Case presentation
A 13-year-old male presents to the emergency department (ED) with 2 weeks of chest pain. He describes the pain as sharp and constant, worsening over the past week. Two weeks ago, the patient had fever to 102 degrees Fahrenheit and cough. He then developed sharp frontal chest pain that he described as “stabbing.” The pain worsened when lying down. He was seen by his primary care provider and at that time had a chest radiograph and electrocardiogram (ECG) that were reported to be normal. He was diagnosed with a viral infection and prescribed symptomatic care. His fevers have resolved but the chest pain has worsened. He denies vomiting, abdominal pain, back pain, difficulty breathing, or trauma.
Physical examination reveals unremarkable vital signs other than mild tachycardia (heart rate of 110 beats per minute with a blood pressure of 110/70 mm Hg). He has slightly distant heart sounds and there appears to be a friction rub without a discernable murmur. His lungs are clear. An ECG is obtained, demonstrating low voltage throughout with no other acute abnormalities.
Imaging considerations
The choice of imaging modalities will depend on the clinical presentation, but when pericarditis is suspected, it will typically begin with plain chest radiography and may be followed by bedside ultrasound (US), echocardiogram, cardiac computed tomography (CT), or cardiac magnetic resonance imaging (MRI).
Plain radiography
Chest imaging may be normal in many patients with early or mild cases of pericarditis. In addition to helping to identify other etiologies of chest pain or fever in patients with potential pericarditis, findings can include cardiomegaly (most often due to a pericardial effusion referred to as a “water bottle sign”). Associated findings may also include pleural effusion, pulmonary edema, lung infiltrates, or an enlarged mediastinum. , A pericardial effusion may distort the cardiac silhouette, but often, chest radiography appears unremarkable. Plain radiography is also useful to detect other causes of chest pain, such as pneumothorax, rib fractures, pleural effusion, and pneumonia. This modality is readily available, rapid, and exposes the patient to minimal ionizing radiation.
Cardiac US/echocardiography
Transthoracic echocardiography is an excellent imaging modality for patients with a suspected cardiac process, including pericarditis. This modality can detect pericardial effusion, assess cardiac function, and be useful to distinguish between pericarditis and myocarditis (in which cardiac dysfunction is usually present).
If possible, a point of care cardiac US should be performed on all suspected cases of pericarditis to evaluate for pericardial effusion and signs of cardiac tamponade, since this modality is highly sensitive and specific (96% and 98%, respectively) for pericardial effusion. In particular, bedside imaging is critical in ill-appearing or hypotensive patients, where early identification of an effusion and tamponade physiology can guide management and resuscitation including pericardiocentesis. Echocardiography by Pediatric Cardiology can help to identify smaller effusions, especially in patients who do not present in more advanced disease states.
Cardiac CT
This imaging modality may be used in patients with chronic or constrictive pericarditis but is not indicated in the acute period of illness. ,
Cardiac MRI
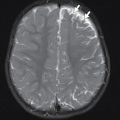
Cardiac MRI is not typically indicated in the ED setting or in the acute course, but if the diagnosis is uncertain or additional complications such as constrictive pericarditis, complex effusion, and myocardial involvement are considered, these can be identified through the use of MRI.
Imaging findings
This patient had a bedside point-of-care US (POCUS) performed in the ED, which revealed grossly normal cardiac function but the presence of a pericardial effusion. Pediatric Cardiology was consulted. Since he was deemed stable for a more confirmatory study, the decision was made to perform cardiac MRI. Select images from this study are provided. There is a moderate pericardial effusion noted, with thickened and enhancing pericardium, but the study was otherwise unremarkable ( Figs. 11.1–11.3 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree