Lymphoma and Myeloma
S. N. Reske
Malignant Lymphoma
The use of positron emission tomography (PET) and PET combined with computed tomography (CT) in lymphoma management has shown remarkable growth in the past few years as a wide range of articles have been published showing the generally broad applicability of PET with fluorodeoxyglucose (FDG) in this group of diseases (1,2,3,4,5,6,7,8,9,10).
This chapter will summarize the current state of the art for PET and PET/CT in lymphoma, emphasizing the performance, value, and limitations of these technologies. Due to highly increased glycolysis in most malignant lymphomas, FDG is currently the preferred radiopharmaceutical for PET imaging of lymphomas. Interestingly, however, one of the earliest reports of PET imaging in lymphoma used calcium-11-methionine for assessment of viability of a residual mass in non-Hodgkin’s lymphoma (NHL) after radiation therapy (11). In a letter to Lancet in 1990, Leskinnen-Kallio et al. (11) made the farsighted statement that “PET may be a new way of detecting viable malignant tissue.” Since that time, many reports have shown the use and value of PET and more recently of PET/CT imaging of malignant lymphomas for pretherapeutic staging, therapy control, interim response assessment of various combinations of radio-, chemo-, immuno- and radioimmunotherapy (3,12,13,14), and evaluation of prognosis (10,15,16). Several excellent recent reviews covering these issues have been published (15,16,17,18,19). This chapter will briefly summarize use of FDG PET and PET/CT for (a) initial pretherapeutic staging, (b) relevance of response monitoring, (c) technical considerations, (d) treatment remission assessment, (e) evaluation after completion of chemotherapy and/or radiotherapy, and (f) early response assessment, as well as discuss some novel functional imaging approaches in malignant lymphoma.
Staging
The Ann Arbor classification can be used both for Hodgkin’s lymphoma and NHL and differentiates malignant lymphoma distribution into four categories.
Stage I: disease limited to a single lymph node or a single lymph node group;
Stage II: two or more noncontiguous nodal groups or the spleen on the same side of the diaphragma;
Stage III: two or more nodal groups or the spleen on both sides of the diaphragma;
Stage IV: disease in extranodal sides (bone marrow, liver, lung, bone, or other organs/tissues).
Extension from a nodal manifestation into extranodal tissue (S) such as the lung, pleura, pericardium, skin, and so forth may occur in stage I through III and does not increase the stage to stage IV, but is designated by the involved tissue/organ with the subscript “E.” Nodal disease greater than 10 cm in the largest diameter is defined as “bulky” and designated with a suffix “X” to the numeric stage (18).
There are several preferred sites of involvement of NHL: compared to Hodgkin’s lymphoma, Waldeyer’s ring is involved in 5% to 10% of patients with NHL and extremely rarely involved in Hodgkin’s lymphoma. Waldeyer’s ring involvement by NHL may be associated with involvement of the gastrointestinal tract/stomach or bowel. Mesenteric lymph node involvement is quite common in NHL, but only rarely seen (less than 5%) in Hodgkin’s lymphoma. Bone marrow involvement is present in 15% to 40% of patients with NHL (17).
Stage is an important component of a predictive model for untreated patients with intermediate- or high-grade NHL (9). The five important factors at presentation are age (60 years or less vs. greater than 60 years, serum low-density lipoprotein concentration (one or less times normal vs. greater than one times normal), performance status (0 or 1 vs. 2 to 4), stage (I or II vs. III or IV), and extranodal involvement (one or less site vs. more than one site).
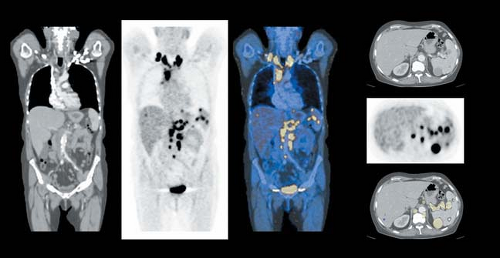
FDG PET or more recently FDG PET/CT can be used both for nodal and extranodal staging (14,20,21,22,23,24,25). Fast and convenient imaging of the whole body or, more practically, the body from the ear to the proximal thigh, within about 30 minutes in conjunction
with contrast-enhanced CT provides excellent and precise imaging of virtually all organs and tissues potentially involved by Hodgkin’s lymphoma or NHL (Fig. 8.10.1). This approach offers the advantage of both diagnostic CT with the added benefit of the functional imaging of FDG PET with high technical quality and less dependence on size-based criteria, limiting the sensitivity of nodal staging of CT. Thus, increased FDG uptake can be easily measured with FDG PET or FDG PET/CT in nodes less than 1 cm in diameter. In addition, it has been shown that focal involvement of bone marrow can be accurately detected with FDG PET or PET/CT, but is limited with CT. Virtually all nodal groups can be reasonably accurately imaged, with the FDG PET/CT approach in high- and intermediate- grade lymphoma.
with contrast-enhanced CT provides excellent and precise imaging of virtually all organs and tissues potentially involved by Hodgkin’s lymphoma or NHL (Fig. 8.10.1). This approach offers the advantage of both diagnostic CT with the added benefit of the functional imaging of FDG PET with high technical quality and less dependence on size-based criteria, limiting the sensitivity of nodal staging of CT. Thus, increased FDG uptake can be easily measured with FDG PET or FDG PET/CT in nodes less than 1 cm in diameter. In addition, it has been shown that focal involvement of bone marrow can be accurately detected with FDG PET or PET/CT, but is limited with CT. Virtually all nodal groups can be reasonably accurately imaged, with the FDG PET/CT approach in high- and intermediate- grade lymphoma.
Practically all studies comparing FDG PET to CT reported a 10% to 20% higher accuracy of FDG PET for staging of lymphoma and resulted in treatment changes of 10% to 20% (see Hicks et al. [14] for a review). Improved staging in Hodgkin’s lymphoma with FDG PET/CT compared to CT was recently demonstrated by Hutchings et al. (26). Many of the lesions detected with PET are in lymph nodes of under 1 cm in size and thus are called normal nodes on CT. Similarly, detection of disease within the spleen is markedly improved using PET versus CT methods.
Limitations of FDG PET or FDG PET/CT for staging are diffuse bone marrow involvement by NHL with less than 10% infiltration of bone marrow with NHL (23), with a reduced sensitivity of FDG PET and probably also FDG PET/CT in some indolent (low-grade) lymphomas (27). The manifestations of FDG uptake in lymphoma vary depending on the histology (28). In a recent study, the sensitivity of FDG PET was excellent (approximately 95%) in grade I to III follicular lymphoma, moderate (74%) in mantle cell lymphoma, and limited (approximately 50%) in B-cell small cell lymphocytic lymphoma (28). A study by Jerusalem et al. (27) reported that FDG PET identified 40% more abnormal lymph node sites then conventional staging in 24 patients with follicular histology, but less than 58% of abnormal nodal sites compared to CT in 11 patients with small lymphocytic lymphoma.
As suggested by studies in a small number of patients, performance of FDG PET is less accurate in patients with mucosa-associated lymphoid tissue lymphoma (29). Sensitivity is probably dependent on histology and limited in low-grade mucosa-associated lymphoid tissue lymphoma (30). With regard to a false-negative case of bronchial wall involvement by NHL reported by Bangerter et al. (31), it is clear that microscopic involvement in any tissue is beyond the detection capabilities of FDG PET or FDG PET/CT. Small tumor volume likely accounts for failure to detect small levels of bone marrow involvement with PET. Unspecific nodal or extranodal FDG uptake due to focal inflammatory disease may be a cause of false-positive results, but this rarely causes problems in the context of initial staging of malignant lymphomas.
Relevance of Response Monitoring
As recently reviewed by Mikhaeel (16), many forms of lymphoma are curable disease, but its treatment is associated with significant short- and long-term toxicity. In the treatment of curable lymphoma (Hodgkin’s) and aggressive high-grade NHL the goal of treatment is to achieve a complete response (CR), which is a prerequisite for cure. Patients who do not achieve a CR by the end of treatment are offered various salvage treatment regimens. Accurate assessment of remission after the completion of a planned course of treatment is therefore essential to improve the prognosis of patients with less than CR and to avoid unnecessary treatment-related toxicity and treatment-associated short- and long-term morbidity in those patients who achieve a complete CR.
FDG PET and PET/CT have been very successfully employed for this posttreatment remission assessment. Another comparable interesting and potentially more important form of assessment is early response assessment. The main goal of this approach is to
adjust the intensity and type of treatment to the individual patient’s prognosis. Response to treatment is probably the most important single factor determining the prognosis of the individual patient. Response adjusted treatment aims to optimize the balance between the chance of cure and potential toxicity for the individual patient. Early response assessment enables a strategy for minimizing treatment for patients with a good prognosis and intensifying treatment for patients with a poor prognosis (16).
adjust the intensity and type of treatment to the individual patient’s prognosis. Response to treatment is probably the most important single factor determining the prognosis of the individual patient. Response adjusted treatment aims to optimize the balance between the chance of cure and potential toxicity for the individual patient. Early response assessment enables a strategy for minimizing treatment for patients with a good prognosis and intensifying treatment for patients with a poor prognosis (16).
Technical Considerations
The best time for end of treatment evaluation remains unknown, but most investigators suggest waiting at least 1 month after the last day of chemotherapy and 3 months after the last dose of radiotherapy (15,16). It must be kept in mind, that fluorine-18 (18F)-FDG PET or PET/CT cannot exclude minimal residual disease, and it may be indicated to repeat [18F]-FDG PET or PET/CT during routine follow-up to overcome insecurities regarding the potential of residual tumor at the end of treatment (15). Residual lymphoma also may be missed or its extent underestimated because low-grade lymphoma is not FDG avid or has very low uptake. This is, however, relatively uncommon.
Positive findings in PET/CT do not necessarily represent residual disease. Meticulous evaluation of PET images is mandatory to avoid false-positive findings associated with muscle tension or normal intestinal structures. Brown fat can avidly incorporate FDG and is frequently seen in slim young women. Because FDG is not a tumor-specific radiotracer and acute inflammation stimulates glycolytic flux in leucocytes (32), inflammatory lesions may show intense FDG uptake. Documented causes of false-positive PET studies in the assessment of response of lymphoma are shown in Table 8.10.1.
Although not studied in detail in lymphoma, it is well known from studies in various solid tumors that diabetes mellitus and increased blood sugar concentration can reduce the sensitivity of FDG PET considerably (33,34). Therefore, it is the author’s institutional practice to examine patients only with a blood sugar concentration below 150 mg/dL and to keep patients fastened at least 5, better 8, hours before the examination. Practice varies by center, but most would not perform PET studies if the serum glucose level exceeds 200 mg/dL. Intravenous furosemide before the PET study in order to flush the renal collecting system and thus to avoid reconstruction artifacts is no longer used by most centers, since powerful iterative reconstruction algorithms and CT-based attenuation correction impressively improve the image quality of PET scans.
Assessment of Treatment Remission
The assessment of remission status commonly involves clinical examination, blood tests, CT scanning, and in some cases histopathological examination of bone marrow and other imaging modalities such as magnetic resonance tomography (16,35). Criteria for response assessment and response categories have been established for lymphoma and are commonly known as the International Workshop Classification (IWC) (35). The IWC predominantly relies on anatomical imaging modalities such as CT scanning or magnetic resonance tomography.
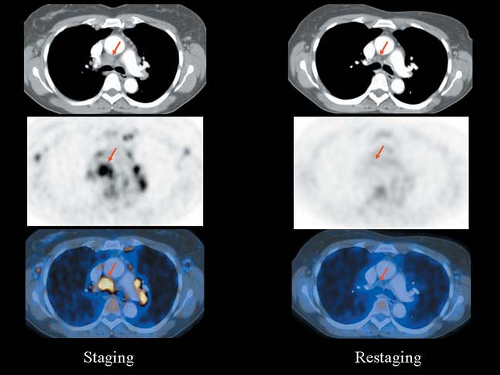
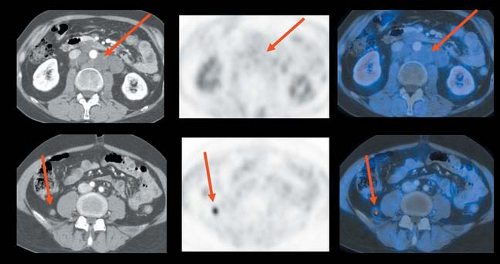
Criteria for response assessment have been recently revised and PET or PET/CT has been implemented (9). The reason for revision was that it had been long recognized that lymphoma masses, especially when bulky on presentation, may not disappear completely if the disease has been eradicated completely (Fig. 8.10.2). These “residual masses” are formed mainly from necrotic or fibrotic tissue and may continue to shrink during follow-up (16,36). Only about 20% of residual masses harbor residual viable malignant cells. Therefore, offering more treatment to all patients with residual masses would involve overtreating many patients unnecessarily (16) (Fig. 8.10.3). Follow-up of these masses to treat only the progressing ones may waste valuable time and compromise the chances of cure.
Table 8.10.1 Documented Causes of False-positive Fluorine-18-fluorodeoxyglucose PET Studies in Evaluation of Response | ||
|---|---|---|
|
The introduction of functional metabolic imaging using FDG PET or PET/CT has proven to be helpful in accurate assessment of remission posttreatment and in characterizing residual masses. The role of FDG PET in assessing residual masses has been widely accepted (9).
As recently recommended by the imaging subcommittee of the International Harmonization Project in Lymphoma, pretherapy PET is not obligatory for assessment of response after treatment of patients with Hodgkin’s lymphoma and those subtypes of NHL that normally have a high glycolytic rate and hence high FDG uptake. These include diffuse large B-cell lymphoma, follicular lymphomas, and mantle cell lymphoma (7). However, FDG PET or PET/CT is indicated in these subtypes as a baseline examination and a reference of lymphoma manifestations for follow-up (7). In contrast, FDG PET or PET/CT is mandatory in those subtypes with variable FDG uptake when FDG PET will be used during follow-up (7). These subtypes include aggressive NHL excepting diffuse large B-cell lymphoma (i.e., T-cell lymphoma) and indolent lymphoma excepting follicular lymphoma (7). In practice, many centers prefer
to have a baseline PET study so that tumor burden and starting standard uptake value (SUV) can be determined. Indeed, some investigators feel it is much better to secure a baseline PET/CT study in all patients with lymphoma if at all possible.
to have a baseline PET study so that tumor burden and starting standard uptake value (SUV) can be determined. Indeed, some investigators feel it is much better to secure a baseline PET/CT study in all patients with lymphoma if at all possible.
Diagnostic Criteria
PET after completion of chemotherapy should be performed at least 3 weeks, preferably 6 to 8 weeks, after chemotherapy or chemoimmunotherapy, and 8 to 12 weeks after irradiation or combined radio- and chemotherapy (7). Mediastinal blood pool activity is recommended as the reference background radioactivity for classification of residual masses either as positive (i.e., viable lymphoma), when their radioactivity concentration is increased over the reference background, or negative (i.e., scar tissue), when their radioactivity is less than the reference background. Visual assessment of potential lymphoma manifestations is regarded as adequate.
Mild and diffusely increased FDG uptake in residual masses 2 cm or greater in diameter with intensity less than or equal to mediastinal blood pool structures should be considered negative for lymphoma. New FDG positive lung nodules should be regarded as inflammatory when all other previously known lymphoma manifestations show complete response. Residual hepatic or splenic lesions greater than 1.5 cm on CT and FDG uptake greater than or equal to that of liver or spleen should be considered positive. Clearly increased multifocal bone marrow uptake should be interpreted as positive for lymphoma. A detailed discussion of FDG imaging criteria was recently published by Juweid et al. (7).
From the published literature, some general conclusions can be drawn (16):
FDG PET is more accurate than CT in virtually all studies (except in the relatively low FDG avidity lymphomas noted previously).
The accuracy of PET is high enough to be used as a standard measure for assessment of remission, either supplementing or in combination with PET/CT, replacing the “CT only” study in the FDG avid lymphomas.
Evaluation After Completion of Chemotherapy and/or Radiotherapy
Achieving a complete remission is a major objective in patients with Hodgkin’s lymphoma or NHL because it is usually associated with a longer progression-free survival than a partial remission (see Jerusalem et al. [15] for a review). However, in as many as 64% of all Hodgkin’s lymphoma cases and in 30% to 60% of all NHL cases, CT
or magnetic resonance tomography shows abnormalities during restaging (16). Residual masses are observed more frequently in patients with aggressive NHL and with a large tumor mass at diagnosis, as well as in patients suffering from Hodgkin’s lymphoma of the nodular sclerosis histologic subtype (15). Unfortunately, conventional anatomic imaging cannot differentiate between benign fibrous tissue and an inflammatory process or persistent malignant disease. A maximum of only 20% of residual masses at the completion of treatment are reported to be positive for lymphoma on biopsy, and they eventually relapse (35,36). If the tumor is easily accessible, such as an enlarged peripheral lymph node, the questionable lesion can be excised and histologically analyzed.
or magnetic resonance tomography shows abnormalities during restaging (16). Residual masses are observed more frequently in patients with aggressive NHL and with a large tumor mass at diagnosis, as well as in patients suffering from Hodgkin’s lymphoma of the nodular sclerosis histologic subtype (15). Unfortunately, conventional anatomic imaging cannot differentiate between benign fibrous tissue and an inflammatory process or persistent malignant disease. A maximum of only 20% of residual masses at the completion of treatment are reported to be positive for lymphoma on biopsy, and they eventually relapse (35,36). If the tumor is easily accessible, such as an enlarged peripheral lymph node, the questionable lesion can be excised and histologically analyzed.
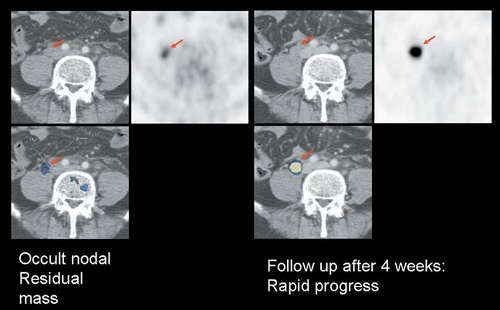 Figure 8.10.3. Fluorodeoxyglucose PET/CT of residual occult viable non-Hodgkin’s lymphoma 8 weeks after completion of chemotherapy. There is rapid progression of disease at 4-week follow-up. |
If anatomical access is difficult, noninvasive imaging with FDG PET or PET/CT is of major importance (Fig. 8.10.4). Several recent
studies demonstrate the value of FDG PET or PET/CT for end-of-treatment response assessment (15). Jerusalem et al. (15) compiled the results of 17 selective studies with a total of 752 patients. In these studies the overall accuracy of PET was 88% to 91%. PET had a better positive predictive value for NHL (100%) than for Hodgkin’s lymphoma (74%) and a better negative predictive value (for Hodgkin’s lymphoma 93%) than for NHL (83%) (Tables 8.10.2 and 8.10.3). As indicated by Mikhaeel (16), a positive PET after treatment of NHL is strongly predictive of residual disease, but less so in Hodgkin’s lymphoma. A negative PET after Hodgkin’s lymphoma treatment is predictive of freedom of residual disease, but this is slightly less in NHL. This finding possibly reflects the presence of inflammatory cellular infiltrate in Hodgkin’s lymphoma and the higher relapse rate of NHL (16).
studies demonstrate the value of FDG PET or PET/CT for end-of-treatment response assessment (15). Jerusalem et al. (15) compiled the results of 17 selective studies with a total of 752 patients. In these studies the overall accuracy of PET was 88% to 91%. PET had a better positive predictive value for NHL (100%) than for Hodgkin’s lymphoma (74%) and a better negative predictive value (for Hodgkin’s lymphoma 93%) than for NHL (83%) (Tables 8.10.2 and 8.10.3). As indicated by Mikhaeel (16), a positive PET after treatment of NHL is strongly predictive of residual disease, but less so in Hodgkin’s lymphoma. A negative PET after Hodgkin’s lymphoma treatment is predictive of freedom of residual disease, but this is slightly less in NHL. This finding possibly reflects the presence of inflammatory cellular infiltrate in Hodgkin’s lymphoma and the higher relapse rate of NHL (16).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree