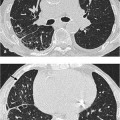
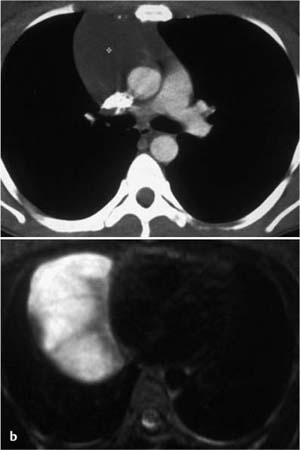
10 Mediastinal Disorders Most common mediastinal cysts Bronchogenic cysts arise from the ventral foregut, enteric cysts from the dorsal foregut MRI is equivalent to CT. Smoothly demarcated, thin-walled, cystic, spherical or ellipsoid mass showing no enhancement with contrast Water-equivalent density and signal intensity One-third are asymptomatic incidental findings Complete surgical resection is usually indicated even for asymptomatic cysts Prognosis is excellent following complete excision. Diagnosis and differential diagnosis Fig. 10.1 Pericardial cyst in a 52-year-old woman (incidental finding). The plain chest radiograph (a) shows a circumscribed convex shadow in the right cardiophrenic angle with a cardiac silhouette sign. The shape and location suggest a pericardial cyst. This was confirmed on MRI, where the lesion exhibited signal intensity typical of a cyst (b). Fig. 10.2 MR image of a bronchogenic cyst. The cyst has a typical spherical shape, is smoothly demarcated, thin-walled, and exhibits homogeneous, fluid-equivalent density.
Mediastinal Cysts
Definition
 Epidemiology
Epidemiology
 Developmental anomalies of the embryonal foregut
Developmental anomalies of the embryonal foregut  Isolated cystic lesions
Isolated cystic lesions  Forms include pericardial cysts, thymic cysts, bronchogenic cysts, esophageal duplication cysts, and neuroenteric cysts.
Forms include pericardial cysts, thymic cysts, bronchogenic cysts, esophageal duplication cysts, and neuroenteric cysts.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
 Bronchogenic cysts contain respiratory epithelium, smooth muscle, and cartilage; enteric cysts contain squamous and gastrointestinal epithelium, smooth muscle, and nerve plexus.
Bronchogenic cysts contain respiratory epithelium, smooth muscle, and cartilage; enteric cysts contain squamous and gastrointestinal epithelium, smooth muscle, and nerve plexus.
Imaging Signs
 Modality of choice
Modality of choice
 CT and MRI findings
CT and MRI findings
 Cysts with serous contents (most common) exhibit water-equivalent density (most common in pericardial cysts), those with other contents (mucus, calcium milk, blood) show higher density
Cysts with serous contents (most common) exhibit water-equivalent density (most common in pericardial cysts), those with other contents (mucus, calcium milk, blood) show higher density  Bronchogenic cysts
Bronchogenic cysts  Cysts rarely communicate with the tracheobronchial or esophageal lumen (air–fluid level)
Cysts rarely communicate with the tracheobronchial or esophageal lumen (air–fluid level)  On MRI, cysts show variable signal behavior depending on the contents, typically appearing markedly hyperintense on T2-weighted sequences and hypointense or hyperintense on T1-weighted sequences
On MRI, cysts show variable signal behavior depending on the contents, typically appearing markedly hyperintense on T2-weighted sequences and hypointense or hyperintense on T1-weighted sequences  Bronchogenic cysts are usually subcarinal and paratracheal (> 50% on the right side, 15% in the pulmonary region)
Bronchogenic cysts are usually subcarinal and paratracheal (> 50% on the right side, 15% in the pulmonary region)  Esophageal duplication cysts usually occur in a distal paraesophageal location (more often on the right than left) and are rarely intramural
Esophageal duplication cysts usually occur in a distal paraesophageal location (more often on the right than left) and are rarely intramural  Neuroenteric cysts occur in the mediastinum superior to the carina and in 50% of cases are associated with spinal anomalies.
Neuroenteric cysts occur in the mediastinum superior to the carina and in 50% of cases are associated with spinal anomalies.
 Pathognomonic findings
Pathognomonic findings
 No enhancement
No enhancement  Typical location
Typical location  Neuroenteric cysts are associated with spinal anomalies.
Neuroenteric cysts are associated with spinal anomalies.
Clinical Aspects
 Typical presentation
Typical presentation
 Two-thirds are symptomatic (causing airway or esophageal obstruction) and usually already manifest in infancy.
Two-thirds are symptomatic (causing airway or esophageal obstruction) and usually already manifest in infancy.
 Therapeutic options
Therapeutic options
 Pericardial cysts usually require no treatment.
Pericardial cysts usually require no treatment.
 Course and prognosis
Course and prognosis
 What does the clinician want to know?
What does the clinician want to know?
 Location and extent (resection)
Location and extent (resection)  Impairment of adjacent structures.
Impairment of adjacent structures.
Differential Diagnosis
Thymus cyst | – Location: upper anterior mediastinum |
Pericardial cyst | – Pericardial contact – Usually in the cardiophrenic angle (right side in 70% of cases, left in 22%) – Invariably water equivalent |
Lymphangioma | – Occurs in infancy – Multicystic or septate – With axial or cervical ramifications |
Meningocele | – Paravertebral cystic formation isodense and isoin-tense to CSF and continuous with the dural sac – Occasionally with widening of the neural foramen |
Tumor cysts | – Thymic and germ cell tumors: solid tumor components predominate |
Pancreatic pseudocyst | – Signs of a complicated cyst (irregularity, septation, marginal enhancement, reaction in adjacent tissue) – History of pancreatitis |
Fig. 10.3 Thymic cyst.
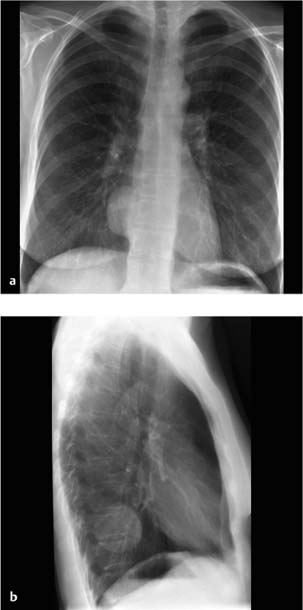
a The plain chest radiograph shows a widening of the mediastinal shadow on the right by a large, smoothly demarcated paracardiac mass with a shallow convex lateral margin obscuring the right margin of the heart (silhouette sign).
b CT (above) and MRI (below) show liquid cystic findings. The thymic cyst was confirmed intraoperatively. The size and cranial location are largely inconsistent with a pericardial cyst.
Tips and Pitfalls
Can be misdiagnosed as a solid mass  Complicated cysts are not clearly distinguishable from cystic tumors.
Complicated cysts are not clearly distinguishable from cystic tumors.
Selected References
Jeung MY et al. Imaging of cystic masses of the mediastinum. Radiographics 2002; 22: 79–93
Kim JH, Goo JM, Lee HJ. Cystic tumors in the anterior mediastinum: radiologic-pathological correlation. J Comput Assist Tomogr 2003; 27: 714–723
Strollo DC, Rosado-de-Christensom ML, Jett JR. Primary mediastinal tumors: Part 1 Tumors of the anterior mediastinum. Part 2 Tumors of the middle and posterior mediastinum. Chest 1997; 112: 511–522, 1344–1357
Takeda S, Miyoshi S, Minami M. Clinical spectrum of mediastinal cysts. Chest 2003; 124: 125–132
Retrosternal Intrathoracic Goiter
Definition
 Epidemiology
Epidemiology
Goiter occurs on average in about 5% of the population (in Germany), about 20% of these have an intrathoracic component  Three times as common in women than in men.
Three times as common in women than in men.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Primary goiter occurs with an accessory intrathoracic thyroid (with thoracic vascular supply)  Secondary goiter develops as a ramification of a cervical goiter (with cervical vascular supply)
Secondary goiter develops as a ramification of a cervical goiter (with cervical vascular supply)  Develops in response to thyroid-stimulating hormone in iodine deficiency or thyroid insufficiency.
Develops in response to thyroid-stimulating hormone in iodine deficiency or thyroid insufficiency.
Imaging Signs
 Modality of choice
Modality of choice
Radiographs, CT, nuclear medicine.
 Radiographic findings
Radiographic findings
Smoothly demarcated space-occupying lesion in the anterior upper mediastinum that moves when the patient swallows and leads to tracheal shift and/or compression  Calcifications occur in 25% of cases.
Calcifications occur in 25% of cases.
 CT findings
CT findings
Smoothly demarcated mass appearing hyperdense on plain scans due to iodine (70–120 HU) and located in the upper mediastinum (75% anterior to the trachea, 25% posterior)  Tracheal shift (occasionally with compression)
Tracheal shift (occasionally with compression)  Calcifications and colloid cysts are common findings
Calcifications and colloid cysts are common findings  Enhances markedly on contrast-enhanced
Enhances markedly on contrast-enhanced  Contrast-enhanced CT scans should be performed only after nuclear medicine studies.
Contrast-enhanced CT scans should be performed only after nuclear medicine studies.
 Nuclear medicine
Nuclear medicine
Nuclide uptake (iodine-123) equivalent to thyroid tissue.
 Pathognomonic findings
Pathognomonic findings
Mass in the anterior upper mediastinum continuous with the thyroid and displacing and/or compressing the trachea and/or esophagus.
Clinical Aspects
 Typical presentation
Typical presentation
Usually asymptomatic where only mild hypothyroidism is present (variable thyroid function is normal; thyroid function tests are indicated)  Stridor and/or dyspnea, dysphagia, and dysphonia depending on size and location.
Stridor and/or dyspnea, dysphagia, and dysphonia depending on size and location.
 Therapeutic options
Therapeutic options
Surgical resection is indicated for large symptomatic goiters and where malignancy is suspected  Thyroid function tests are invariably indicated.
Thyroid function tests are invariably indicated.
 Course and prognosis
Course and prognosis
Prognosis is good for benign goiters  Prognosis for malignant goiters depends on the histology.
Prognosis for malignant goiters depends on the histology.
 What does the clinician want to know?
What does the clinician want to know?
Confirmation of tentative diagnosis  Determine whether findings appear malignant
Determine whether findings appear malignant  Thyroid function.
Thyroid function.
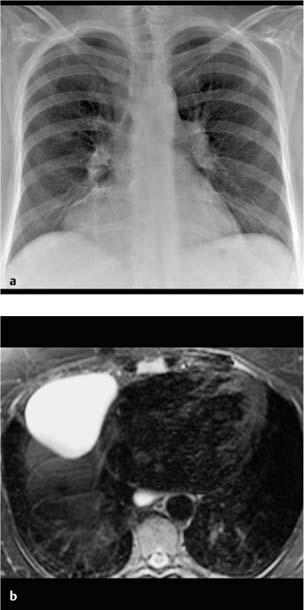
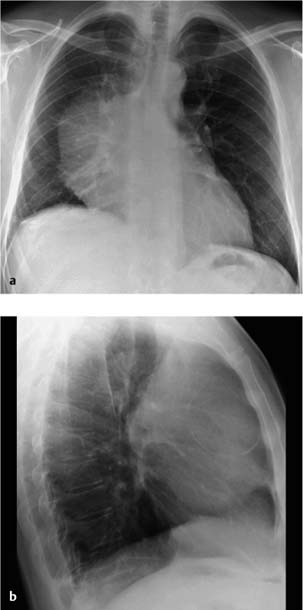
Fig. 10.4 Retrosternal goiter in a 66-year-old woman. The plain chest radiograph shows a space-occupying lesion at the level of the thoracic inlet with coarse patchy calcifications and a right convex tracheal shift. Other findings include a fatty mass in the right paracardiac region.
Differential Diagnosis
Thymic tumor | – Located farther caudally and not continuous with the thyroid – Lesser density and enhancement on CT |
Teratoma | – Located farther caudally and not continuous with the thyroid – Lesser density and enhancement on CT – Fatty components |
Lymphoma | – No calcifications initially – Multinodular – Lesser density and enhancement on CT |
Castleman disease | – Strong contrast enhancement similar to goiter – Not continuous with the thyroid – Multinodular and multilocular |
Tips and Pitfalls
Difficulties with differential diagnosis are to be expected only with the primary form.
Selected References
Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005; 128: 2893–2909
Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: Part 1 Tumors of the anterior mediastinum. Chest 1997; 112: 511
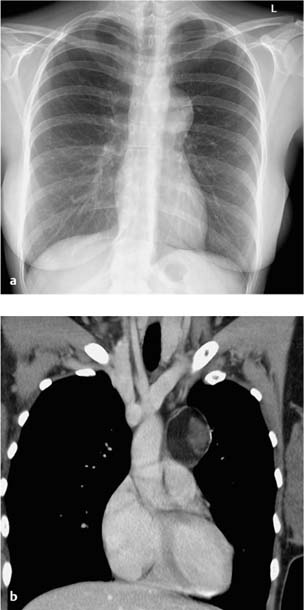
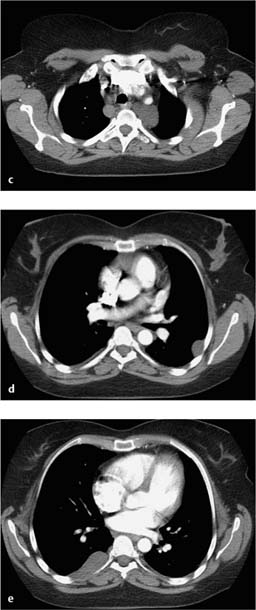
Fig. 10.5 Retrosternal goiter in a 76-year-old woman. The axial (b) and coronal CT-images show a severe cervical goiter with regressive changes (cystic necrotic components and calcifications). The goiter extends far into the anterior upper mediastinum, significantly displacing the carotid arteries and brachiocephalic veins. The trachea shows a right convex shift with only slight compression. The cardinal diagnostic criteria are the continuity of the mediastinal mass with the thyroid and its equivalent texture.
Thymic Tumors
Definition
 Epidemiology
Epidemiology
Account for about 20% of primary mediastinal tumors  Most common mass in the anterior mediastinum aside from teratoma, lymphoma, and goiter
Most common mass in the anterior mediastinum aside from teratoma, lymphoma, and goiter  Occurs exclusively in the anterior mediastinum anterior to the heart and great vessels
Occurs exclusively in the anterior mediastinum anterior to the heart and great vessels  Occurs at age 40–60
Occurs at age 40–60  Often associated with other clinical pictures and findings (especially myasthenia gravis, red cell aplasia, hypogammaglobulinemia).
Often associated with other clinical pictures and findings (especially myasthenia gravis, red cell aplasia, hypogammaglobulinemia).
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
The classification of thymomas is based on the predominant cell type, epithelial or lymphocytic  Encapsulated and invasive lymphomas are histologically identical
Encapsulated and invasive lymphomas are histologically identical  Other thymic tumors and tumorlike processes include thymic cyst, thymic lipoma, thymic carcinoma, and thymic carcinoid.
Other thymic tumors and tumorlike processes include thymic cyst, thymic lipoma, thymic carcinoma, and thymic carcinoid.
Imaging Signs
 Modality of choice
Modality of choice
CT is preferable to MRI.
 CT findings
CT findings
– Thymoma: Solid round or oval smoothly demarcated mass in the anterior upper mediastinum (usually < 10 cm)  Necrotic, cystic, hemorrhagic components
Necrotic, cystic, hemorrhagic components  Calcifications in 25% (not a criterion of malignancy)
Calcifications in 25% (not a criterion of malignancy)  35% of thymomas show locally invasive growth—pericardial thickening, vascular encasement, pleural metastases
35% of thymomas show locally invasive growth—pericardial thickening, vascular encasement, pleural metastases  Invasive forms of thymoma are indistinguishable from thymic carcinoma, thymic carcinoid, or malignant germ cell tumor.
Invasive forms of thymoma are indistinguishable from thymic carcinoma, thymic carcinoid, or malignant germ cell tumor.
– Thymic carcinoma: Usually > 10 cm  Irregular
Irregular  Ill-defined margin
Ill-defined margin  Signs of
Signs of  Heterogeneous enhancement
Heterogeneous enhancement  Involvement of mediastinal lymph nodes in 40% of cases
Involvement of mediastinal lymph nodes in 40% of cases  Metastases (lung, liver) in 30%.
Metastases (lung, liver) in 30%.
– Thymic cyst: Thin-walled  Usually a solitary finding.
Usually a solitary finding.
– Thymic lipoma: Sharply demarcated  Fat-equivalent density.
Fat-equivalent density.
– Thymic carcinoid: Resembles a thymoma  Involvement of mediastinal lymph nodes or metastases in 20–30% of cases.
Involvement of mediastinal lymph nodes or metastases in 20–30% of cases.
 MRI findings
MRI findings
– Thymoma: Isointense to muscle on T1-weighted sequences, cystic components are hypointense  Hyperintense on T2-weighted sequences, cystic components are markedly hyperintense.
Hyperintense on T2-weighted sequences, cystic components are markedly hyperintense.
– Thymic carcinoma: Heterogeneous signal behavior and enhancement.
– Thymic cyst: Hypointense on T1-weighted sequences  Markedly hyperintense on T2-weighted sequences.
Markedly hyperintense on T2-weighted sequences.
 Pathognomonic findings
Pathognomonic findings
Round or oval lobulated mass in the anterior upper mediastinum < 10 cm.
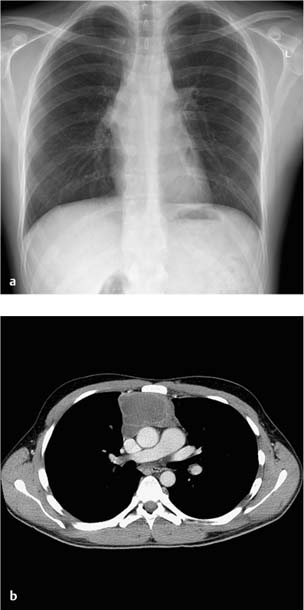
Fig. 10.6 Thymoma in a 43-year-old man. The plain chest radiograph shows a large mass in the right anterior mediastinum. On the lateral film (b) the tumor shows a convex partial calcification. Slightly high-riding right diaphragmatic crus. Histological examination revealed a thymoma with no evidence of malignancy.
Clinical Aspects
 Typical presentation
Typical presentation
– Thymoma: Myasthenia gravis (diplopia, ptosis, weakness) in 50% of cases.
– Thymic carcinoma: Chest pain  Weight loss
Weight loss  Paraneoplastic syndrome in rare ing syndrome
Paraneoplastic syndrome in rare ing syndrome  Multiple endocrine neoplasia (MEN) 1 syndrome.
Multiple endocrine neoplasia (MEN) 1 syndrome.
– Thymic cyst and thymic lipoma: Asymptomatic incidental findings.
 Therapeutic options
Therapeutic options
Resection.
 Course and prognosis
Course and prognosis
Thymoma: Prognosis is good where the capsule is intact, moderate for invasive cases  Thymic carcinoma: Poor prognosis.
Thymic carcinoma: Poor prognosis.
 What does the clinician want to know?
What does the clinician want to know?
Localization and extent (for biopsy and/or resection)  Involvement of adjacent structures.
Involvement of adjacent structures.
Differential Diagnosis
Retrosternal goiter | – Continuous with the thyroid – Higher density than muscle on CT – Regressive changes are common |
Lymphoma | – Thymic involvement in the setting of a generalized lymphoma (usually Hodgkin disease) |
Teratoma or germ cell tumors | – Similar cross-sectional morphology – Clinical findings and laboratory results are required to distinguish these disease entities |
Tips and Pitfalls
Thymic carcinoma is indistinguishable from invasive thymoma on imaging studies  Complete resection is required to distinguish between the two conditions.
Complete resection is required to distinguish between the two conditions.
Selected References
Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005; 128: 2893–2909
Nishino M et al. Thymus—a comprehensive review. Radiographics 2006; 26: 335–348
Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: Part 2 Tumors of the middle and posterior mediastinum. Chest 1997; 112: 1344–1357
Germ Cell Tumors
Definition
 Epidemiology
Epidemiology
Germ cell tumors account for about 15% of primary mediastinal tumors  Predilection for the anterior mediastinum, often adjacent to the thymus
Predilection for the anterior mediastinum, often adjacent to the thymus  Predilection for young men
Predilection for young men  Teratoma is the most common germ cell tumor of the mediastinum, seminoma the most common malignant form.
Teratoma is the most common germ cell tumor of the mediastinum, seminoma the most common malignant form.
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
The germ cell tumors include teratomas (usually benign, rarely teratocarcinomas), seminomas, and nonseminomatous germ cell tumors (embryonal carcinoma, yolk sac tumors, choriocarcinoma, and mixed tumors).
Imaging Signs
 Modality of choice
Modality of choice
CT, MRI.
 CT and MRI findings
CT and MRI findings
– Seminoma: Large solid, usually lobulated mass of homogeneous density; cystic or necrotic areas are rare
– Teratomas: Mature teratomas are the only germ cell tumors to exhibit typical findings (see below)
– Teratocarcinoma: Irregularly demarcated tumor with inhomogeneous contrast enhancement, calcifications, necrosis, and signs of infiltration.
 Pathognomonic findings
Pathognomonic findings
Mature teratomas are the only germ cell tumors to exhibit typical findings on imaging studies—they are well demarcated round or lobulated tumors with cysts, calcifications or ossifications, and fatty tissue (50% of cases)  Primordia of tooth and/or bone or fat–fluid levels are pathognomonic findings.
Primordia of tooth and/or bone or fat–fluid levels are pathognomonic findings.
Clinical Aspects
 Typical presentation
Typical presentation
Asymptomatic incidental finding or symptomatic lesion  Symptomatic tumors (cough, pain, dyspnea, fever) suggest malignancy
Symptomatic tumors (cough, pain, dyspnea, fever) suggest malignancy  AFP is elevated in embryonal
AFP is elevated in embryonal  HCG is elevated in choriocarcinoma
HCG is elevated in choriocarcinoma  Pure seminomas do not show raised AFP and only occasionally raised HCG (10% of cases). Exclude a primary testicular tumor.
Pure seminomas do not show raised AFP and only occasionally raised HCG (10% of cases). Exclude a primary testicular tumor.
 Therapeutic options
Therapeutic options
Mature teratomas: Resection  Seminomas: Combined radiation therapy and chemotherapy
Seminomas: Combined radiation therapy and chemotherapy  Nonseminomatous germ cell tumors: Chemotherapy and resection.
Nonseminomatous germ cell tumors: Chemotherapy and resection.
 Course and prognosis
Course and prognosis
Mature teratomas: Excellent prognosis  Pure seminomas: Very good prognosis
Pure seminomas: Very good prognosis  Mixed tumors: Variable prognosis.
Mixed tumors: Variable prognosis.
 What does the clinician want to know?
What does the clinician want to know?
Localization and extent (for biopsy and/or resection)  Involvement of adjacent structures.
Involvement of adjacent structures.
Fig. 10.7 Mature teratoma in a 37-year-old woman (incidental finding).
a The plain chest radiograph shows a sharply demarcated convex mass in the aortopulmonary window.
b CT also shows a smoothly demarcated lesion with focal mural calcifications and components isodense to fat and soft tissue.
Fig. 10.8 Extragonadal germ cell tumor in a 26-year-old man with chest pain.
a The plain chest radiograph shows an abnormally widened anterior upper mediastinum.
b CT visualizes the tumor as a lobular mass with inhomogeneous density and liquid components suggestive of necrosis.
Differential Diagnosis
Lymphoma | – Homogeneous solid mass – Multilocular – Often indistinguishable from a seminoma |
Thymoma or thymic tumor | – Indistinguishable from malignant germ cell tumors |
Retrosternal goiter | – Continuous with the thyroid – Higher density than muscle on CT |
Tips and Pitfalls
Except for mature teratomas, it is impossible to determine whether findings are malignant.
Selected References
Duwe BV, Sterman DH, Musani AI. Tumors of the mediastinum. Chest 2005; 128: 2893–2909
Kim JH, Goo JM, Lee HJ. Cystic tumors in the anterior mediastinum: radiologic-pathological correlation. J Comput Assist Tomogr 2003; 27: 714–723
Moeller KH, Rosado-de-Christenson ML, Templeton DA. Mediastinal mature teratoma: imaging features. AJR Am J Roentgenol 1997; 169: 985–990
Strollo DC, Rosado-de-Christenson ML, Jett JR. Primary mediastinal tumors: Part 1 Tumors of the anterior mediastinum. Chest 1997; 112: 511
Neurogenic Tumors
Definition
 Epidemiology
Epidemiology
Account for 10–20% of mediastinal masses  90% occur in the posterior mediastinum
90% occur in the posterior mediastinum  Usually benign (80%).
Usually benign (80%).
 Etiology, pathophysiology, pathogenesis
Etiology, pathophysiology, pathogenesis
Several forms are differentiated: Peripheral nerve sheath tumors (schwannomas or neurilemmomas, neurofibromas, malignant nerve sheath tumors; usually in adults)  Tumors of the sympathetic ganglia (ganglioneuromas, ganglioneuroblastomas, neuroblastomas; usually in children under 10)
Tumors of the sympathetic ganglia (ganglioneuromas, ganglioneuroblastomas, neuroblastomas; usually in children under 10)  Tumors of the para-sympathetic ganglia (very rare).
Tumors of the para-sympathetic ganglia (very rare).
Imaging Signs
 Modality of choice
Modality of choice
CT and MRI are indicated to evaluate intraspinal findings  MIBG imaging in neuroblastoma.
MIBG imaging in neuroblastoma.
 CT findings
CT findings
– Schwannoma and neurofibroma: Paravertebral, smoothly demarcated round or lobulated mass isodense to soft tissue extending over one to two intercostal spaces  Homogeneous or heterogeneous density
Homogeneous or heterogeneous density  Homogeneous, heterogeneous, or marginal enhancement
Homogeneous, heterogeneous, or marginal enhancement  In 50% of cases there is compressive excavation of the vertebrae and or ribs
In 50% of cases there is compressive excavation of the vertebrae and or ribs  Widening of the neural foramen occurs with hourglass tumors (10%)
Widening of the neural foramen occurs with hourglass tumors (10%)  Plexiform neurofibroma is a variant.
Plexiform neurofibroma is a variant.
– Ganglioneuroma and ganglioneuroblastoma: Tumor tends to be long, extending over three to five segments with broad anterolateral contact with the spine  Homogeneous or heterogeneous density (stippled calcifications may occur)
Homogeneous or heterogeneous density (stippled calcifications may occur)  Enhances moderately with contrast
Enhances moderately with contrast  Signs of malignancy include size > 5 cm, heterogeneity, local invasiveness (mediastinum or chest wall), hematogenous metastases (lung).
Signs of malignancy include size > 5 cm, heterogeneity, local invasiveness (mediastinum or chest wall), hematogenous metastases (lung).
 MRI findings
MRI findings
– Schwannoma and neurofibroma: Morphologic criteria as on CT  Low to intermediate signal intensity on T1-weighted sequences, intermediate to high signal intensity on T2-weighted sequences.
Low to intermediate signal intensity on T1-weighted sequences, intermediate to high signal intensity on T2-weighted sequences.
– Ganglioneuroma and ganglioneuroblastoma: Heterogeneous signal intensity on all sequences.
 Pathognomonic findings
Pathognomonic findings
Smoothly demarcated round or lobulated tumors in a typical paravertebral location with compressive erosion of bone  Multiple neurogenic tumors and plexi-form neurofibromas are pathognomonic for neurofibromatosis.
Multiple neurogenic tumors and plexi-form neurofibromas are pathognomonic for neurofibromatosis.
Fig. 10.9 Neurilemoma in a 48-year-old man. The plain chest radiographs show only a spherical, smoothly demarcated paravertebral mass of soft tissue density in the posterior lower mediastinum. Even without widening of the intervertebral foramen, the lesion is most likely a neurogenic tumor because of its location. The lesion was confirmed intraoperatively as a neurilemoma.
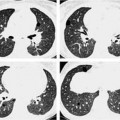
Fig. 10.10 Neurofibroma in a 38-year-old woman.
a The plain chest radiograph shows bilateral abnormal widening of the upper mediastinum primarily on the left side involving the thoracic inlet. A second tumor of soft tissue density is visualized laterally along the ribs in the left upper lung field. A local density is also visible projected on the right hilum.
b– e The CT images show the lesion in each case to be a smoothly demarcated extrapulmonary tumor homogeneously iso-dense to soft tissue without any bony destruction. Local widening of the intervertebral foramen was demonstrated only at the level of the thoracic inlet (not shown).
Clinical Aspects
 Typical presentation
Typical presentation
 Therapeutic options
Therapeutic options
Radical surgical excision  Chemotherapy and resection are indicated for neuroblastoma and ganglioneuroblastoma.
Chemotherapy and resection are indicated for neuroblastoma and ganglioneuroblastoma.
 Course and prognosis
Course and prognosis
Prognosis is good for benign tumors that are excised completely  Local recurrence is common following incomplete resection or in neurofibromatosis
Local recurrence is common following incomplete resection or in neurofibromatosis  The prognosis for malignant tumors depends on the initial findings and the opportunity for radical treatment but on the whole is quite unfavorable.
The prognosis for malignant tumors depends on the initial findings and the opportunity for radical treatment but on the whole is quite unfavorable.
 What does the clinician want to know?
What does the clinician want to know?
Involvement of the spinal canal  Determine whether findings appear malignant (local invasiveness, metastases)
Determine whether findings appear malignant (local invasiveness, metastases)  Staging in neuroblastoma and ganglioneuroblastoma:
Staging in neuroblastoma and ganglioneuroblastoma:
Stage I: | Ipsilateral, circumscribed, noninvasive |
Stage II: | Locally invasive, does not cross the midline, no lymph node metastases |
Stage III: | Crosses the midline, bilateral regional lymph node metastases |
Stage IV: | Extensive metastases |
Stage IVS: | Stage I or II tumors with metastases limited to the liver, skin, and/or bone marrow |
Differential Diagnosis
Lateral thoracic meningocele | – Isodense and isointense to CSF Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





 The majority of malignant tumors are symptomatic (pain, paresthesias, neurologic deficits)
The majority of malignant tumors are symptomatic (pain, paresthesias, neurologic deficits)  A metabolically active neuroblastoma or ganglioneuroblastoma produces catecholamines and intestinal peptides that can cause hypertension, flush symptoms, and diarrhea.
A metabolically active neuroblastoma or ganglioneuroblastoma produces catecholamines and intestinal peptides that can cause hypertension, flush symptoms, and diarrhea.