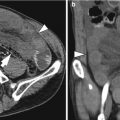
Fig. 15.1
Jejunal adenocarcinoma manifesting as an annular narrowing in a 72-year-old woman. (a) Portal-venous phase CT image shows an annular tumor with concentric luminal narrowing in the proximal jejunum (arrow). (b) Photograph of the gross specimen reveals a circumferential wall thickening (arrows) of the jejunum with luminal narrowing
15.6.2 Small Bowel Adenocarcinoma: Small Bowel Follow-Through and CT Findings
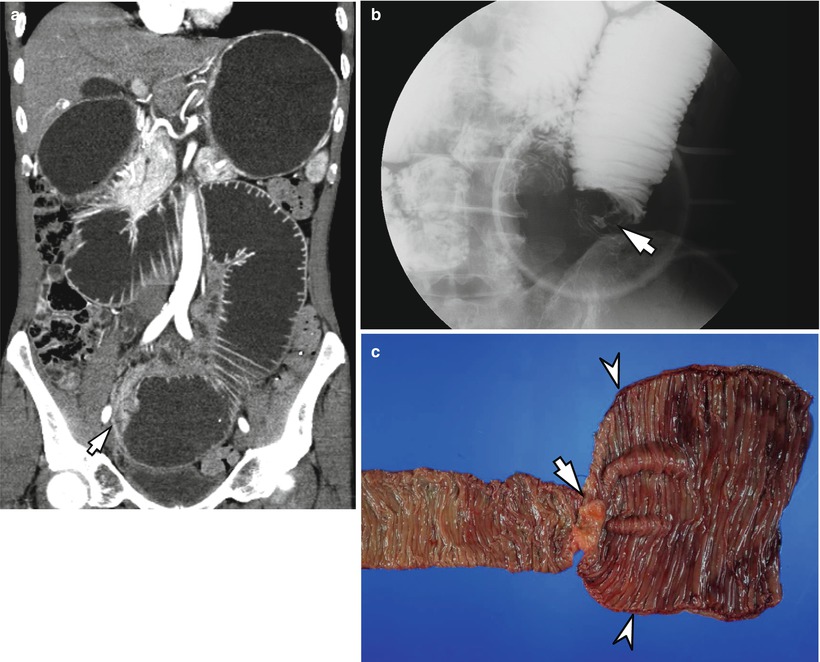
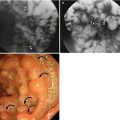
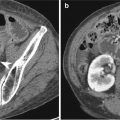
Fig. 15.2
Adenocarcinoma in the jejunum in a 64-year-old man presenting with vomiting. (a) Coronal image of contrast-enhanced CT shows mild wall thickening (arrow) in the jejunum. Note the dilated, fluid-filled proximal small bowel and stomach. (b) Spot radiograph from a small bowel follow-through reveals a short segment of circumferential narrowing (arrow) in the jejunum with overhanging edges which is the typical finding of adenocarcinoma. (c) Photograph of the gross specimen shows an annular tumor (arrow) and a markedly dilated jejunum (arrowheads) proximal to the tumor
15.6.3 Carcinoma of the Ampulla of Vater: MRI Findings
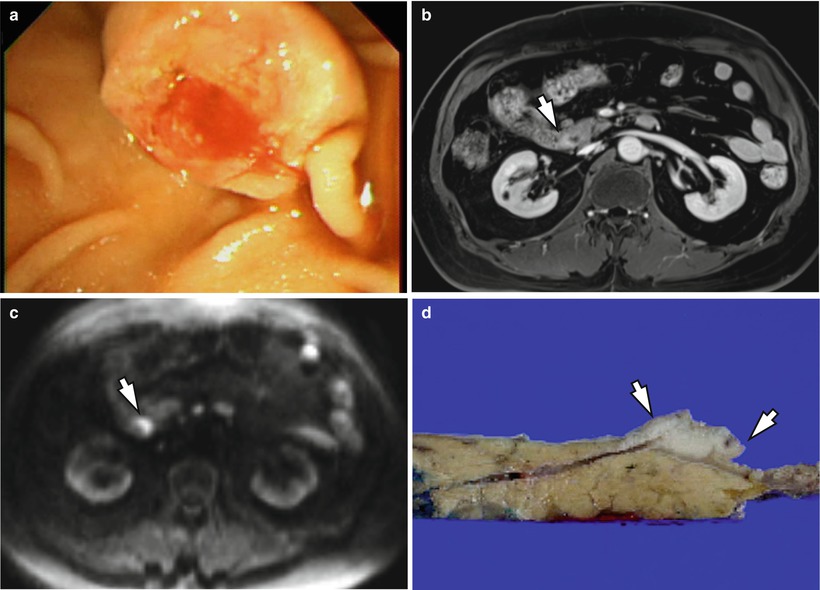
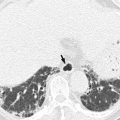
Fig. 15.3
Adenocarcinoma in the ampulla of Vater presenting with jaundice. (a) Endoscopic image demonstrates an ulcerated polypoid mass encroaching the ampulla of Vater. (b) Contrast-enhanced MR image shows an eccentric tumor (arrow) with mild enhancement at the ampulla of Vater. (c) High b-value (b = 1,000) diffusion-weighted image demonstrates a hyperintensity of the lesion (arrow). (d) Specimen photograph shows a protruded mass (arrows) with ulceration at the ampulla of Vater
15.6.4 Peutz-Jeghers Syndrome Associated with Adenocarcinoma
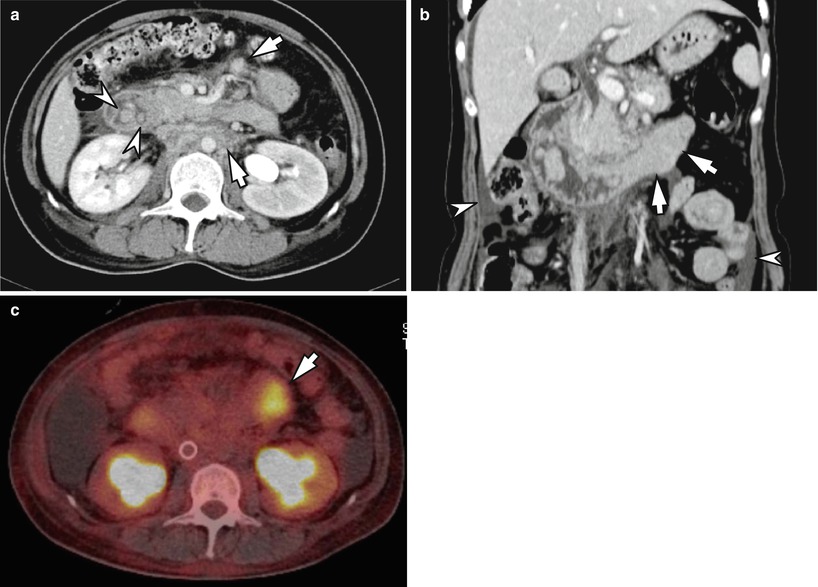
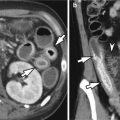
Fig. 15.4
Duodenal adenocarcinoma in a 47-year-old woman with Peutz-Jeghers syndrome. (a) Contrast-enhanced CT image shows multiple polyps (arrowhead) in the duodenum. There are multiple enhancing lymph nodes (arrows) in the mesentery and para-aortic space which are highly suggestive of lymph node metastases.(b) Coronal reformatted CT image shows enhancing intraluminal tumor (arrows) affecting the duodenal third portion which causes bowel obstruction. Cytology results for the ascites (arrowheads) were positive for adenocarcinoma. (c) 18F-FDG PET-CT image demonstrates hypermetabolic mass in the duodenum
15.6.5 Crohn’s Disease Associated with Adenocarcinoma (Crohn’s Carcinoma)

Fig. 15.5
Adenocarcinoma in a 39-year-old woman with long-standing Crohn’s disease. Coronal reformatted CT image shows a segmental wall thickening (arrows) in the small bowel causing bowel obstruction. Note the transmural enhancement of the wall thickening. Adenocarcinoma in the jejunum was proved by surgical resection
15.6.6 Neuroendocrine Tumor, Grade 1 (Carcinoid Tumor)
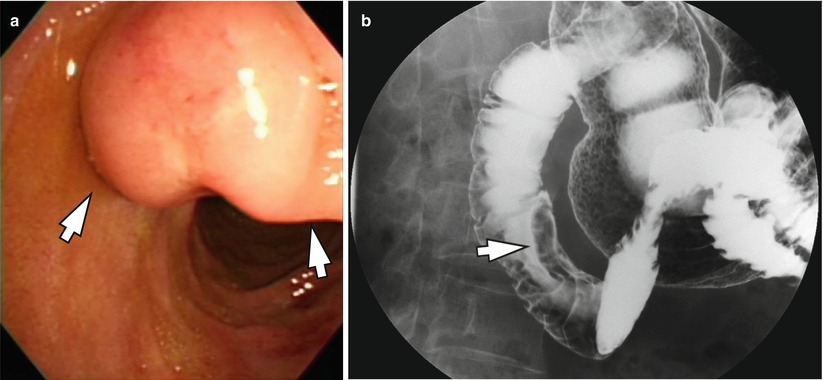
Fig. 15.6
Duodenal neuroendocrine tumor, grade 1 (Carcinoid tumor) in a 64-year-old woman. (a) Endoscopy shows a smooth subepithelial mass (arrows) in the duodenum. Note the intact overlying mucosa. (b) Barium study shows a subepithelial mass (arrow) with smooth, well-defined borders in the second portion of the duodenum. This mass was confirmed as a carcinoid tumor
15.6.7 Neuroendocrine Carcinoma: CT and PET-CT Findings
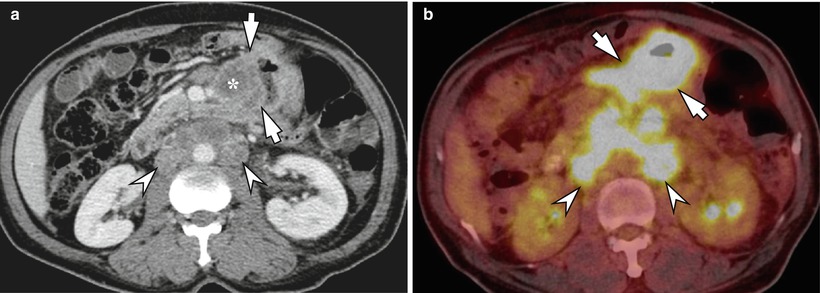
Fig. 15.7
Neuroendocrine carcinoma in the jejunum with lymph node metastases. (a) Contrast-enhanced CT image shows an eccentric wall thickening (arrows) in the jejunum which is conglomerated with the enlarged mesenteric lymph nodes (asterisk). There are multiple metastatic lymph nodes in the para-aortic space (arrowheads). (b) 18F-FDG PET-CT image shows a hypermetabolic lesion affecting jejunum and adjacent mesentery (arrows). Metastatic lymph nodes (arrowheads) in the para-aortic space demonstrate hypermetabolism
15.6.8 Gastrointestinal Stromal Tumor: Small Bowel Follow-Through and CT Findings
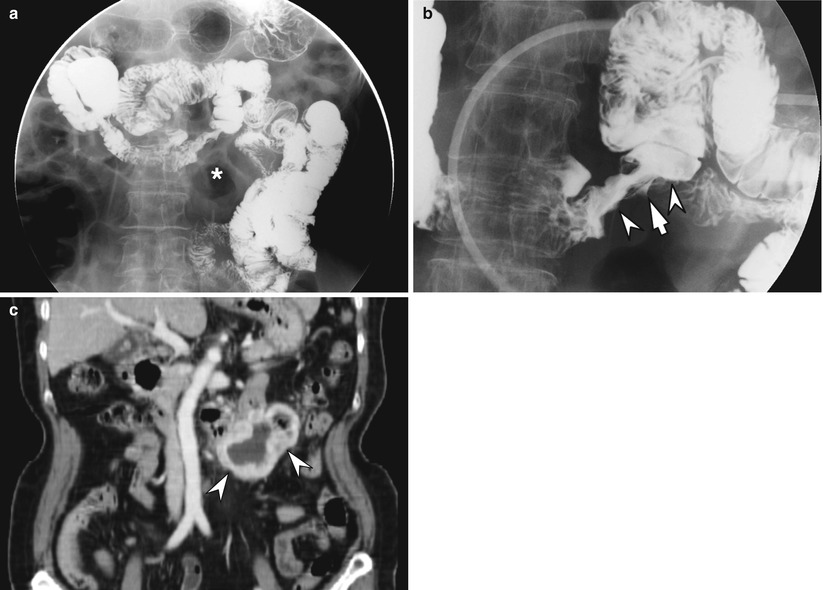
Fig. 15.8




Gastrointestinal stromal tumor in a 72-year-old woman. (a) Spot radiograph from a small bowel follow-through shows an area of mass effect (asterisk) displacing the small bowel loops. (b) An irregular eccentric mass (arrowheads) is seen in the duodenum. Note the focal ulceration (arrow) of the overlying mucosa. (c) Coronal reformatted CT image shows an exophytic mass (arrowheads) arising from the duodenum with internal necrosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree