Fig. 4.1
There are a large number of parameters and settings which may be modified by the user. These seven represent commonly used adjustments and functions for manipulating image quality
This chapter will explore the use of each of these “user-controlled” variables emphasizing the underlying physical principles and defining the clinical circumstances under which these adjustments may be necessary.
Transducer Selection
Selection of the transducer is critical to maximizing image quality . The physical shape of the transducer may be important in certain circumstances. The image that is produced by a transducer may be recognized by its shape. A linear array transducer produces a rectangular image whereas a curved array transducer produces an image which is trapezoidal in shape (Fig. 4.2).
Fig. 4.2
(a) The linear array transducer produces a rectangular image field. (b) The curved array transducer produces a trapezoidal or pie-shaped image. The shape of the transducer affects the divergence of the sound wave as it propagates in the body
Linear array transducers are most commonly used in urology for imaging of the testes and male genitalia. The curved array transducer is more frequently used for abdominal scanning. The curved nature of the probe allows gentle pressure on the patient’s abdomen or flank resulting in contact of the entire transducer face with the skin. Curved array transducers are useful for imaging between ribs or angling beneath the pubic symphysis.
Transducers are usually multifrequency, meaning the frequency can be switched electronically over a range of frequencies (e.g., 2.5–6 mHz for an abdominal transducer). It is important to select the highest frequency which has adequate depth of penetration for the anatomic area of interest. The higher the frequency of the transducer, the greater the axial resolution and the better the anatomic representation of the image. However, there is a trade-off between frequency and depth of penetration. Imaging of the kidneys requires a lower frequency to penetrate to a depth of 6–14 cm below the surface of the skin. Thus, renal scanning is usually performed with a curved array transducer between 2.5 and 6 mHz. By contrast, because of the close proximity of the testes to the surface of the skin, scanning of the testis can be performed with high frequency transducer, producing excellent axial resolution. A linear array transducer at 12 mHz is often used for testicular ultrasound. Transrectal ultrasound of the prostate often employs a transducer of 7.5 mHz since it offers an optimal combination of depth of penetration and axial resolution for the average-sized gland (Fig. 4.3).
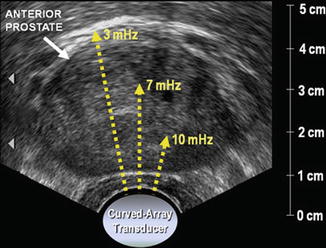
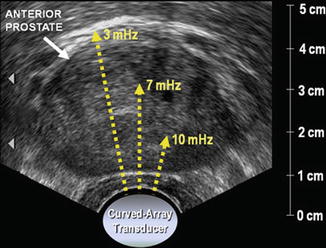
Fig. 4.3
The selection of a transducer with the frequency of 7.5 mHz reflects the trade-off between depth of penetration and good axial resolution. In this axial image of a large prostate, a lower scanning frequency may be needed to adequately visualize the anterior prostate
Scanning Environment
To produce the best-quality image, the sonographer should arrange the scanning environment so that the interfaces between patient, sonographer, and equipment are optimized. The patient should be positioned at a height which allows the sonographer to stand or sit in a comfortable position so that the sonographer is able to stabilize the transducer against the patient’s body. This minimizes unwanted movement of the transducer and allows the sonographer to maintain the orientation and position of the transducer while adjusting machine features (Fig. 4.4).


Fig. 4.4
The configuration of the equipment and proximity to the patient are critical in maximizing comfort, efficiency, and accuracy during scanning and documentation
The sonographer must have the ability to comfortably reach the physical console or touch screen in order to adjust the machine setting. Many ultrasound units provide the ability to freeze and unfreeze the transducer via a button on the transducer itself or by a foot switch. In either case, the sonographer must be able to scan the patient with one hand while manipulating the console and documenting with the other hand.
The sonographer must have a clear direct view of the monitor. The angle of the monitor should be adjusted for viewing by the sonographer. The brightness settings on the monitor need to be adjusted for the conditions under which the scan is being performed . In general, dimming the room lights improves the ability to evaluate the image on the monitor.
Monitor Display
It is important when performing an ultrasound examination to understand the information that is available on the monitor. Patient demographic information, type of exam, and facility should be entered. The monitor will usually display information regarding which probe is active, the frequency of the probe, and the magnification of the image. Information regarding overall gain and other settings is available on the monitor. Typically, there will be a TGC curve displayed on one side of the image as well as color bar which demonstrates the range of pixel brightness or hues available. In addition, there will be gradient markings on one side so that depth of field can be appreciated (Fig. 4.5).
Fig. 4.5
Some of the machine settings are displayed on the monitor. Knowing where these settings are displayed and what they mean assists in optimizing image quality
By convention, when scanning organs in the sagittal view, the upper pole of the organ (e.g., kidney or testis) is to the left of the screen and the lower pole is to the right of the screen (Fig. 4.6).
Fig. 4.6
In this sagittal image of the left testis, the superior pole of the testis (A) is to the left and the inferior pole of the testis (B) is to the right. The anterior aspect of testis (C) is at the top of the image and the posterior aspect (D) is at the bottom. Without the label “LtTestSag,” there would be no way to distinguish the right from the left testis
In transverse scanning, the right side of an anatomic structure is displayed on the left side of the image just as it would be when evaluating a conventional radiograph. These conventions should always be followed when documenting an ultrasound examination; however, it may be useful to also demonstrate the orientation of the probe using graphics or icons. When paired structures such as the kidneys or testes are imaged, it is particularly important to designate the organ as right or left.
User-Controlled Variables
One of the most commonly required adjustments during ultrasound scanning is an adjustment to the overall gain. The gain is a control which determines the degree to which the electrical signal produced by a returning sound wave when it strikes the transducer will be amplified for display. This needs to be differentiated from acoustic output which is defined as the power or amplitude of the afferent wave which is generated by the transducer (Fig. 4.7).


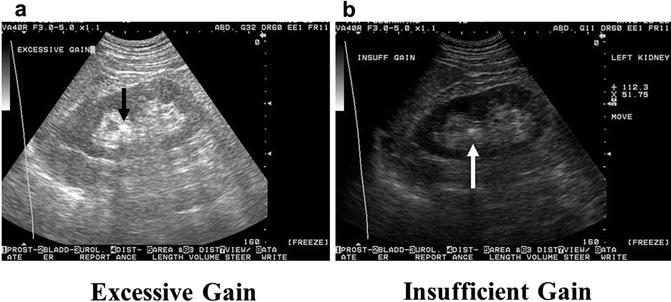
Fig. 4.7
A typical console interface showing common user-controlled variables
Both gain and acoustic power can be controlled by the operator; however, acoustic output is limited by the manufacturer in compliance with industrial safety standards [1]. In general, when the gain is increased the resultant image is brighter or more hyperechoic. When there is excessive overall gain, the image often appears bright and washed out. When there is insufficient overall gain, the image is often dark and it is difficult to distinguish between adjacent structures (Fig. 4.8).