CHAPTER 12 When most of us first encounter an ankle MRI image, we get out a cross-sectional atlas and start trying to determine where all the tendons, muscles, vascular structures, and so on, lie. I can assure you this will be unnecessary after reading this chapter. Although the anatomy of the foot and ankle can be complex, the significant anatomy, that is, the anatomy that must be learned because it is affected by disease, is fairly straightforward and easily learned.1 There is no need to memorize tendons, ligaments, and muscles that are only rarely seen to be abnormal; therefore this chapter dwells only on the pathologically significant areas. The Achilles tendon does not have a sheath associated with it; therefore tenosynovitis does not occur. Tendinosis and partial tears are commonly seen in the Achilles tendon. Complete disruption is commonly seen in athletes and in males around the age of 40; however, it is such an easy clinical diagnosis that MRI examination is usually not necessary. Complete tears are also commonly associated with other systemic disorders that cause tendon weakening, such as rheumatoid arthritis, collagen vascular diseases, crystal deposition diseases, and hyperparathyroidism. MRI scanning is being used by some surgeons to help decide if surgery should be performed. If a large gap is present (Figure 12-1), some surgeons believe surgery should be performed to reappose the torn ends of the tendon, whereas if the ends of the tendon are not retracted, nonsurgical treatment is preferred. No papers have been published to show that this is, in fact, scientifically valid. The flexor tendons are easily remembered and identified by using the mnemonic “Tom, Dick, and Harry,” with Tom representing the posterior tibial tendon (PTT); Dick, the flexor digitorum longus; and Harry, the flexor hallucis longus (FHL) (Figure 12-2). The PTT is the most medial and the largest, with the exception of the Achilles, of the flexor tendons. The PTT inserts onto the navicular, second to fourth cuneiforms, and the bases of the second to fourth metatarsals. As it sweeps under the foot, it provides some support for the longitudinal arch; hence, problems in the arch or plantar fascia can sometimes lead to stress on the PTT with resulting tendinosis or even rupture. Posterior tibial tendinosis and rupture are commonly encountered in patients with rheumatoid arthritis. FIGURE 12-2 Rupture of the PTT results clinically in a flat foot as a result of the loss of arch support given by this tendon. The spring ligament runs just deep to the PTT and then goes underneath the neck of the talus, which it supports in a slinglike fashion. When the PTT tears, the stress is then placed on the spring ligament to support the talus and the arch. The spring ligament has a high incidence of disruption when the PTT tears. Once the PTT and the spring ligament tear, the next structure to fail is the subtalar joint ligaments: the sinus tarsi. We looked at 20 patients with PTT tears and found that 92% of them had abnormal spring ligaments (thickened or torn) and 75% had an abnormal sinus tarsi.2 It’s clear that these structures are linked and injury or stress to one can affect the others. Differentiation of partial tears from tendon rupture can be difficult clinically, and MRI examination has become very valuable for making this distinction.3 Most surgeons will operate on a disrupted PTT, whereas nonoperative therapy is usually preferred for partial tears. Posterior tibial tendinosis is seen on axial T1- or T2-weighted images as swelling and/or signal within the normally low-signal tendon on one or more images (Figure 12-3). The increased signal should not be fluid bright on the T2-weighted images. Tendon disruption is diagnosed by noting the absence of low-signal tendon on one or more axial image (Figure 12-4). This typically occurs just at or above the level of the tibiotalar joint. FIGURE 12-3 FIGURE 12-4 The spring ligament is identified on axial and coronal images just deep to the PTT. When it is stressed, it typically gets scarred and thickened (Figure 12-5). A tear can be diagnosed by noting a gap in the ligament. The FHL is known as the Achilles tendon of the foot in ballet dancers because of the extreme flexion position they frequently employ. Ballet dancers often have tenosynovitis of the FHL, seen on MRI scans as fluid in the sheath surrounding the tendon. Care must be taken to have clinical correlation, because up to 20% of healthy people have a communication between the ankle joint and the FHL tendon sheath; therefore fluid can be seen in the FHL tendon sheath from a connection to an ankle joint, which has an effusion. Rupture of the FHL is rare. Disruption of the superior retinaculum, often seen in skiing accidents, can result in displacement of the peroneal tendons (Figure 12-6), which must be surgically corrected. It often occurs with a small bony avulsion, called a flake fracture, off of the fibula caused by the avulsed superior retinaculum.
Magnetic resonance imaging of the foot and ankle
Tendons
Achilles tendon
Posterior tibial tendon
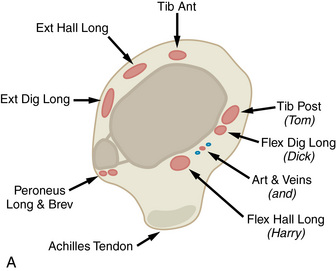

 Normal ankle anatomy. A, This drawing of the tendons around the ankle at the level of the tibiotalar joint shows the relationship of the flexor tendons posteriorly and the extensor tendons anteriorly. B, An axial T1-weighted image through the ankle just above the tibiotalar joint shows the normal anatomy. A, Achilles tendon; D, flexor digitorum tendon; H, flexor hallucis tendon; P, peroneal tendons; T, posterior tibial tendon; TA, tibialis anterior tendon.
Normal ankle anatomy. A, This drawing of the tendons around the ankle at the level of the tibiotalar joint shows the relationship of the flexor tendons posteriorly and the extensor tendons anteriorly. B, An axial T1-weighted image through the ankle just above the tibiotalar joint shows the normal anatomy. A, Achilles tendon; D, flexor digitorum tendon; H, flexor hallucis tendon; P, peroneal tendons; T, posterior tibial tendon; TA, tibialis anterior tendon.
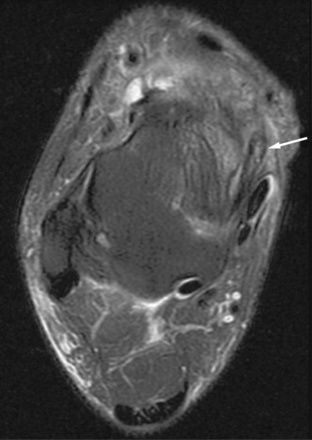
 Posterior tibial tendon tendinosis. A T2-weighted axial image through the ankle shows the posterior tibial tendon (arrow) swollen and containing high signal. This is the appearance of marked tendinosis.
Posterior tibial tendon tendinosis. A T2-weighted axial image through the ankle shows the posterior tibial tendon (arrow) swollen and containing high signal. This is the appearance of marked tendinosis.

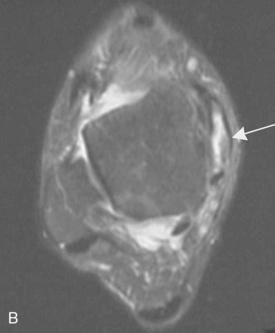
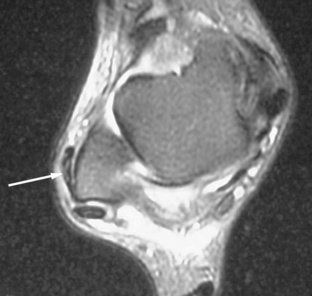
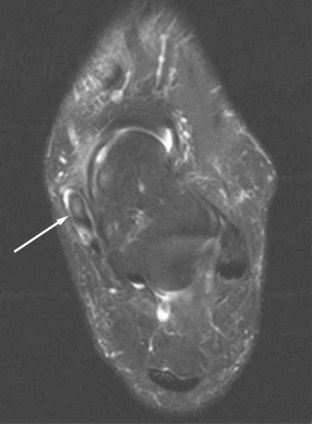
 Torn posterior tibial tendon. Axial T1-weighted (A) and T2-weighted (B) images through the ankle in this patient with chronic pain reveal a distended posterior tibial tendon sheath (arrows) with no low-signal tendon identified within. This is a tear of the posterior tibial tendon.
Torn posterior tibial tendon. Axial T1-weighted (A) and T2-weighted (B) images through the ankle in this patient with chronic pain reveal a distended posterior tibial tendon sheath (arrows) with no low-signal tendon identified within. This is a tear of the posterior tibial tendon.
Flexor hallucis longus
Peroneal tendons
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Magnetic resonance imaging of the foot and ankle