, Leonid Tiutin2 and Thomas Schwarz3
(1)
Russian Research Center for Radiology and Surgery, St. Petersburg, Russia
(2)
Department of Radiology and Nuclear Medicine, Russian Research Center for Radiology, St. Petersburg, Russia
(3)
Department of Nuclear Medicine Division of Radiology, Medical University Graz, Graz, Austria
Abstract
The liver is the biggest parenchymatous organ, situated in the superior segment of the abdominal cavity under the diaphragm, mainly to the right. The liver takes an active part in all kinds of metabolism, digestion and blood circulation processes as well as in the fermentative, excretory and detoxifi cation functions of the organism, as well as in many other functions. Functionally the structural unit of the liver is a lobule consisting of hepatocytes surrounding the central vein. Between particles of lobules there lie bile ducts which interfl ow into interlobular bile ducts beyond the lobules. The latter, when joined together, form the right and left hepatic ducts, which interfl ow beyond the liver into a common hepatic duct opening to the duodenum.
The liver is the biggest parenchymatous organ, situated in the superior segment of the abdominal cavity under the diaphragm, mainly to the right. The liver takes an active part in all kinds of metabolism, digestion and blood circulation processes as well as in the fermentative, excretory and detoxification functions of the organism, as well as in many other functions. Functionally the structural unit of the liver is a lobule consisting of hepatocytes surrounding the central vein. Between particles of lobules there lie bile ducts which interflow into interlobular bile ducts beyond the lobules. The latter, when joined together, form the right and left hepatic ducts, which interflow beyond the liver into a common hepatic duct opening to the duodenum.
The blood supply of the liver occurs through the portal vein and hepatic artery; 70–80% of blood comes through the former and 20–30% through the latter. Blood outflow from the liver takes place through hepatic veins flowing into the inferior vena cava.
The liver consists of the right (and bigger) and left lobe, each of them being divided into four segments. This division is due to the portal vein branching into two big branches (for the right and left hepatic lobes); from each of them four second-order veins depart for each segment. The complexity of the anatomic structure of the liver and the diversity of its functions account for the difficulties in the diagnosis of pathological processes of the liver, especially tumor lesions.
9.1 Methods of Diagnosis
In spite of the introduction of high-technology methods of diagnosis (US, MDCT, MRI), it is only in 5–15% of cases that radical removal of the hepatic tumor is possible by the time of its detection. Up to 90% of liver cancer patients do not receive radical surgical treatment because of late diagnosis. This situation is no doubt associated with matters of general organization of oncological aid. However, there are still grave problems also in the diagnostic process. As is known, screening of liver cancer is imperfect. Usually it includes analysis of clinical data, determining the content of alpha-fetoprotein in blood and US (Sakata et al. 2008). Experience shows that this information in many cases is insufficient since clinical data have a non-specific character and are not early, and the contents of alpha-fetoprotein (AFP) in blood virtually does not increase in some malignant tumors of the liver (Kehagias et al. 2000; Sakata et al. 2008).
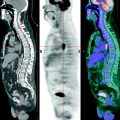
US is an efficient method of diagnosis of liver cancer. However, results of examination are to a great extent determined by the operator’s individual capacities and by the state of the apparatus. The last decade has been marked by the introduction of MDCT and MRI into clinical practice. Each of these methods develops intensively on account of improving hardware and software. Today, contrast-enhanced MDCT and CT arterioportography are used for the diagnosis of liver tumors. Besides standard MRI, dynamic contrast-enhanced MRI (DCMRI), MRI cholangiopancreatography, MRI venoportography, MR spectroscopy, etc. are also implemented. These methods have a high resolving capacity. As a rule they permit the detection of even slight structural changes in the liver. However, experience shows that in a number of situations diagnosis of liver cancer with the help of MDCT and MRI involves difficulties, especially when a tumor lesion accompanies cirrhosis. In such cases it is virtually impossible to distinguish a small tumor from nodes of hyperplasia. It should be noted that the use of contrast-enhanced CT and CT arterioportography is accompanied by a significant number of false-positive conclusions conditioned by changes in liver structure in cases of perfusion disturbances and fatty degeneration. In such cases, decisive information for differential diagnosis can be obtained by means of positron emission tomography (PET).
Liver tumors originate from hepatocytes, epithelium of bile ducts and mesenchymal tissue. The widest-spread histological classifications of malignant and benign liver tumors are shown in Tables 9.1 and 9.2 (Podymova 1998).
Table 9.1
WHO histological classification of tumors of the liver and intrahepatic bile ducts
Histological group of tumors | Histological type of tumors |
|---|---|
Epithelial tumors | Malignant |
Hepatocellular carcinoma (liver cell carcinoma) | |
Intrahepatic cholangiocarcinoma (peripheral bile duct carcinoma) | |
Bile duct cystadenocarcinoma | |
Combined hepatocellular and cholangiocarcinoma | |
Hepatoblastoma | |
Undifferentiated carcinoma | |
Benign | |
Hepatocellular adenoma (liver cell adenoma) | |
Focal nodular hyperplasia | |
Intrahepatic bile duct adenoma | |
Intrahepatic bile duct cystadenoma | |
Biliary papillomatosis | |
Non-epithelial tumors | Malignant |
Epithelioid hemangioendothelioma | |
Angiosarcoma | |
Embryonal sarcoma (undifferentiated sarcoma) | |
Rhabdomyosarcoma | |
Benign | |
Angiomyolipoma | |
Lymphangioma and lymphangiomatosis | |
Hemangioma | |
Infantile hemangioendothelioma | |
Miscellaneous tumors | Solitary fibrous tumor |
Teratoma | |
Yolk sac tumor (endodermal sinus tumor) | |
Carcinosarcoma | |
Kaposi sarcoma | |
Rhabdoid tumor | |
Others | |
Hemopoietic and lymphoid tumors | |
Secondary tumors | |
Epithelial abnormalities | Liver cell dysplasia (liver cell change) |
Large cell type (large cell change) | |
Small cell type (small cell change) | |
Dysplastic nodules (adenomatous hyperplasia) | |
Low-grade | |
High-grade (atypical adenomatous hyperplasia) | |
Bile duct abnormalities | |
Hyperplasia (bile duct epithelium and peribiliary glands) | |
Dysplasia (bile duct epithelium and peribiliary glands) | |
Intraepithelial carcinoma (carcinoma in situ) | |
Miscellaneous lesions | Mesenchymal hamartoma |
Nodular transformation (nodular regenerative hyperplasia) | |
Inflammatory pseudotumor |
Table 9.2
Classification of benign liver tumors
Histological group of tumors | Histological type of tumors |
|---|---|
Benign tumors | |
(a) Tumors originating from the stromal and vascular elements | Hemangioma (cavernoma and true gemanioma), lymphangioma, fibroma, lipoma |
(b) Tumors originating from epithelioid tissue | Adenoma |
Non-parasitic cysts | Retention cystadenoma, dermoid cysts |
Pseudocyst formations | Inflammatory and posttraumatic mesenchymal hamartoma, biliary hamartoma, congenital biliary cysts, focal nodular hyperplasia, compensatory lobar hyperplasia, etc. |
Tumor-like formations |
9.1.1 Epidemiology and Clinical Picture of Liver Tumors
Malignant Tumors
In recent decades the incidence of primary liver cancer has significantly increased. According to Weiss (1978), 20 years ago the frequency of primary liver cancer constituted 0–8% of all the pathomorphological studies and 3% of all the malignant tumors. Presently it constitutes 2–3% and 11% respectively (Podymova 1998). The mean primary liver cancer frequency in Russia is currently 6.2 per 100,000 of the population. There are regions where the values are much higher: in the basins of the Irtysh and Ob they constitute 22.5–15.5 per 100,000, cholangiocellular cancer being more often observed there. The development of cholangiocarcinoma is stimulated by parasitic diseases and helminthiases (amebiasis, schistosomiasis, opisthorchiasis and others). The risk of the disease in persons suffering from ulcerative colitis is higher by 10% than in the general population. Cirrhoses do not predispose to the development of cholangiocarcinoma. However, secondary biliary cirrhosis may develop due to tumor obstruction of bile ducts. On the whole it is hepatocellular cancer (HCC) that prevails among primary malignant liver tumors (80% of all primary liver cancers). In 60–80% of patients the development of hepatocellular cancer is associated with persistence of the viruses of hepatitis A and B. In 80–90% of these patients tumors accompany cirrhosis. Men develop the disease four- to ten-times more frequently than women. Among predisposing factors of hepatocellular cancer there are uncontrolled consumption of alcohol and other regular intoxications leading to cirrhosis.
Metastatic lesion of the liver is observed 20-times more frequently than primary liver tumors. According to different authors, from 77% to 90% of liver metastases are multifocal. Isolated lesion of one of the lobes of the liver (more frequently the right one) is observed in 10–30% of cases. Most often it is tumors of the large intestine (50–75%), pancreas (45–70%), mammary gland (10–60%), cholecyst and extrahepatic bile ducts (50–60%), stomach (20–50%) and lungs (10–40%) that metastasize to the liver. Some rarer localizations of primary tumors metastasizing to the liver are the esophagus, ovary, skin melanoma, prostate and kidneys (Prokop and Galansky 2003).
The predisposing factors of metastatic lesion of the liver are its double blood supply, a developed net of vessels of the microcircular channel, fenestrated basal membrane of sinusoids favoring the penetration of tumor cells and stimulation of tumor growth by local humoral factors.
Benign Tumors
The most frequent benign liver tumor is hemangioma. According to data obtained by autopsies, the frequency of this tumor ranges from 1% to 7%. Clinical examinations show that it is observed in 2–4% of adults. The main cause of development of liver hemangioma is considered to be associated with taking oral hormonal contraceptives. On the other hand, the dysembryoplastic theory seems to be fairly well-grounded, according to which liver hemangioma occurs in consequence of abnormal development of vessels in the phase of dysembryogenesis (Granov and Polysalov 1999). The second most frequent benign liver tumor is focal nodular hyperplasia. It is observed in patients aged 20–50 and is four- to ten-times more frequent in women. Focal nodular hyperplasia is often detected accidentally during routine diagnostic examinations. It has been established that occurrence of this disease does not depend on taking oral contraceptives.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree