Feature
Medical thoracoscopy/pleuroscopy
VATS
Purpose
Diagnosis
Minimally invasive thoracic surgery
Pleurodesis
Location
Endoscopy suite
Operating room
Operating room
Anesthesia
Local with moderate sedation
Single-lung ventilation
Technique
Single puncture
Multiple punctures
Double puncture
Instruments
Nondisposable
Disposable
Simple
Complex
As with all technical procedures requiring special skills, there is a learning curve before full competence is achieved. Appropriate learning is therefore mandatory. The technique is actually very similar to chest-tube insertion by means of a trocar, the difference being that the thoracoscope/pleuroscope is introduced before insertion of the chest tube. Thus, the whole pleural cavity can be visualized, and biopsies can be taken from all areas of the pleural cavity, including the chest wall, diaphragm, lung, and even mediastinum. In general, MT/P is easier to learn than flexible bronchoscopy if sufficient expertise in thoracentesis and chest-tube placement has already been gained. When indicated, talc poudrage can be performed prior to chest-tube insertion, allowing a very homogeneous distribution of talc on the visceral and parietal pleura. Today, this is the gold standard for nonsurgical pleurodesis.
Historical Development
Probably the first thoracoscopy was performed as early as 1866 by Francis-Richard Cruise in Ireland. This was brought to light only recently.
However, Hans-Christian Jacobaeus in Sweden has to be regarded as the father of thoracoscopy since he introduced the technique together with laparoscopy in 1910 and made it known worldwide by many publications and lectures. Primarily, in his pioneer paper (published in German in the “Münchner Medizinische Wochenschrift,” one of the leading journals at that time), Jacobaeus used the method for diagnosis in tuberculous pleural effusions. He defined three main prerequisites which are still valid today: (1) the possibility to introduce a trocar into the relevant cavity without lacerating the inner organs and without causing too much pain, (2) introduction of a transparent medium into the cavity (Jacobaeus used filtered air for this purpose), and (3) an endoscope of such small dimensions that it can be introduced through the trocar.
But already in 1913, Jacobaeus applied the technique also for therapeutic purposes. He used it for cauterization of adhesions between the parietal and visceral pleura which prevented a complete artificial pneumothorax required for the collapse therapy of pulmonary tuberculosis. The technique, with two different points of entry under local anesthesia, called “Jacobaeus operation,” became very popular in the pre-antibiotic era for treatment of tuberculosis and was applied during the ensuing 40 years on a worldwide scale almost exclusively for this purpose.
Only with the advent of antibiotic treatment of tuberculosis in the 1950s, the therapeutic use of thoracoscopy in the treatment of tuberculosis came to an end. At the same time, other diseases became more important to the chest physician, and, consequently, a generation of physicians already familiar with the therapeutic application began to use thoracoscopy on a much broader basis for diagnostic evaluation of many pulmonary diseases, mainly in Europe. Today, MT/P is considered as an integral part of interventional pulmonology.
At the beginning of the 1990s, following the experience of abdominal surgeons with minimally invasive surgery, thoracic surgeons introduced these techniques for “surgical thoracoscopy” or “video-assisted thoracic surgery (VATS).”
To clarify the difference between the two methods, the term “medical thoracoscopy” was introduced. However, because the term “thoracoscopy” is used for both the medical and surgical procedures, a degree of uncertainty has arisen, which may lead to unnecessary surgical interventions for what are, in fact, medical indications (Table 59.2). To avoid confusion in the future, it has been suggested that the old term “pleuroscopy,” as used already in 1923, should be favored over “medical thoracoscopy,” both terms are used today in an interchangeable way.
Table 59.2
Indications for medical thoracoscopy/pleuroscopy (MT/P) versus surgical thoracoscopy (VATS) versus the middle column where both methods can be used
MT/P | MT/PorVATS | VATS |
|---|---|---|
Pleural effusions | Spontaneous pneumothorax | Lung procedures |
Pleural effusions of unknown etiology | Staging | Lung biopsy |
Staging of lung cancer | Pleurodesis by talc poudrage | Lobectomy |
Staging of diffuse malignant mesothelioma | Empyema (stage I/II) | Pneumonectomy |
Pleurodesis by talc poudrage or any other agent | Drainage | Decortication |
Diffuse pulmonary diseases | Lung volume reduction surgery | |
Localized lesions | Pleura procedures | |
Chest wall, diaphragm | Pleurectomy (pneumothorax) | |
Sympathectomy, splanchnicectomy | Drainage/decortication (empyema stage III) | |
Esophageal procedures | ||
Excision of cyst, benign tumors, esophagectomy, anti-reflux procedures, mediastinal procedures | ||
Resection of mediastinal mass | ||
Thoracic duct ligation | ||
Pericardial window | ||
Sympathectomy |
In several European countries, MT/P has already been part of the training program in respiratory medicine for many years, and it is now becoming more popular in the United States, where according to the national survey in 1994, MT/P was applied frequently by 5 % of all pulmonary physicians. Although newer data are not available, the interest in the technique seems to be increasing; however, training is lacking. In an American College of Chest Physicians (ACCP) survey of US pulmonary/critical care fellowship programs in 2002/2003, only 12 % of the directors stated that MT/P was offered in their programs. In the United Kingdom, where medical thoracoscopy was underutilized compared with the rest of Europe, there is also growing interest. Meanwhile, the technique has been introduced successfully in Australia, as in many Asian, South American, and some African countries.
Techniques
The modern principles and techniques of MT/P using rigid instrumentation were developed in continental Europe during the second half of the last century. These principles remain valid for use of the newer generation of semirigid (semiflexible) pleuroscopes, too.
Pulmonologists nowadays use two different techniques for performance of diagnostic and therapeutic thoracoscopy. One method recommends a single entry site, the use of a usually 9-mm rigid thoracoscope (or of a semirigid/semiflexible 7-mm pleuroscope) with a working channel for accessory instruments and optical biopsy forceps, and is most often performed under local anesthesia. The other method requires two entry sites – one for a 7-mm trocar for the examination telescope and the other for a 5-mm trocar for accessory instruments, including the biopsy forceps – and is usually performed with conscious sedation or general anesthesia. As with all technical procedures, there is a learning curve before full competence is achieved. Since the technique is actually very similar to chest-tube insertion by means of a trocar, sufficient expertise in thoracentesis and chest-tube placement is mandatory. The difference to the latter is only that with MT/P, the pleural cavity can be visualized and biopsies can be taken from all areas of the pleural cavity, including the chest wall, diaphragm, mediastinum, and lung, under direct visual control. When indicated, talc poudrage can be performed additionally.
For most indications, MT/P will start as a single-port, single-instrument rigid procedure, as first described by Jacobaeus for diagnostic purposes. However, with the introduction of the semirigid/semiflexible pleuroscope, which is similar in design, accessory equipment, and handling to the flexible bronchoscope, MT/P can now be performed in a fashion analogous to flexible bronchoscopy. Thus, this technique is now increasingly used by pulmonologists who are experienced with video-controlled flexible bronchoscopy.
Equipment
Since the first detailed description by Jacobaeus in 1910, rigid endoscopic instruments such as stainless-steel trocars and endoscopes have been pivotal in the performance of thoracoscopy (and VATS). With the introduction of the semirigid/semiflexible pleuroscope, similar in design and handling to the flexible bronchoscope, pleuroscopy is now frequently performed with this technique. An additional advantage is that parts of the bronchoscopy equipment (e.g., the light source, processor, and monitor) can be used, reducing the acquisition costs.
The equipment requirements include trocar, thoracoscope/pleuroscope, biopsy forceps, unipolar coagulation forceps, light sources, video system, aspiration system, talc, chest tubes, and drainage systems. The usual diameter of the rigid thoracoscope is 7–9 mm, that of the semirigid pleuroscope 7 mm. For the rigid technique, optical devices exist with various fields of view (0, 30, and 90 °); trocars are also available with diameters of 5 and 3.75 mm for performing thoracoscopy in children. The trocar consists of an obturator and cannula with a blunt conical tip, adjacent to which there is a small hole connected to the trocar lumen, open to the exterior, so that penetration into the pleural cavity is signaled. Unlike the instruments for laparoscopy, this trocar does not have to be airtight. Air should be allowed to enter and leave the thoracic cavity freely. Examination will be limited by pain if the diameter of the trocar is larger than 10 mm.
Figure 59.1 shows a selection of rigid thoracoscopy instruments (Fig. 59.1). Besides the biopsy forceps, needle biopsy, and suction catheter, the working channel also accommodates electrocautery. A bajonet optical system with an instrumentation channel and the appropriate instruments may facilitate direct fluid suction, electrocautery, or direct insufflation of talc. A Xenon light source satisfies the requirements for high-quality visual exploration and video documentation. The inspection of the pleural space can be performed either directly through the telescope or indirectly by video (Figs. 59.2 and 59.3). Today, most – if not all – centers use video systems.
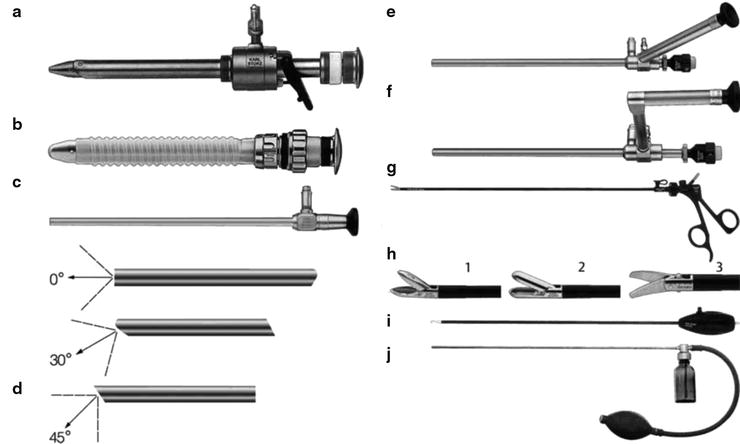


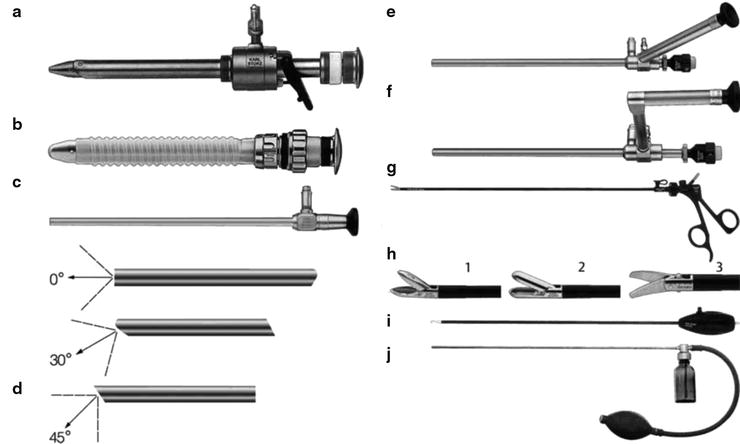
Fig. 59.1
Selection of instruments for rigid medical thoracoscopy. (a) Trocar with multifunctional valve with insufflation stopcock, 11 mm, autoclavable. (b) Trocar with silicone leaflet valve, 11 mm, autoclavable. (c) Telescope, particularly suited for single-incision thoracoscopy, here with light shaft for photography, diameter 10 mm, length 31 cm, trocar size 11 mm. (d) Various fields of view. (1) Straightforward telescope 0 °, diameter 10 mm, length 31 cm, autoclavable; (2) Forward-oblique telescope 30 °, diameter 10 mm, length 31 cm, autoclavable; (3) Telescope 45 °, diameter 10 mm, length 31 cm, autoclavable. (e) Straightforward telescope 0 ° with angled eyepiece, diameter 10 mm, working length 27 cm, with instrument channel 6 mm, trocar size 11 mm, single puncture. (f) Straight-forward telescope 0 °, with parallel eyepiece (bayonet optic), diameter 10 mm, working length 27 cm, with instrument channel 6 mm, trocar size 11 mm, single puncture. (g) Dissecting and biopsy forceps, rotational, that can be dismantled, with connector pin for unipolar coagulation, 5 mm. (h) Single-action jaws: (1) dissecting and biopsy forceps: (2) biopsy forceps; (3) scissors. (i) Dissecting electrodes, with connector pin for unipolar coagulaton, L-shaped, size 5 mm, working length 43 cm. ( j) Powder blower, with rubber bulb, size 5 mm, working length 42 cm (Reprinted with kind permission from Karl Storz GmbH & Co. KG, Tuttlingen, Germany)

Fig. 59.2
Direct inspection through the rigid thoracoscope (while taking a biopsy) (Reprinted with permission from Loddenkemper R, Mathur PN, Noppen M, Lee P. Medical thoracoscopy/pleuroscopy: manual and atlas. Stuttgart: Thieme; 2010)

Fig. 59.3
Indirect, video-controlled inspection of the pleural cavity through the semiflexible pleuroscope (Reprinted with permission from Loddenkemper R, Mathur PN, Noppen M, Lee P. Medical thoracoscopy/pleuroscopy: manual and atlas. Stuttgart: Thieme; 2010)
Rigid mini-thoracoscopes were recently introduced, but they have the disadvantage that a second point of entry is necessary for biopsy purposes, and insertion of a large drainage catheter through the same channel post-thoracoscopy is impossible. The semirigid/semiflexible pleuroscope has been developed by the Japanese company Olympus in conjunction with pulmonologists for a single-puncture technique. The pleuroscope consists of a handle that is similar to the standard flexible bronchoscope and a shaft that measures 7 mm in outer diameter and 27 cm in length (Fig. 59.4a–c). The shaft is made up of two sections: a 22-cm proximal rigid portion and a 5-cm flexible distal end. The flexible tip is movable by a lever on the handle, which allows a two-way angulation capability of 160 ° up and 130 ° down. It also has a 2.8-mm working channel that accommodates biopsy forceps, needles, and other accessories and is compatible with various electrosurgical and laser procedures (Fig. 59.5). The instrument is used with a single-port technique with a disposable 8-mm inner diameter flexible trocar (Figs. 59.6 and 59.7). The new LTF 160 model allows autoclaving, thereby obviating important questions and issues related to sepsis (Fig. 59.8a, b). The other notable advantage of the semirigid pleuroscope over rigid instruments is that it interfaces easily with existing processors and light sources made by the manufacturer for flexible bronchoscopy or gastrointestinal endoscopes, which are available in most endoscopy units without additional costs (Fig. 59.9).
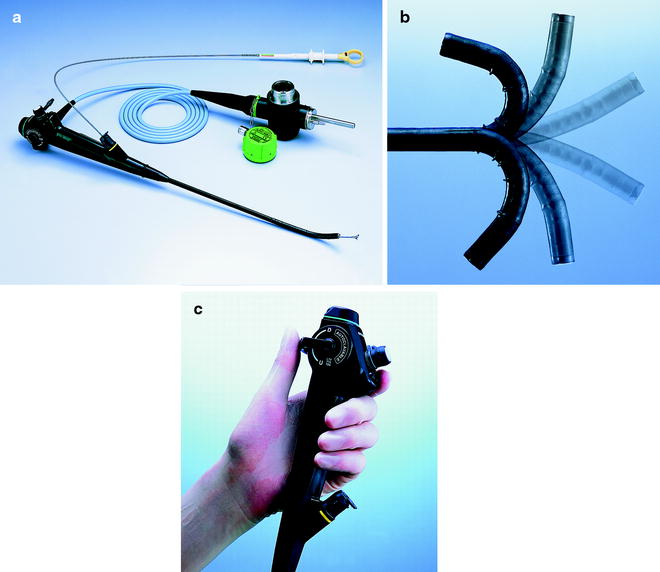


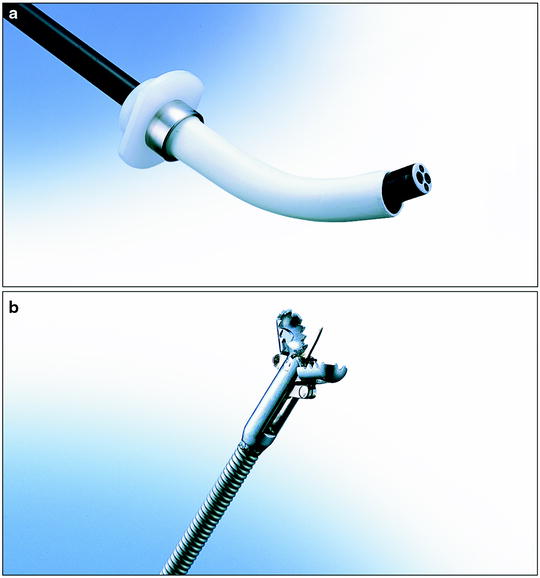


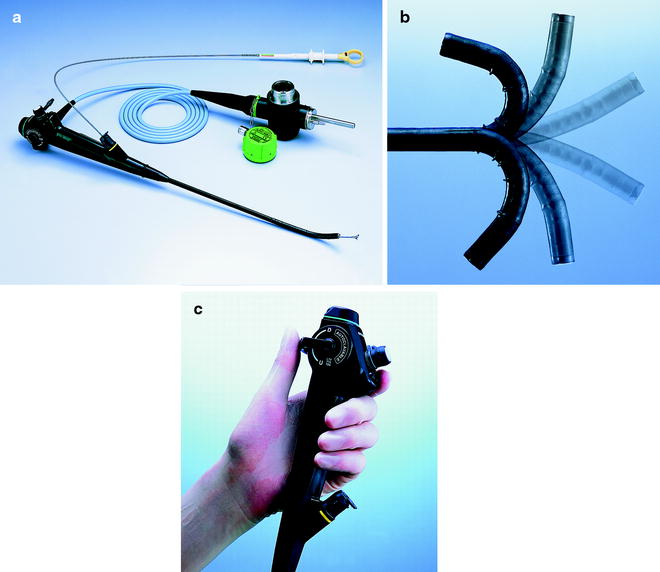
Fig. 59.4
(a) The semirigid (semiflexible) pleuroscope (Olympus Corporation). Control section allows handling as with the flexible bronchoscope. (b) Angulation capability 160 ° upward/130 ° downward. (c) Diameter of the pleuroscope 7-mm, with a 2.8-mm diameter of the working channel (Reprinted with kind permission from Olympus Corporation)

Fig. 59.5
Additional accessories for electrosurgical and laser procedures that can be introduced through the semirigid (semiflexible) pleuroscope. (a) Spray catheter. (b) (left to right) Coagulation electrode, hot biopsy forceps, electrosurgical knife ((a) and (b) reprinted with kind permission from Olympus Corporation)

Fig. 59.6
Rigid trocar and cannula with valve for the semiflexible pleuroscope (Olympus). Outer diameter 10 mm, inner diameter 8 mm
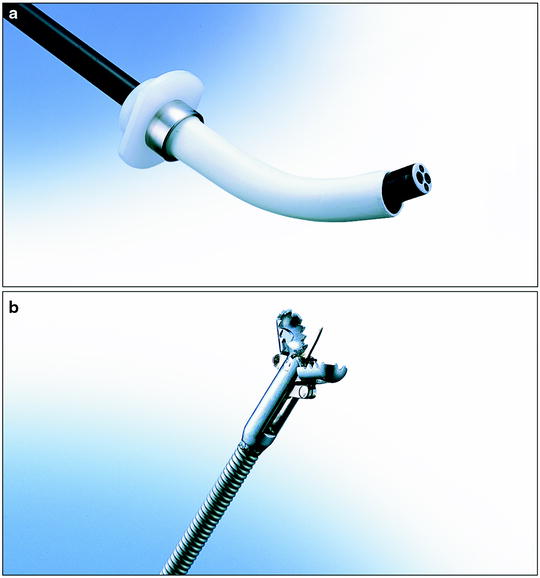
Fig. 59.7
(a) Pleuroscope with the flexible forceps, introduced through the trocar shaft. (b) Swing-jaw needle forceps (alligator jaw type) (Reprinted with kind permission from Olympus Corporation)

Fig. 59.8
(a) A dedicated, green waterproof cap protects the electrical connections of the LTF 160 pleuroscope during autoclaving. (b) Waterproof control section (Reprinted with kind permission from Olympus Corporation)

Fig. 59.9
Light source, processor, and monitor used with the bronchovideoscope (Reprinted with kind permission from Olympus Corporation)
Comparison of the Rigid and Semirigid Technique
Advantages of the rigid thoracoscopic instruments are, besides larger biopsy sizes, that the rigid forceps allows taking of biopsies from very dense lesions, too. The rigid instruments are also more suitable when more elaborate procedures are indicated or when it is necessary to control hemorrhage after biopsy. Rigid instruments are less expensive, more robust, have a longer endurance, and may need maintenance and repair less often (Tables 59.3 and 59.4).
Table 59.3
Advantages of rigid medical thoracoscopy
Trocar with multifunctional valve |
Larger biopsy specimens |
Biopsies from dense lesions easier to take |
More suitable for elaborate procedures, extensive adhesiolysis, lung biopsies, sympathicolysis, etc. |
Less expensive, more robust, and less maintenance and repair cost |
Table 59.4
Advantages of semiflexible pleuroscopy
“Look and feel” of a flexible bronchoscope (lower threshold for the chest physician) |
Interfaces easily with existing processors and light sources for flexible bronchoscopy/GI endoscopy (without additional cost) |
Allows better view by maneuvering the flexible tip into different directions and around adhesions |
Flexible tip facilitates homogeneous insufflation of talc (talc poudrage) |
The advantage of the semirigid pleuroscope is that it has the “look and feel” of a flexible bronchoscope, and thus may “lower the threshold” for MT/P for the pulmonologist. It may also be helpful psychologically in overcoming fear of using the rigid (and therefore often regarded as more dangerous) instruments. In addition, it helps maintain a clear optical field by allowing concurrent suctioning, which is analogous to the suction techniques used during flexible bronchoscopy, and it may allow one to overcome a limited view by maneuvering its flexible tip in different directions and around adhesions. Its flexible tip facilitates the homogeneous insufflation of talc (via a catheter), introduced through the working channel, into all areas of the parietal and visceral pleura.
The ideal is certainly the combination of both techniques, in which rigid MT can be complemented by the semiflexible pleuroscope in the above-mentioned advantageous situations, which is comparable to the combined use of rigid and flexible bronchoscopy in complex therapeutic endobronchial indications.
MT/P can be performed in the operating room or in an environment dedicated to invasive procedures such as a clean endoscopy room. The personnel required to perform endoscopy include an endoscopy nurse (or an endoscopy assistant) to assist with the instrumentation, an additional assistant outside the sterile field to bring necessary equipment, and the physician performing MT/P. Ideally, an additional person sits at the patient’s head and monitors his or her overall condition. In an emergency, MT/P can be performed with only a physician and a nurse, but this is less efficient and prolongs the procedure.
The procedure suite should be equipped with monopolar and, if possible, bipolar electrocoagulation as well as equipment for resuscitation, assisted ventilation, electrocardiography, and blood pressure monitoring and a defibrillator, as well as an oxygen source and a pulse oximetry system.
Knowledge and Skills Required for MT/P
To learn MT/P, the pulmonologist needs to know the exact topographical anatomy of the thorax, the pathophysiology and pathology of respiratory diseases, their diagnostic approach and their management options, in particular of pleural diseases, as well as the clinical prerequisites, the contraindications, and the potential complications of the technique. He or she must also know the details of the technique of MT/P including all instruments used, the different options of access to the pleural space, the technique of coagulation, and so on, as outlined later. In addition, he or she should already have adopted certain skills in the diagnosis and treatment of respiratory diseases, particularly pleural diseases.
The learner should already have acquired skills in the following: application of the above knowledge, diagnostic and therapeutic thoracentesis, performance of local anesthesia, closed needle biopsy of the pleura, familiarity with chest tubes and pleural drainage, closed chest-tube insertion, pleurodesis techniques, flexible bronchoscopy, rigid bronchoscopy (optional), use of either the semirigid pleuroscope or the rigid thoracoscope (or both), use of biopsy forceps and other instruments, use of coagulation systems, use of the talc atomizer/talc spray, use of video-endoscopic equipment, ultrasonography, and/or fluoroscopy (optional).
Technical skills are best learned under the direct supervision of an experienced thoracoscopist. Because manual dexterity, confidence, and expertise may vary from one physician to another, it is difficult to specify a minimum number of procedures necessary to obtain the skill or to maintain competence. It is unlikely that any specific number of procedures will guarantee competence. However, a minimum number of 20 procedures are desirable to achieve sufficient familiarity with the instrumentation and interpretation of normal and pathological thoracoscopic findings. Procedural competence can probably be maintained if about 10–20 thoracoscopies are performed yearly.
Adequate training in both the cognitive and technical aspects of MT/P is essential. This is unlikely to be provided by a single 2-day course. Training courses should be encouraged and may be extremely beneficial if they follow certain guidelines and include didactic lectures as well as laboratory sessions. By attending hands-on training seminars, lectures, and symposia, physicians can learn basic concepts and acquire a greater understanding of the appropriate indications, risks, benefits, and limitations of MT/P. These sessions should allow physicians to achieve familiarity and comfort with basic thoracoscopic/pleuroscopic techniques and instrumentation. Physicians should be encouraged to work with a mentor within their community until the necessary criteria are met for MT/P privileges within their own institutions. This form of a mini-fellowship may be ideal for training physicians in procedures not learned during formal subspecialty training. A good opportunity to learn inspection of the pleural space and its pathological situation is given by observation of procedures on a video screen or live transmission into a bigger group. Also, manuals describing in detail the technique including the demonstration of endoscopic photos will be helpful. As with all technical procedures, there is a learning curve before full competence in MT/P is achieved, although it is easier to learn than flexible bronchoscopy. The recommendation for beginners is to start with easy situations such as a large pleural effusion or a pneumothorax when placement of a chest tube is indicated.
Point of Entry
The point of entry is generally near the mid-axillary line, within the axillary triangle. The axillary triangle has no large muscle obstructing passage of the instruments: it is bordered anteriorly by the lower edge of the pectoralis major muscle, posteriorly by the anterior edge of the latissimus dorsi muscle, and inferiorly at the level of the diaphragmatic insertions. Its apex reaches the second intercostal space. The final location of the insertion port will be determined by the indication: for pleural effusions most commonly in the fifth, sixth, or seventh intercostal space. The last two spaces are especially preferred when metastatic tumor and diffuse malignant mesothelioma are suspected to reach the most common sites of these malignancies. This provides an excellent view of both the diaphragm and the costovertebral gutter where malignant lesions, if present, will usually be reachable.
In case of spontaneous pneumothorax, the entry port will be located at the third or fourth intercostal space to allow thorough inspection of the lung apex and because the leak, if present, is usually in the upper lobe.
In different indications, other points of entry are used depending on the clinical setting and/or the chest radiography/CT or ultrasound results.
Access to the Pleural Space
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree