chapter 12 Lymphoma
INTRODUCTION
In recent years, 18F-fluoro-deoxy-D-glucose positron emission tomography (FDG-PET) has been incorporated in the management of malignant lymphomas. FDG-PET provides valuable information to clinicians in disease staging, evaluation of response to chemotherapy, planning of radiotherapy, and finally, re-staging and follow-up after therapy.1–4 Therapeutic implications for patients with Hodgkin’s disease (HD) and non-Hodgkin’s lymphoma (NHL) emphasize the importance of initial accurate disease staging. Until recently, gallium scintigraphy played an important role in lymphomas in monitoring the response to treatment and clarifying the nature of residual masses detected on computed tomography (CT).5,6 Its limited resolution failed to detect smallvolume residual disease and sometimes non-specific uptake in benign lesions. In addition, it is less sensitive in intra-abdominal disease.7 For these reasons, FDG-PET has largely replaced the gallium scan in many centers.8,9 Other than being a valuable staging tool, it provides accurate prognostic information for both HD and NHL since a reduction of FDG uptake after initial chemotherapy is a highly predictive factor of favorable outcome, while residual uptake is indicative of unfavorable prognosis.10,11 PET helps to distinguish complete disease remission from partial response,12–14 which can lead to a change in management plan.
FDG-PET can be very valuable for radiotherapy purpose, and it is currently used successfully in several centers worldwide. The most important application of PET is for radiotherapy field delineation. By accurate assessment of initially involved anatomic sites and response to chemotherapy, radiation oncologists can reduce the volume of irradiation, spare the surrounding healthy tissues, and adjust the prescribed dose. FDG-PET has been reported as a useful tool for early identification of patients who may benefit from salvage therapy.14,15
Rationale for Use of PET and PET-CT for Lymphoma
The Value of PET in Determining the Indication of Radiation Therapy
The PET-CT can be particularly helpful in distinguishing between residual disease and complete response after initial chemotherapy, and can help identify the favorable group of patients with either HD or NHL who can be treated with reduced intensity chemotherapy or radiotherapy or with a single modality after achieving PET negativity. In conjunction with CT and magnetic resonance imaging (MRI) criteria, a metabolic image can add substantial validity to the interpretation of a chemotherapy response (complete response [CR] vs. partial response [PR]). For instance, functional imaging may play a more critical role in the tumor response evaluation particularly in the case of nodular sclerosing Hodgkin’s lymphoma, which is characterized by the presence of a thickened lymph node capsule and is commonly associated with extensive tumor bulk. Because of the abundance of collagen, the radiographic appearance of these lesions (particularly in the mediastinum) may only slowly return to normal, even when the patient is responding to therapy.16 Regression or resolution of metabolic tumor activity by PET serves as a surrogate for tumor response and precludes the need for invasive procedures to document the disease status.
Integration of PET-CT in the Process of Radiation Treatment for Lymphomas
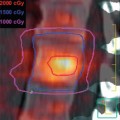
Because tumor control rates are excellent with current approaches, there is an opportunity for the reduction of treatment intensity in an attempt to minimize late effects, especially in younger patients. In the era of combined chemoradiotherapy for lymphoma, there has been a substantial paradigm shift from extended field to involved field radiotherapy, but the concept of contiguous lymphatic tumor spread in HD is still applied in designing radiotherapy fields.17 Radiation oncologists usually attempt to cover lymphatic regions rather than individual involved nodes. PET can help define the target volume and tailor radiation doses according to the disease burden. The treatment volume irradiated following the delivery of systemic therapy is often modified relative to the initially defined volume based on changes in normal tissue anatomy (defined on CT and MRI) as the primary mass shrinks following chemotherapy. The incorporation of PET imaging into radiation therapy treatment planning could allow further reduction of the treatment dose and/or volume, based on the response following systemic chemotherapy. This strategy of dose reduction was undertaken by several investigators specifically for pediatric HD.17,18
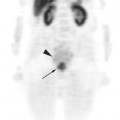
As part of radiotherapy planning, the first important goal for the radiation oncologist is to provide a careful evaluation of the patient for initially involved sites and the response to chemotherapy. This is better accomplished with collaboration from radiology colleagues. Previously, when only CT or MRI was used to assess the response to initial chemotherapy, a decrease in the size of a lymphomatous mass was considered a response to treatment. This led to the development of formal criteria based on the measurement of the cross-sectional area.19,20 Current radiotherapy design guidelines are still mainly based on size criteria as determined from CT or MRI scans, and PET serves only as a correlative tool. The evaluation of residual masses on anatomic imaging following treatment is a major challenge in a significant number of patients with lymphoma. It may take a long time before the decrease in size of the tumor mass becomes evident on anatomic imaging scans. Other processes such as fibrosis, necrosis, or inflammation may cause only a partial reduction of the mass, and this may be influenced by its location, histology, original size, and treatment.16,19,20
Fusion Technique and Target Delineation
In addition, patients may have received a series of PET scans that reflect the initial staging and the response to chemotherapy, all of which may ultimately be incorporated in radiation treatment planning. Indeed, the ideal timing of PET scans after the completion of chemotherapy has not been firmly established for patients with lymphoma. Some have advocated that scans be obtained 2 weeks after the completion of chemotherapy to avoid fluctuations in FDG metabolism.21–23 There is firm evidence that for radiotherapy planning purposes, the pre-chemotherapy PET scan is the most reliable and will help to avoid mis- or under-dosing of the areas at high risk of relapse.14 Accepting the variability in body positioning from the initial PET scan to the planning CT or PET-CT scan, it is still desirable to fuse these image sets together to incorporate all the information on disease involvement in radiotherapy planning. This step will help to most accurately delineate all target volumes and also assess disease volume reduction and resulting change in normal structure anatomy.
Co-registration, Fusion, and Target Delineation
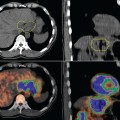
Co-registration and fusion occurs between the CT component of the PET-CT scan and the CT planning image set. Software fusion can be accomplished via a variety of methods including the placement of fiducial markers or anatomic localization of similar points. At our institution, manual co-registration is undertaken with the selection of easily identifiable anatomic landmarks. We typically choose a minimum of three non-coplanar anatomic points on both image sets, and fusion is considered acceptable when a mean error of 2 mm by root-mean-square is achieved.
Contours typically include both a CT-gross tumor volume (GTV) and a PET-GTV. Contours on the PET portion of the PET-CT automatically transfer to the planning CT. When delineating the PET tumor volume, it is important to understand the threshold intensity that was selected in interpreting PET images and determining what shows increased FDG uptake. A commonly employed mechanism is to interpret images at the 50% threshold intensity or isocontour.24,25 A potential limitation of this approach is that if a tumor shows high avidity for FDG, selection of the 50% intensity may underestimate the true tumor volume. Conversely, the true volume for lesions with low avidity may be overestimated.
Pitfalls Associated with PET-CT
Interpretation of Pre-treatment PET-CT
While PET imaging generally provides information about tumor activity that complements anatomic findings on CT and facilitates assessment of treatment response, FDG avidity related to other nonmalignant conditions may, on occasion, confound interpretation of tumor response. Multiple factors can account for changes in PET avidity within a CT-defined mass. According to the literature, one of the most frequent causes of non-tumoral FDG uptake is non-specific inflammation; therefore, active inflammation/infection, granulomas, and abscesses can be associated with increased standardized uptake value (SUV) and can be falsely interpreted as a malignant process.26,27 Also, thymic hyperplasia can cause FDG uptake, especially following chemotherapy (so-called “thymic rebound”).28 FDG uptake may also occur in up to 30% of normal thymus glands in patients younger than age 30.29 More recently, the presence of brown adipose tissue has been described as related to focal FDG accumulation, especially in the neck and upper posterior thorax and causing some difficulty in PET scan interpretation.30–32 Previous lymphangio-graphy and radiation pneumonitis are other causes responsible for false-positive FDG uptake.33,34 Other, less frequent causes of potential pitfalls due to FDG uptake in treated malignant lymphoma patients have been described as esophagitis, gastritis, and colitis.35 Moreover, the possibility of an infectious disease concomitant to malignant lymphoma, even if rarely described, should be taken into account by the clinician.36,37 There are reports on observed transient intense FDG-avidity of the skeleton and spleen in patients treated with growth-factor support following myelosuppressive therapy.38 Subsequent resolution of these findings without therapeutic intervention establishes the relationship of FDG avidity and granulocyte-colony stimulating factor (G-CSF)-induced stimulation of myelopoiesis. If folow-up imaging shows improvement or resolution without a change in antineoplastic therapy, a non-malignant source of FDG avidity is suggested.
Knowledge of these conditions and a precise interpretation of the PET scan are essential to guarantee the correct management of patients with malignant lymphoma. Accordingly, an accurate patient history and physical examination are very important in leading the nuclear medicine physician to suspect non-specific FDG focal uptake. Particular attention has to be given to the symptoms that suggest an infection. Moreover, as suggested by many authors, an appropriate learning curve in reading and interpreting PET scans is another important factor to reduce the number of false-positive results.37,39 The more widespread use of hybrid PET–CT scanners is expected to further help the nuclear medicine physician obtain a correct diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree