Key Points
- •
Providers can accurately detect lower extremity deep venous thrombosis with bedside ultrasound after limited training.
- •
Compression ultrasound exams are as accurate as traditional duplex and triplex vascular ultrasound exams.
- •
Compression ultrasound exam at only two sites, the common femoral vein and popliteal vein, permits rapid and accurate assessment of deep venous thrombosis.
Background
Venous thromboembolic disease (VTE) is a common cause of morbidity and mortality in hospitalized patients and is especially prevalent in critically ill patients. Bedside ultrasound is readily available as a diagnostic tool for VTE. Both emergency medicine and critical care medicine literature have demonstrated that after brief, focused training, physicians and other healthcare providers can perform compression ultrasonography rapidly with high diagnostic accuracy for lower extremity deep venous thrombosis (DVT).
Traditional vascular studies, the “duplex” and “triplex” exams, use a combination of two-dimensional (2-D) imaging with compression along with the use of color and/or spectral Doppler. More recent studies have demonstrated that 2-D compression ultrasound exams alone yield accuracy similar to that of traditional duplex or triplex vascular studies. Furthermore, reporting of duplex or triplex exams is often delayed due to limitations in the availability of radiology services. Resultant delays in obtaining such test results can compromise the care of acutely ill patients. Thus the importance in avoiding such delays along with the minimal training needed to learn how to perform the exam make point-of-care lower extremity compression ultrasonography an essential skill for providers.
This chapter focuses solely on ultrasonography to detect proximal lower extremity DVT. Distal lower extremity DVTs below the knee are not discussed due to both the low embolic potential of untreated calf DVTs, as well as the lower accuracy of compression ultrasound to detect DVTs below the knee.
Anatomy
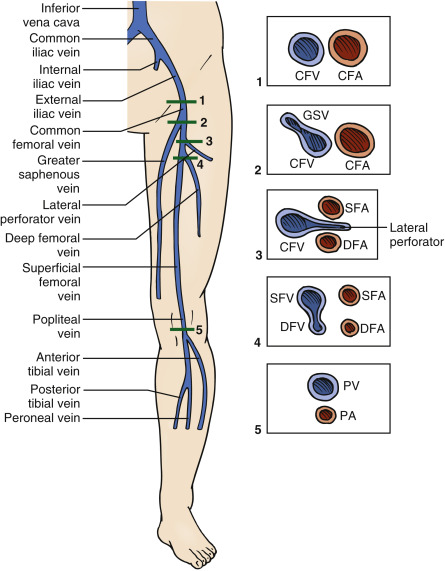
The proximal lower extremity deep venous system consists of the external iliac, common femoral, deep femoral, and popliteal veins ( Figure 26.1 ). Deep veins are accompanied by an adjacent artery. The external iliac vessels are named common femoral vessels distal to the inguinal ligament. Arteries are typically lateral to veins in the thigh. The greater saphenous vein (GSV) is the first venous branch of the common femoral vein (CFV) located anteromedially in the upper thigh. Next, the adjacent common femoral artery (CFA) divides into a deep and superficial femoral artery. A lateral perforator vein is usually seen just distal to the division of the CFA. Distal to the lateral perforator vein, the CFV divides into a deep femoral vein (DFV) posteriorly and superficial femoral vein (SFV) anteriorly. The SFV is actually a deep vein and prone to DVT formation. Current guidelines advocate removing “superficial” from the name and referring to it simply as the femoral vein . The SFV is visualized with ultrasound until it dives deep into the adductor canal (Hunter’s canal) in the distal thigh. In the popliteal fossa, the popliteal vein (PV) overlies the artery until the vein trifurcates in the distal fossa into the anterior and posterior tibial and peroneal veins.
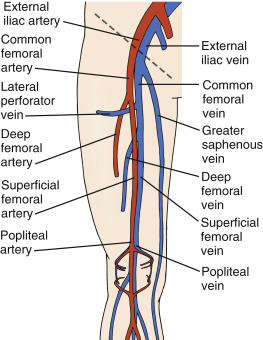
Image Acquisition
A high-frequency (5–12 MHz) linear transducer is best suited for the evaluation of lower extremity vasculature because it provides high resolution and sufficient penetration. Vessels typically appear as well-defined, circular, anechoic structures that are contiguous when tracked proximally and distally. A key step in compression ultrasound studies is differentiating veins from arteries. Even though no single feature is entirely specific, arteries are generally rounder, thicker walled, pulsatile, and smaller than accompanying veins. Most important, veins are normally fully compressible under light pressure, whereas arteries require substantial pressure to compress. Although color Doppler is not used to identify thrombus, it may help differentiate arteries from veins when the above features are equivocal, when vessels are deeper in the leg, or in obese and edematous patients.
A compression ultrasound exam is performed with patients in a supine position with the leg externally rotated and knee flexed. Ideally, the ultrasound machine should be placed ipsilaterally, distal to the site of examination with the screen directly facing the provider. The transducer is placed in a transverse orientation at the most proximal point to the inguinal ligament where the external iliac vessels can be identified, although vessels above the inguinal crease can sometimes be obscured by bowel gas.
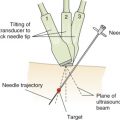
Compressions should be applied every 1–2 cm while sliding the transducer distally along the common femoral vasculature, identifying and compressing each of the main branch points ( Figure 26.2 and ![]() ). The proximal portion of the GSV should be examined as thrombus here is at high risk for extending into the CFV. Continuing distally along the CFV, a lateral perforator vein is usually seen entering the CFV prior to the division into DFV and SFV. In a “two-site” examination, compressions should be performed to a point just beyond where the CFV divides into the DFV and SFV ( Figure 26.3 ). At this point, the examiner should then examine the PV by placing the transducer within the popliteal fossa with the transducer in a transverse orientation ( Figure 26.4 ). The transducer should be held gently to avoid inadvertently collapsing the PV. If an adequate seal between the transducer and skin cannot be attained in the popliteal fossa without applying excessive pressure, consider using a narrower linear transducer. The PV is typically superficial to the artery in a central location. Visualization of associated smaller vessels indicates the transducer is positioned too distal in the popliteal fossa. Compressions are performed sequentially to the trifurcation of the PV into three calf veins.
). The proximal portion of the GSV should be examined as thrombus here is at high risk for extending into the CFV. Continuing distally along the CFV, a lateral perforator vein is usually seen entering the CFV prior to the division into DFV and SFV. In a “two-site” examination, compressions should be performed to a point just beyond where the CFV divides into the DFV and SFV ( Figure 26.3 ). At this point, the examiner should then examine the PV by placing the transducer within the popliteal fossa with the transducer in a transverse orientation ( Figure 26.4 ). The transducer should be held gently to avoid inadvertently collapsing the PV. If an adequate seal between the transducer and skin cannot be attained in the popliteal fossa without applying excessive pressure, consider using a narrower linear transducer. The PV is typically superficial to the artery in a central location. Visualization of associated smaller vessels indicates the transducer is positioned too distal in the popliteal fossa. Compressions are performed sequentially to the trifurcation of the PV into three calf veins.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree