that deposit along the cord surface or in the cauda equina. Drop metastases most commonly occur with intracranial ependymomas and less commonly astrocytomas. Intradural ependymomas arising in the lumbosacral spinal canal may also cause leptomeningeal dissemination superiorly to involve the thoracic, cervical, or intracranial leptomeninges. Intracranial germ cell tumors, such as pineal germinomas, are also known to spread along cerebrospinal fluid (CSF) pathways and may involve the intracranial or spinal leptomeninges ( Figs. 42-6 and 42-7 ) .


Glioblastoma multiforme and rarely oligodendroglioma may spread along the leptomeninges. Hemangioblastomotosis, a histologically benign yet highly aggressive and devastating condition, has the same imaging appearance as leptomeningeal carcinomatosis. The clear cell subtype of meningioma has an aggressive nature and has a propensity to spread along the leptomeninges.
Leptomeningeal tumors in general carry a dire prognosis, usually leading to the demise of the patient within weeks to months. Untreated patients with leptomeningeal cancer usually die within a month. The median survival is only 4 to 5 months with treatment.
Hematogenous spread via arachnoidal vessels is believed to be the most common mechanism of spread to the leptomeninges. Direct extension may also occur from tumors located along the ependymal or meningeal surfaces. Another proposed mechanism of leptomeningeal dissemination is iatrogenic spread at the time of surgical removal of a parenchymal brain tumor, which is believed to occur more commonly after resection of a brain metastasis, especially when the metastasis is located in the posterior fossa.
There is almost always a history of known malignant neoplasm in patients with leptomeningeal metastasis. Patients with this condition typically present with severe back pain and weakness. They may have polyradicular symptoms and bladder or bowel dysfunction. Nuchal rigidity may exist, similar to patients with meningitis. Absent deep tendon reflexes and sensory loss may be present.
A lumbar puncture is usually performed in these patients to obtain CSF for chemical analysis, cell count, and cytology and to aid in excluding meningitis, which may have a similar clinical presentation. Ideally, the lumbar puncture should be performed after brain computed tomography (CT) or magnetic resonance (MR) imaging to exclude a space-occupying intracranial mass. In leptomeningeal carcinomatosis, CSF protein is usually elevated, CSF glucose may be low, lymphocytic pleocytosis may be present, and the opening pressure is often elevated. The absence of positive cytology does not exclude leptomeningeal metastasis. Malignant cells are usually detected in the CSF, but negative CSF cytology does not exclude the presence of leptomeningeal metastasis, because cytology may be negative in 10% to 15% of patients even after repeated lumbar punctures. In a patient with known malignancy and in the appropriate clinical setting with the characteristic MR imaging appearance of leptomeningeal disease, positive CSF cytology is not required to make the diagnosis.
Imaging Features
If leptomeningeal carcinomatosis is suspected, contrast-enhanced MR imaging of the entire spinal axis and brain should be obtained. Contrast-enhanced MR imaging is far more sensitive than contrast-enhanced CT or CT myelography. Leptomeningeal spread of tumor may manifest as a solitary nodule or a mass lesion along the surface of the spinal cord, cauda equina, or in the caudal aspect of the thecal sac ( Fig. 42-8 ) . More commonly, multiple small nodular tumors arise along the cord surface or cauda equina, which are visible on post-myelogram CT images, but better demonstrated on contrast-enhanced MR images (see Figs. 42-1 to 42-5 ). Diffuse leptomeningeal tumor often manifests as a fine multinodular pattern or uniform sheet-like pattern of tumor enveloping the spinal cord and nerve rootlets of the cauda equina, but this may not easily be seen on myelographic or post-myelogram CT images. Larger nodular tumor deposits may be visible as filling defects within the intrathecal contrast column on the cord surface on myelographic radiographs or on post-myelogram CT images.