Management of a Diagnostic Breast Center
Cancer is a topic that provokes anxiety. In our industrialized society, breast cancer is the most common cancer in women, and represents a particular threat. It is not surprising, therefore, that not only the actual revelation of ambiguous breast findings but even the early diagnostic setting itself arouses feelings of apprehension in many women. Thus, the evident quality and friendliness of the professional medical personnel, the quality and range of the devices and procedures offered, and provision of a pleasant ambience help create an environment that is as anxiety-free as possible and in which care can be provided without adding to the patient’s insecurities.
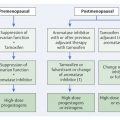
High-quality breast diagnostics is founded and supported on three pillars (▶ Fig. 14.1). It is important to note that deficiencies in one pillar cannot be compensated for by making a special effort in one of the others. It follows that each individual pillar must provide maximum quality so that they jointly ensure the highest level of breast diagnostic quality.

Fig. 14.1 Quality aspects of high-quality breast diagnostics. ACR, American College of Radiology. PGMI (classification) perfect, good, moderate, or inadequate.
14.1 Expertise
In addition to the technical-methodological aspects, breast diagnostics requires a special expertise on the part of the personnel involved in the entire process. This affects the radiologic technologists on the one hand and the physicians on the other.
Given the natural anatomical differences between the women to be examined, generating the mammograms makes high demands of the diagnostic radiographers. For this reason, specific courses have been established in American and European countries to certify that the radiologic technologists performing mammograms meet specific qualification requirements. The quality of all completed mammograms should be reviewed and coded according to the PGMI classification (perfect, good, moderate, or inadequate). The proportion of images classified as “perfect” or “good” should be at least 75%.
A physician’s expertise correlates first and foremost with the extent of their experience in evaluating mammographic images. It is well established that the learning curve for physicians who interpret mammograms rises over a time period of 8 to 10 years, assuming that 3,000 to 5,000 mammograms are read per year. These physicians then have stored mental image patterns that allow them to recognize pathologic processes in the mammogram within a few seconds.
The American College of Radiology (ACR) Mammography Accreditation Program for interpreting physicians calls initially for board certification in radiology, interpretation, and documentation of 240 mammograms within 6 months, and 15 units of category I continuing medical education (CME) in mammography. For continuing experience, 960 mammographic examinations must be interpreted over a period of 2 years. Continuing education requires 15 units of category I CME within 3 years.
The ACR also gives specifications for breast ultrasound accreditation. Interpreting physicians are required, among other things, to perform or oversee, interpret, and document 300 breast ultrasounds within 36 months. To maintain the certification, for example, 200 breast ultrasound examinations can be performed and a total of 15 hours CME completed within 3 years. Minimum criteria to be met by a physician who performs or supervises ultrasound-guided biopsies are the qualification to interpret mammograms under MQSA (Mammography Quality Standards Act) and the performance of 36 image-guided biopsies within 36 months.
Minimum criteria required by the ACR for breast MRI accreditation are, for example, board certification in radiology or diagnostic radiology, interpretation, and documentation of 150 breast MRI examinations within 3 years and completion of 15 hours of category I CME in MRI. To renew the certification, 75 independent examinations must be interpreted within the prior 36 months. In order to meet ACR general quality standards, certain requirements, such as a dedicated breast coil, bilateral examinations, and the means for performing MRI-guided interventions are specified.
In European countries there are similar certification requirements and course programs for all breast imaging modalities. As an example, in Germany, the AIM e.V. (Arbeitsgemeinschaft für individuelle Mammadiagnostik [Working Group for Individualized Breast Diagnostics]) has defined two quality levels: “Level 1” (high level) and “Level 2” (professional level) to ensure the quality of high-resolution breast MRI. In addition to device and technical-methodological requirements, certified radiologists must independently interpret 250 breast MRI examinations per year for Level 1, and 500 per year for Level 2 (▶ Table 14.1). In addition, certification requirements for the performance of percutaneous biopsy examinations prescribe country-specific numbers of ultrasound-, mammography-, and MRI-guided interventions within a certain period for accreditation.
Requirement | Level 1 | Level 2 |
System | ≥1.5 T | ≥1.5 T |
Spatial resolution | 512 × 512 | 512×512 |
Temporal resolution | <2 min/sequence | <2 min/sequence |
Coil | Open, bilateral | Open, bilateral |
Breast fixation | Yes | Yes |
Postprocessing | Subtraction, maximum intensity projection. | Subtraction, maximum intensity projection. |
Number of patients per examiner per year | > 250 | > 500 |
Interventions per examiner per year | Cooperation | >50 biopsies >50 localizations |
CME in breast MRI | > 8 h/year | > 16 h/year |
Abbreviation; AIM, Arbeitsgemeinschaft individuelle Mammadiagnostik (Working Group for Individualized Breast Diagnostics). CME, continuing medical education. Source: http://www.aim-mamma.de/tl_files/downloads/open/aim-info-aerzte.pdf (accessed March 28, 2013). | ||
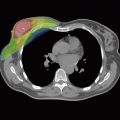
14.2 Equipment
As well as providing all the devices and means for breast imaging, a diagnostic breast center should also have available all the equipment needed to perform percutaneous biopsies in the diagnostic work-up of ambiguous findings. Because of its many advantages in terms of radiation exposure, data storage, and image postprocessing and evaluation, digital mammography has now almost completely superseded analog imaging. In addition to the digital mammography unit itself, digital imaging necessitates the provision of a diagnostic viewing station with screen monitors that must meet the high demands of breast diagnostics. Both the mammography unit and the review workstation must meet performance requirements in terms of resolution, contrast, and diagnostic quality. In the United States, these units are tested by a medical physicist and must meet the requirements of the Mammography Quality Standards Act to be certified.