Synovial Abnormalities
Infectious Synovitis
The general diagnostic considerations for the MRI diagnosis of septic arthritis have been discussed earlier in this book. Suffice it to say that the distinction between infectious and noninfectious synovitis can be challenging both clinically and with MRI. Historically, clinical presentation and fluid sampling have been the gold standard for the diagnosis of septic arthritis or infectious tenosynovitis. This is particularly problematic in the small joints of the hands, in which joint effusions have been shown to be small or absent in a significant number of cases (1). This may be the result of a lack of compliance in the joint capsule, which in turn results in decompression of joint fluid into the periarticular soft tissues. Infectious synovitis in the hand, although not exceedingly common, is encountered in specific situations and associated with specific pathologic entities.
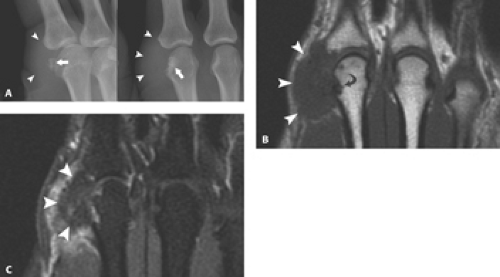
Common causes for acute septic arthritis in the finger include neglected punctiform inoculation or an adjacent infection such as a subcutaneous felon (2). Perhaps the most notorious cause of the infected hand is the clenched fist injury to the mouth, known as the “fight bite.” The closed fist injury results from the patient’s practice of striking another individual in the mouth region with the fist. Such blunt impact on the aggressor’s hand can produce both a soft tissue and an osseous injury. Although the osseous injury can be readily apparent on plain film, the presence of a fight bite injury can be much more subtle. The teeth of the victim generally produce a small laceration over the dorsal metacarpophalangeal joint that appears innocuous. After contact is made, the patient is likely to extend the hand, creating a deep inoculum of oral bacteria into the wound, which can involve the periarticular soft tissues, the joint space, and even the bone (3, 4). These fight bite wounds have the highest incidence of complications of any closed fist injury and of any type of bite wound. Their occurrence over the third through fifth metacarpophalangeal joints makes this injury susceptible to deep infection because there is little overlying soft tissue to protect the underlying articulation (Fig. 20.1).
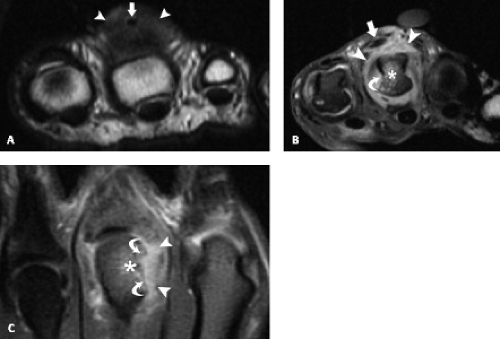
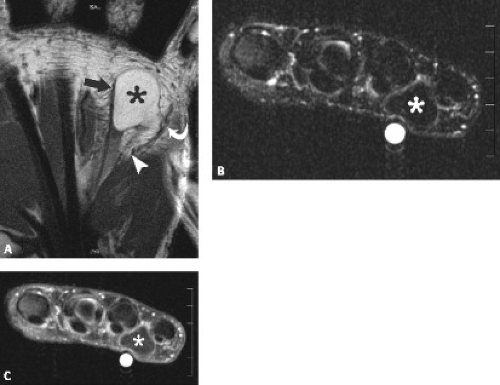
Another infection that is classically associated with the fingers and hands is that of Mycobacterium marinum, the most common atypical mycobacterial species to occur in the upper extremity. This is an unusual atypical mycobacterial infection that occurs in immune-competent hosts, usually after exposure to contaminated water. It is associated with cutaneous lesions, but deeper infection can cause tenosynovitis and septic arthritis (5– 7). The first case of infection was contracted from a fish tank, although other documented causes of infection include occupational and leisure activities in water with infection requiring breakdown of skin integrity through a lesion such as an abrasion or laceration (5, 8). There are no pathognomonic clinical features of this entity. Initially, skin lesions in the form of noncaseating granulomas appear. Infections have been divided into three types: Type I representing superficial, self-limiting infection; Type II with single or multiple granulomas; and Type III with deeper infection involving the underlying bone, joint, and soft tissues (7, 9, 10). Imaging is nonspecific in the early stages. Even in the later stages of the disease, the imaging findings of exuberant tenosynovitis are nonspecific (Fig. 20.2). The tendons appear intrinsically normal, the striking feature being the abundant fluid distending the tendon sheath. In one case, rice bodies were identified within the distended tendon sheath (11). As previously noted, osseous and articular involvement may also occur, but imaging findings are nonspecific.
Noninfectious Synovitis
Rheumatoid Arthritis
As noted previously, the wrist, metacarpophalangeal joints, and proximal interphalangeal joints comprise the sites most commonly involved in the presentation of rheumatoid arthritis. The role and technical considerations of MRI in the assessment of nonspecific synovial inflammatory processes, specifically its usefulness for evaluation and identification of synovial inflammation and hypertrophy, bone marrow edema, osseous erosions, have been discussed previously in this book (“Miscellaneous Conditions of the Elbow”). The specific literature and data applying to MRI of the hands are reviewed.
In the case of rheumatoid arthritis, increasing attention has been focused on the use of MRI for diagnosis, prognostication, and monitoring of disease progression and response to therapy. It has been suggested that incorporation of MRI signs of synovitis into the diagnostic criteria for rheumatoid arthritis would not only increase diagnostic accuracy, but lead to a diagnosis earlier in the course of the disease (12). Moreover, many believe that MRI may provide the most sensitive means of identifying rheumatoid arthritis at its earliest stages (13–16).
Radiography has served as the primary method for both the diagnosis and follow up of patients with rheumatoid arthritis. The earliest radiographic signs of rheumatoid arthritis include soft tissue swelling and periarticular osteopenia. These findings are followed by the hallmark of this disease process, marginal erosions. The finding of bilateral, symmetric wrist and proximal
hand erosive disease comprises one of the early diagnostic criteria for rheumatoid arthritis, distinguishing it from other forms of peripheral synovial inflammatory arthropathies. Because the majority of damage occurs early in the course of rheumatoid arthritis, much interest has focused on earlier detection of joint inflammation and erosions as well as more rapid assessment of therapeutic response to disease modifying antirheumatic drugs.
hand erosive disease comprises one of the early diagnostic criteria for rheumatoid arthritis, distinguishing it from other forms of peripheral synovial inflammatory arthropathies. Because the majority of damage occurs early in the course of rheumatoid arthritis, much interest has focused on earlier detection of joint inflammation and erosions as well as more rapid assessment of therapeutic response to disease modifying antirheumatic drugs.
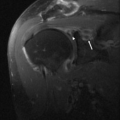
Although multiple imaging methods have been explored with regard to the early detection of rheumatoid arthritis, MRI has emerged as the most sensitive modality for the early detection of synovitis and erosive disease (17). Inflamed synovium is seen on MR images as increased soft tissue mass in the region of the capsule (Fig. 20.3). The signal characteristics are intermediate on T1-weighted images and heterogeneously increased on T2-weighted images. As a result of the hyperemia and neovascularity of the proliferative synovium, it avidly enhances after contrast administration (Fig. 20.4). In addition to its diagnosis, synovial inflammation can be quantified and graded by MRI imaging (18). Ostergaard et al. (19) found that synovial volumes as determined by MRI were closely related to the progression of joint disease and concluded that quantitative MRI may prove valuable as both a marker of joint disease and as a predictor of joint destruction in rheumatoid arthritis.
MRI is also the most sensitive imaging method to detect erosions. McQueen et al. (15) reported that carpal erosions could be detected in patients on MR images 4 months after the onset of symptoms, whereas only 15% of patients had erosions on plain radiographs. Other studies have documented that erosions may be detected 1 to 5 years earlier by MRI than by plain film (20). Erosions are best identified on T1-weighted and other fat-sensitive sequences because the contrast between the high-signal–intensity marrow and the intermediate-signal–intensity proliferative synovium is optimized. The definition of erosions by MRI shows some variability in the literature. Most studies agree on the criteria of the ability to identify the abnormality in two imaging planes, one of which must establish cortical discontinuity (Fig. 20.5) (15, 20). In the small joints of the hand, assessment of cortical discontinuity may be difficult as a result of limitations of spatial resolution and partial volume effects. Typically the erosive changes encountered in the hands favor the radial aspect of the metacarpophalangeal joints with the third and fourth most commonly involved (21).
More recently, changes in bone marrow edema have been implicated as a possible precursor to the erosion. There is a growing body of literature that supports the theory of a three-step evolution of rheumatoid arthritis that progresses from synovitis to bone marrow edema with the ultimate development of erosive change (22). Indeed, the literature has shown that the ultimate development of erosions in a rheumatoid population was frequently preceded by bone marrow edema (23). Like bone erosions, bone marrow edema appears low in signal intensity on T1-weighted images and high signal on
T2-weighted images. Unlike erosions, however, no cortical break can be identified.
T2-weighted images. Unlike erosions, however, no cortical break can be identified.
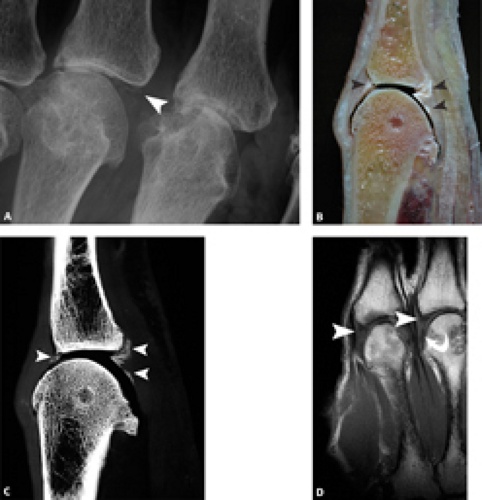
Gout
Gout is a rheumatologic disorder resulting from a metabolic imbalance characterized by episodic attacks of synovial inflammation with the development of characteristic erosive changes as well as articular and periarticular soft tissue calcifications. Untreated gout passes through four stages: (i) asymptomatic hyperuricemia; (ii) acute gouty arthritis; (iii) intercritical gout; and (iv) tophaceous gout. Asymptomatic hyperuricemia is the term for an elevated serum urate level without gouty arthritis. Hyperuricemia is defined as a serum urate concentration greater than 7 mg/dL. Usually this phase lasts over 20 years, and most people with hyperuricemia remain asymptomatic throughout their lifetime. No physical manifestation of gout occurs until the conclusion of this stage heralded by the first attack of gouty arthritis. This is generally monoarticular in nature and commonly affects the first metatarsal phalangeal joint. In an acute attack, the physical examination as well as MRI findings are those of nonspecific synovitis. With repeated attacks, the development of erosive changes with the classic morphology of the overhanging edge occurs in conjunction with soft tissue calcification, the so-called tophus. The most common locations for tophi include the joints of the feet or hands. Articular tophaceous gout results in a destructive arthropathy caused by deposition of urate crystals in the joints and surrounding soft tissues.
MRI is not routinely used for the evaluation of gout; however, this disease process has been referred to as “the great deceiver” in that it can mimic infection or neoplasm. Characteristically, tophi have signal intensity isointense to skeletal muscle on T1-weighted images (Fig. 20.6). On T2-weighted images, the signal characteristics vary from high signal intensity to homogeneous low signal intensity (24–28). Hemosiderin deposition has also been reported within a tophus (27). The pattern of enhancement is variable from intense and homogeneous
to peripheral and heterogeneous (26). Although the MR appearance of tophus is nonspecific, the diagnosis of gout should be entertained whenever a mass has heterogeneous low to intermediate signal intensity on T2-weighted images, especially in the presence of adjacent osseous erosion (28). MRI can also demonstrate extra-articular deposition of monosodium urate in bones, tendons, and bursae (29–32).
to peripheral and heterogeneous (26). Although the MR appearance of tophus is nonspecific, the diagnosis of gout should be entertained whenever a mass has heterogeneous low to intermediate signal intensity on T2-weighted images, especially in the presence of adjacent osseous erosion (28). MRI can also demonstrate extra-articular deposition of monosodium urate in bones, tendons, and bursae (29–32).
Calcium Pyrophosphate Crystal Deposition
Calcium pyrophosphate dihydrate (CPPD) crystal deposition is a rheumatologic disease initially characterized by the occurrence of intermittent episodes of synovial inflammation, so-called “pseudogout” attacks. Based on its etiology, it has been classified as idiopathic, hereditary, and secondary (33–35). The idiopathic form is the most common with surveys indicating 7% of the adult population has CPPD crystal deposits at the age of 70 years (36).
In the pathogenesis of CPPD crystal deposition disease, chondrocyte alteration in the midzonal region occurs resulting in disruption of the extracellular matrix. As a result of the matrix alteration, calcium pyrophosphate crystals form adjacent to chondrocytes. Crystals shed into the joint can elicit an acute synovial inflammatory response, which can, in turn, lead to periarticular soft tissue inflammation (37).
Clinical manifestations of CPPD crystal deposition disease are quite varied. Asymptomatic chondrocalcinosis of the articular cartilage may be the most common form (38). This pattern is rare before the age of 50 years and commonly involves the triangular fibrocartilage of the wrist as well as the knee, symphysis pubis, and intervertebral discs. CPPD crystal arthropathy includes five distinct patterns: pseudogout (18%), pseudo-osteoarthritis with synovitis (40%), pseudo-osteoarthritis without synovitis (18%), monoarthropathy (16%), and pseudorheumatoid arthritis (8%) (33, 39). Of these, the hands are target regions in pseudo-osteoarthritis as well as pseudorheumatoid arthritis. In the hand, there is a predilection to involve the second and third metacarpophalangeal joints with cartilage loss, sclerosis, and squaring of the metacarpal heads resulting from subchondral collapse. Although a predominance of subchondral cysts can be encountered in this disease process, erosive changes are not characteristic. It is the bilateral and symmetric pattern of joint degeneration associated with CPPD crystal deposits that is distinctive (33).
During acute attacks, the MRI findings are simply that of a nonspecific synovial inflammation. In some cases, calcium pyrophosphate dihydrate crystal accumulation can lead to masses of low signal intensity on both T1-weighted and fluid-sensitive sequences. Variable enhancement is seen after the intravenous administration of contrast material. When calcifications occur in intra-articular soft tissues such as meniscus, labrum, or ligamentous structures, they can be easily overlooked on MRI because they are low in signal intensity on all sequences like the tissue in which they reside (Fig. 20.7) (33). In some cases in the meniscus of the knee, however, regions of crystal deposition may produce intermediate signal intensity that can simulate meniscal pathology (40). There are conflicting reports in the literature regarding the efficacy of MRI for the detection of chondrocalcinosis (41, 42). One study advocates the use of three-dimensional fat-saturated gradient imaging sequences for the detection of chondrocalcinosis in the knee (42). In this study, regions of calcification within the cartilage were identified as hypointense foci, in some cases with a surrounding halo of hyperintensity. In cases with surgical correlation, MRI demonstrated more diffuse involvement of the articular cartilage than did corresponding radiographs. The usefulness of MRI for the detection of chondrocalcinosis in the hands has not been
addressed in the literature but may prove challenging as a result of the thin cartilage covering involving these small articulations.
addressed in the literature but may prove challenging as a result of the thin cartilage covering involving these small articulations.
Calcium Hydroxyapatite Deposition
Hydroxyapatite crystal deposition disease (HADD) is a well-recognized disease of unknown etiology that is caused by para-articular and/or intra-articular deposition of hydroxyapatite crystals. Hereditary, traumatic, metabolic, neurologic, degenerative, and vascular factors have all been suggested as possible causes (43, 44). To this end, soft tissue calcifications can be classified by potential etiology or by radiographic appearance. Because the shoulder is the most common site of
involvement for HADD, classification systems for both its clinical and radiographic expression have been described in this articulation.
involvement for HADD, classification systems for both its clinical and radiographic expression have been described in this articulation.
Depalma and Kruper (45) distinguished two morphologic types of calcification about the shoulder based on radiographic observation. These included Type I, fluffy and amorphous, and Type II, defined and homogenous. Type I deposits are indicative of the acute stages of the disease, in which the calcific material may be liquid (consistency of milk) to semiliquid (consistency of toothpaste). In the acute stage of disease, reduction of pain and aspiration of the calcification have been advocated. Type II deposits are associated with subacute or chronic disease, the calcific material forming a dry, dense powder. In this stage of the disease, pain management as well as local injection with or without steroid have been considered standard therapy (45–47).
Although the shoulder is the most commonly involved joint in HADD, any articulation in the body can be affected. Calcifications resulting from HADD have
been reported in various tendons about the hand and wrist. The flexor carpi ulnaris tendon is a common site of involvement (44).
been reported in various tendons about the hand and wrist. The flexor carpi ulnaris tendon is a common site of involvement (44).
On MRI, the calcification will appear low signal intensity on all imaging sequences. The synovitis provoked by this disease process is nonspecific in nature and can involve tendon sheaths, bursae, or articular synovium. It can incite an intense inflammatory response in tendon sheath, bursa, or articular structures, in some cases even resulting in erosion of bone and bone marrow edema (48–51).
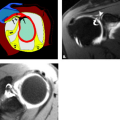
In addition to simple HADD, hydroxyapatite crystal deposition can result in a crystal-induced arthropathy similar to the urate arthropathy in gout and calcium pyrophosphate arthropathy in CPPD (Fig. 20.8). Hydroxyapatite crystals within a joint can cause synovitis that can lead to joint destruction over time. Hydroxyapatite arthropathy is most often seen in elderly women but can occur in either sex at any age. Like with HADD, the etiology of this arthropathy is unknown. Any joint can be involved, although the shoulder is the most commonly affected (52).
Tumors and Tumor-like Disorders of Synovium
Giant Cell Tumor of Tendon Sheath
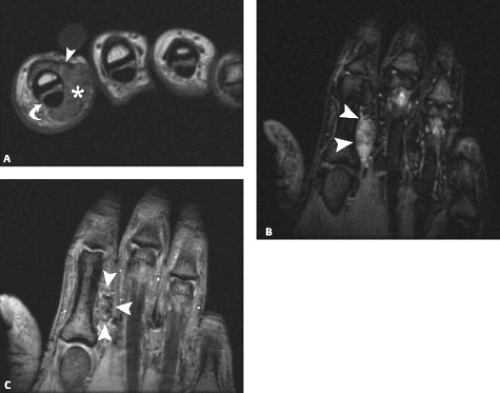
Giant cell tumor of the tendon sheath has been reported to be the second most common tumor of the hand. Despite the relative frequency with which this entity is encountered, debate exists regarding its nomenclature, pathogenesis, and classification. Different names have been used to describe this lesion, including giant cell tumor of the tendon sheath, pigmented villonodular synovitis, fibrous xanthoma, benign synovioma, and sclerosing hemangioma (53). It has been suggested that the lesion may be neoplastic, inflammatory, trauma-induced, immune-mediated, or associated with abnormal lipid metabolism (54–57). The initial classification system described a localized nodular type commonly seen in the hand and a diffuse type seen in large joints such as the knee (58). An extended classification system of hand lesions has been presented in the literature based primarily on the operative and histologic findings in 43 consecutive patients with giant cell tumors of the tendon sheath in the hand. In this classification system, a Type I lesion was surrounded by a pseudocapsule and was further characterized by the following: (a) a single nodule with a thick whitish capsule; (b) a single nodule with a thin capsule; and (c) multilobulated lesions surrounded by a common pseudocapsule. Type II lesions were not surrounded by a pseudocapsule and were further characterized by the following: (a) one main nodule accompanied by separate satellite lesions within the same anatomic area; (b) diffuse involvement with multiple granular-like lesions; and (c) multicentric with separate discrete lesions in the same digit (53). Type II tumors were found to have a higher rate of recurrence after excision. Other factors affecting the recurrence rate included poor surgical technique or incomplete excision and osseous invasion by the tumor, cellularity, and mitotic activity on histologic examination.
Clinically, giant cell tumor of the tendon sheath manifests as a slowly growing nodular mass without fixation to the overlying skin. It is attached instead to the tendon sheath or the joint capsule. Affected tendons may be partially or completely enveloped by the mass (59, 60).
Macroscopically, giant cell tumor of the tendon sheath has been described as a rubbery, nodular or multinodular mass that may be surrounded by a pseudocapsule (61).
On microscopic examination, the lesions present as a well-defined lobulated lesion. They consist of a variable amount of histiocytic mononuclear cells, multinucleated giant cells, xanthoma cells, and collagenous strands. Xanthoma cells often contain hemosiderin granules (59, 62, 63). Lesions demonstrate varying degrees of fibrosis (collagenized stroma) and cellularity, generally with an inversely proportional relationship (53). It is characteristically hypervascular.
On microscopic examination, the lesions present as a well-defined lobulated lesion. They consist of a variable amount of histiocytic mononuclear cells, multinucleated giant cells, xanthoma cells, and collagenous strands. Xanthoma cells often contain hemosiderin granules (59, 62, 63). Lesions demonstrate varying degrees of fibrosis (collagenized stroma) and cellularity, generally with an inversely proportional relationship (53). It is characteristically hypervascular.
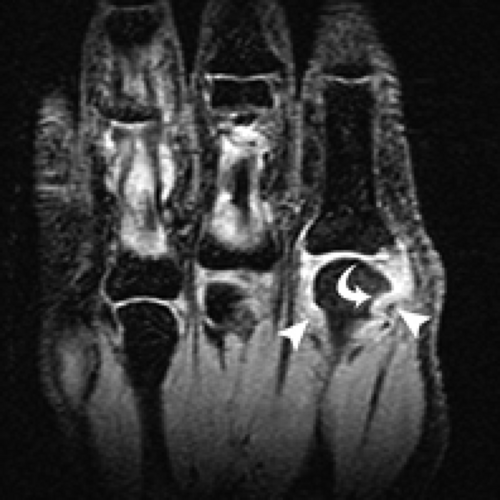
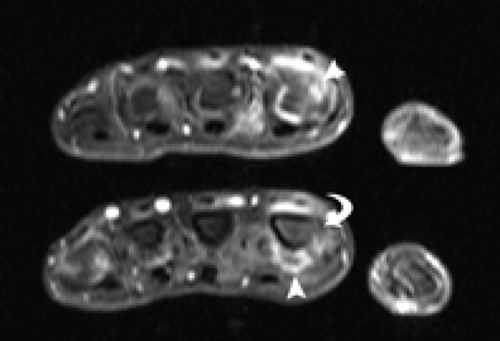
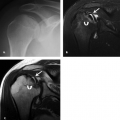
The MRI features of giant cell tumor of the tendon sheath reflect the underlying histologic composition. It is seen as a round or oval solid mass that is eccentrically located partially or completely enveloping the tendon (Fig. 20.9). These lesions may demonstrate mass effect on adjacent bone in the form of periosteal scalloping and have been reported to erode into adjacent bone in rare cases (64). The signal characteristics include homogeneous predominantly low signal intensity on T1- and T2-weighted images (isointense to muscle), although heterogeneous signal intensity on T2-weighted images has been described. In rare cases, atypical increased signal intensity can be encountered in a giant cell tumor of the tendon sheath, creating a diagnostic dilemma. In most cases, however, the diagnosis of giant cell tumor can be suggested based on the identification of hemosiderin within the lesion. Hemosiderin deposition, which shortens T2 relaxation time as a result of magnetic susceptibility effect, and abundant collagenous proliferation are responsible for the characteristically low signal intensity (60, 63, 65–68). The presence of hemosiderin becomes more prominent with increasing echo times and can cause the “blooming” artifact to be present on gradient echo sequences (Fig. 20.10) (61, 69). Strong homogeneous enhancement has been reported and may be the result of the presence of numerous proliferative capillaries in the collagenous stroma (Fig. 20.11).
Differential considerations for giant cell tumor of the tendon sheath include any soft tissue mass with low signal intensity on both T1- and T2-weighted images. This would include entities such as gouty tophus and desmoid tumor.
Extraskeletal Chondroma
Soft tissue (extraskeletal) chondroma is a rare benign tumor most commonly found in the hand, particularly on the volar side (70–72). Although the etiology is unclear, it has been proposed that it arises from the synovium of the tendon sheath (73). It consists of a well-defined nodule of cartilage that is unattached to bone, although it can cause compressive erosion (74). This lesion presents
as a slow-growing mass that may cause pain or tenderness. They are small, firm, and often mobile tumors on palpation (75).
as a slow-growing mass that may cause pain or tenderness. They are small, firm, and often mobile tumors on palpation (75).
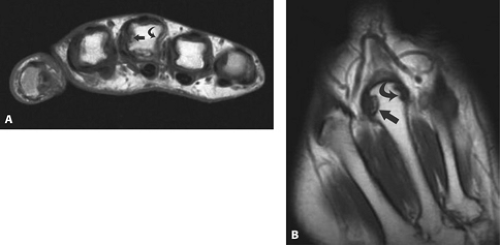
Calcification is seen in 33% to 70% of reported cases, sometimes with a characteristic ring-like cartilage appearance. As noted previously, extrinsic bone erosion may be seen. Although there is little literature regarding the MRI appearance, case reports describe nonspecific signal characteristics with intermediate signal intensity on T1-weighted images, high signal intensity on T2-weighted and inversion recovery sequences, and enhancement after the administration of intravenous contrast material (Fig. 20.12) (75, 76).
Masses and Mass-like Lesions in the Soft Tissues
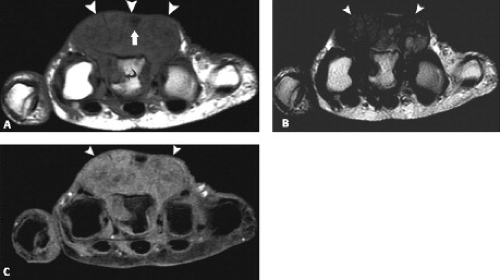
Lipoma Aborescens
Lipomas of the joint or tendon sheath are rare and manifest with two variants: a discrete solid fatty mass in the affected joint or tendon sheath or a “lipoma-like” lesion composed of hypertrophic synovial villi distended with fat called lipoma arborescence (77–79). The former is considered quite rare but has been described in the hand and wrist with less frequent involvement of the foot and ankle. Patients often present with a palpable mass that can cause mechanical dysfunction of the tendon and tendon sheath or mass effect on adjacent structures such as nerves or vessels (79). The imaging features are similar to those of a superficial or deep lipoma. MR images of these lesions reveal signal intensity that is isointense to fat regardless of pulse sequence (Fig. 20.13). No contrast enhancement is seen, except of the fibrous capsule. Lipomas can frequently demonstrate thin nonenhancing septae. Although septae have been shown to enhance in the minority of simple lipomata, this is considered to be a characteristic of well-differentiated liposarcomas (77, 80–82).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree