Lymphocytic Interstitial Pneumonitis
Jud W. Gurney, MD, FACR
Key Facts
Terminology
Lymphoproliferative disorder ranging from follicular bronchiolitis to low-grade lymphoma
Diffuse disease commonly referred to as LIP
Focal disease commonly referred to as pseudolymphoma
Imaging Findings
Radiographic findings centered on lymphatic pathways in lung
Ground-glass opacities
Centrilobular nodules, poorly defined
Thin-walled cysts, perivascular, 1-30 mm in diameter, do not resolve
Centrilobular nodules may evolve into cysts
Top Differential Diagnoses
Nonspecific Interstitial Pneumonitis
Hypersensitivity Pneumonitis
Pathology
Chronic antigenic stimulus elicits lymphoproliferative response, may be
Idiopathic (rare)
Autoimmune: Sjögren syndrome
Viral infection: HIV (especially in children)
Castleman disease
Diffuse infiltration of alveolar septa by lymphocytic infiltrate
Clinical Issues
Nonspecific cough, dyspnea
Dysproteinemia (75%)
May evolve into B-cell lymphoma, especially in Sjögren (5%)
TERMINOLOGY
Abbreviations and Synonyms
Lymphocytic interstitial pneumonia (LIP), pseudolymphoma, lymphoid interstitial pneumonia, diffuse hyperplasia of bronchus-associated lymphoid tissue (BALT), mucosa-associated lymphoid tissue (MALT)
Definitions
Part of spectrum of idiopathic interstitial pneumonias
Lymphoproliferative disorder ranging from follicular bronchiolitis to low-grade lymphoma
Diffuse disease commonly referred to as LIP
Focal disease commonly referred to as nodular lymphomatoid hyperplasia (pseudolymphoma)
Nonneoplastic lymphoproliferation must be differentiated from lymphoma by immunologic stains
Monoclonal cell lines in lymphoma, polyclonal in nonneoplastic lymphoproliferative disorders
IMAGING FINDINGS
General Features
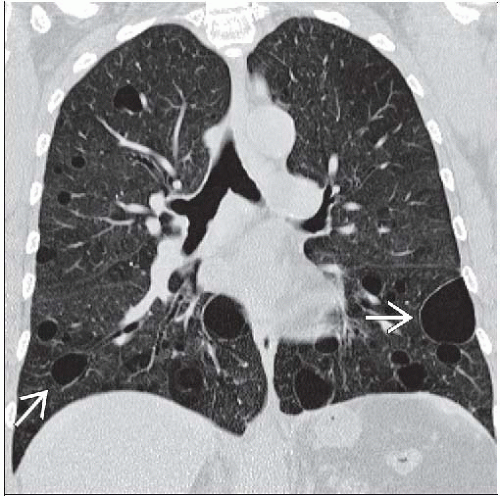
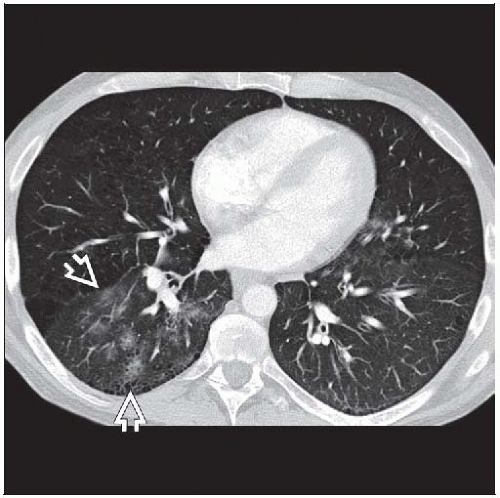
Best diagnostic clue: Thin-walled cysts and centrilobular nodules
Patient position/location: Centered on lymphatic pathways: Peribronchovascular, centrilobular, septa, and pleura
CT Findings
Radiographic findings centered on lymphatic pathways in lung
Peribronchovascular, septa, pleura
Diffuse (LIP)
Ground-glass opacities (100%)
Distribution: Bilateral (90%), diffuse (60%), peripheral distribution (10%)
Centrilobular nodules
Poorly defined, 2-4 mm in size
Thin-walled cysts
Most distinctive finding (80%)
Range 1-30 mm in diameter (average 5 mm)
Involve < 10% of total lung
May be isolated finding
Combination of ground-glass opacities, centrilobular nodules, and thin-walled cysts common
Other findings (related to lymphatic pathways)
Subpleural nodules (> 50%)
Septal thickening (80%)
Thickening of small bronchovascular bundles (tree-in-bud pattern)
Bronchiectasis (20%)
Rarely fibrosis and honeycombing
Focal (pseudolymphoma)
Air-space mass, consolidation with air-bronchograms
Nodules (> 5 mm)
Peribronchial in distribution
Up to 30 mm in size (average 10 mm)
No lobar predilection
Cavitation rare
Evolution
All findings may resolve except for cysts
Centrilobular nodules may evolve into cysts
Airspace consolidation may evolve into honeycombing
Lymph nodes may be enlarged (up to 70%), usually multiple nodal groups
More common in AIDS patients
Not large enough to see on radiography
Pleural effusions rare
Radiographic Findings
Usually nonspecific findings, better evaluated with CT
Diffuse disease (LIP)
Diffuse interstitial thickening, predominately basilar
Multiple pulmonary nodular opacities often with air-bronchograms (more common in AIDS)
Focal
Focal central airspace mass(s), segmental or lobar in size mimicking pneumonia
Over time gradually grow toward periphery of lung
May also arise in lung periphery
Unilateral or bilateral
Pleural effusions rare
Associated findings
Anterior mediastinal mass: Thymoma
Predisposing condition for hypogammaglobulinemia or myasthenia gravis, either of which may lead to LIP
Splenomegaly
DIFFERENTIAL DIAGNOSIS
Nonspecific Interstitial Pneumonitis
Cellular or fibrotic, temporally homogeneous at histology
Idiopathic or seen with collagen vascular diseases
Ground-glass opacities in bronchovascular distribution
Angioimmunoblastic Lymphadenopathy
Lymphoproliferative disorder associated with dysproteinemia and immunodeficiency
Generalized lymphadenopathy and hepatosplenomegaly
Skin rash
Pleural effusion
Lung may be normal or have focal mass-like areas of consolidation
Castleman Disease
Benign lymphoproliferative hyperplasia of lymph nodes
Hilar or mediastinal adenopathy
Hyaline vascular form: Nodes have intense contrast enhancement
Lungs less likely to be abnormal (if abnormal may be due to co-existing LIP)
Lymphomatoid Granulomatosis
Multiple pulmonary nodules (may be cavitary)
Skin rash
Central nervous system (CNS) disease
Hypersensitivity Pneumonitis
Thin-Walled Cysts
Laryngotracheal papillomatosis
Pneumatoceles
Trauma
Pneumocystis jiroveci pneumonia
Staphylococcus pneumonia
Hydrocarbon ingestion
Langerhans granulomatosis
Lymphangiomatosis
Centrilobular emphysema
Metastases
Birt-Hogg-Dubé syndrome: Multiple renal oncocytomas/cancer, skin lesions
PATHOLOGY
General Features
General path comments
BALT is subset of MALT
BALT extends from nodal clusters in airway bifurcations to lymphocyte clusters at proximity of lymphatics in terminal bronchiole
BALT extensive, positioned to handle large number of inhaled or circulating antigens
Polyclonal proliferation consistent with benign disease, monoclonal proliferation of lymphocytes consistent with lymphoma; clonal groups determined by special stains
BALToma (lymphoma) low-grade B-cell primary pulmonary lymphoma
BALT hyperplasia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree