5
Liver
Pyogenic Abscess
 Spread via:
Spread via:
• Biliary system (obstruction)
 Most common
Most common
 For example: cholangiocarcinoma, CBD stone
For example: cholangiocarcinoma, CBD stone
• Hematogenous spread
 For example: appendicitis, diverticulitis
For example: appendicitis, diverticulitis
 Single abscess or multiple abscesses
Single abscess or multiple abscesses
 More common in the right hepatic lobe
More common in the right hepatic lobe
 Bacteria
Bacteria
• Monomicrobial 40%, polymicrobial 40%, culture negative 20%
• Gram-negative organisms most common
• Escherichia coli found in two-thirds of abscesses
• Opportunistic organisms in AIDS patients
 Fungal and mycobacterial
Fungal and mycobacterial
• Blood cultures positive, ∼50% of cases
 Presenting signs and symptoms
Presenting signs and symptoms
• Fever (most common), right upper quadrant abdominal pain/tenderness, jaundice
 Treatment
Treatment
• Antibiotics and drainage
• Manage etiology of the pyogenic abscess
Amebic Abscess
 Caused by Entamoeba histolytica
Caused by Entamoeba histolytica
 Most common abscess worldwide—infects up to 10% of worldwide population
Most common abscess worldwide—infects up to 10% of worldwide population
 Amebic cysts are ingested, passing through stomach and small bowel unharmed → trophozoite in colon → spreads into liver via portal venous system from colon
Amebic cysts are ingested, passing through stomach and small bowel unharmed → trophozoite in colon → spreads into liver via portal venous system from colon
 Presenting signs and symptoms
Presenting signs and symptoms
• History of recent travel to endemic areas
• Right upper quadrant pain, fever, jaundice, diarrhea
• Labs
 Serologic testing
Serologic testing
 Leukocytosis
Leukocytosis
 Normal bilirubin
Normal bilirubin
 Treatment
Treatment
• Metronidazole
RADIOLOGY
General Liver Abscess (Fig. 5.1)
 Multilocular, rim enhancing mass with focal areas of fluid attenuation representing blood or pus
Multilocular, rim enhancing mass with focal areas of fluid attenuation representing blood or pus
FIGURE 5.1 A,B
A. Heart
B. Vertebra
C. Kidney
D. Spleen
E. Descending aorta
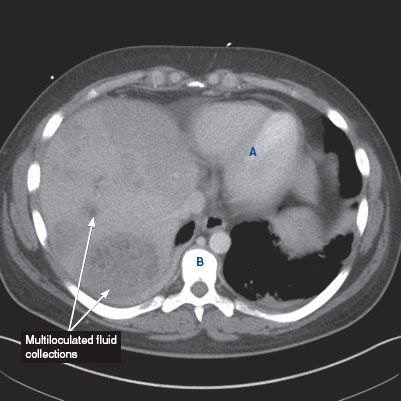
FIGURE 5.1 A
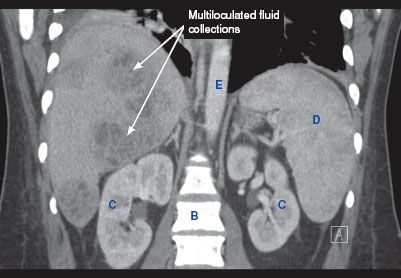
FIGURE 5.1 B
Pyogenic Abscess
 Chest x-ray
Chest x-ray
• Nonspecific findings—elevated right hemidiaphragm, right-sided pleural effusion, and atelectasis can be seen
 Ultrasound
Ultrasound
• Multiloculated fluid collection within the liver, sometimes with posterior acoustic enhancement
 CT findings
CT findings
• Multilocular fluid collection ± air–fluid levels with areas of peripheral enhancement
Amebic Abscess
 Ultrasound
Ultrasound
• Typically, a round hypoechoic, homogeneous lesion with posterior acoustic enhancement
 CT findings
CT findings
• Round, rim-enhancing hypodense lesions with a peripheral zone of edema
• May contain central septations
Hemangioma
 Most common benign tumor of the liver
Most common benign tumor of the liver
 More common in females (3:1)
More common in females (3:1)
 If greater than 5 cm then considered a giant hemangioma
If greater than 5 cm then considered a giant hemangioma
 Mostly asymptomatic. Normal LFTs and tumor markers
Mostly asymptomatic. Normal LFTs and tumor markers
 If symptomatic: Kasabach–Merritt syndrome (presents with bruising, purpura, thrombocytopenia with consumptive coagulopathy, microangiopathic hemolytic anemia)
If symptomatic: Kasabach–Merritt syndrome (presents with bruising, purpura, thrombocytopenia with consumptive coagulopathy, microangiopathic hemolytic anemia)
 Treatment
Treatment
• Surgical resection if ruptured, significant change in size, development of Kasabach–Merritt syndrome
RADIOLOGY
 CT findings (Fig. 5.2)
CT findings (Fig. 5.2)
• Relatively hypodense and well-defined lesion when compared to surrounding liver in precontrast phase
• Early peripheral nodular enhancement, with enhancement equivalent to blood pool
• Centripetal contrast enhancement on more delayed images
 MRI findings
MRI findings
• T1-weighted images may show low signal intensity
• T2-weighted images show high signal intensity
• Peripheral enhancement with equivalent signal intensity to aorta on arterial phase, with centripetal enhancement on more delayed phases
FIGURE 5.2 A,B
A. Stomach
B. Small bowel loops
C. Vertebra
D. Kidney
E. Spleen

FIGURE 5.2 A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree