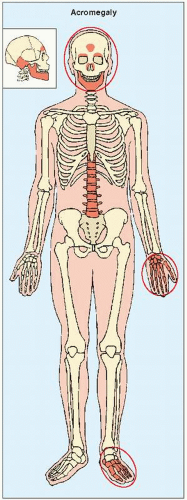
Increased secretion of growth hormone (somatotropin) by the eosinophilic cells of the anterior lobe of the pituitary gland, as a result of either hyperplasia of the gland or a tumor, leads to acceleration of bone growth. If this condition develops before skeletal maturity (i.e., while the growth plates are still open), then it results in gigantism; development after skeletal maturity results in acromegaly. The onset of symptoms is usually insidious, and the involvement of certain target sites in the skeleton is typical (
Fig. 30.4). Gradual enlargement of the hands and feet as well as exaggeration of facial features are the earliest manifestations. The characteristic facial changes result from overgrowth of the frontal sinuses, protrusion of the jaw (prognathism), accentuation of the orbital ridges, enlargement of the nose and lips, and thickening and coarsening of the soft tissues of the face.
Radiographic Evaluation
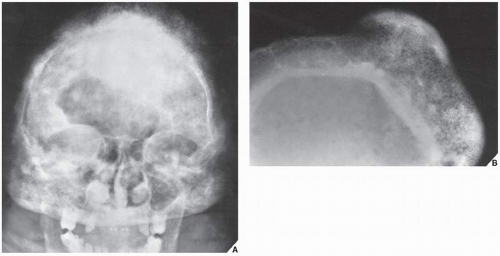
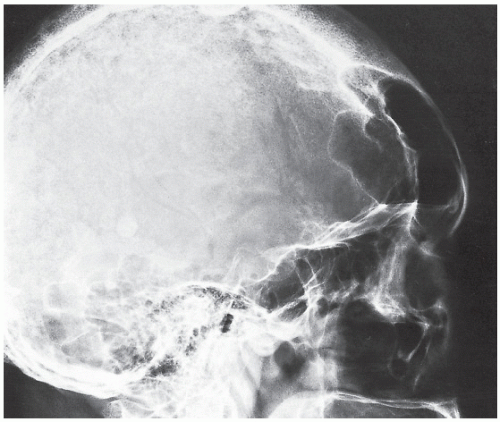
Radiographic examination reveals a number of characteristic features of this condition. A lateral radiograph of the skull demonstrates thickening of the cranial bones and increased density. The diploë may be obliterated. The sella turcica, which houses the pituitary gland, may or may not be enlarged. The paranasal sinuses become enlarged (
Fig. 30.5) and the mastoid cells become overpneumatized. The prognathous jaw, one of the obvious clinical features of this condition, is apparent on the lateral view of the facial bones.
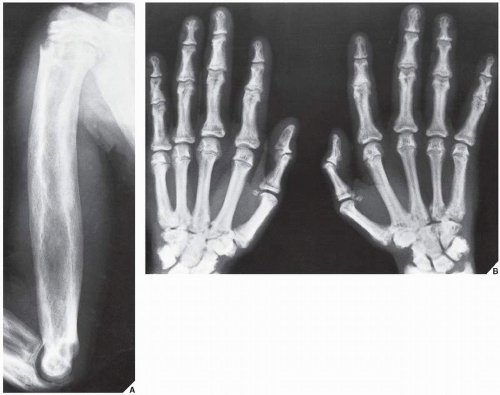
The hands also exhibit revealing radiographic changes. The heads of the metacarpals are enlarged, and irregular bony thickening along the margins, simulating osteophytes, may be seen. Increase in the size of the sesamoid at the metacarpophalangeal joint of the thumb may be helpful in evaluating acromegaly. Values of the sesamoid index (determined by the height and width of this ossicle measured in millimeters) greater than 30 in women and greater than 40 in men suggest acromegaly; however, generally the dividing line between normal and abnormal values is not sharp enough to allow individual borderline cases to be diagnosed on the basis of this index alone. Characteristic changes are also seen in the distal phalanges; their bases enlarge and the terminal tufts form spur-like projections. The joint spaces widen as a result of hypertrophy
of articular cartilage (
Fig. 30.6), and hypertrophy of the soft tissues may also occur, leading to the development of square, spade-shaped fingers.
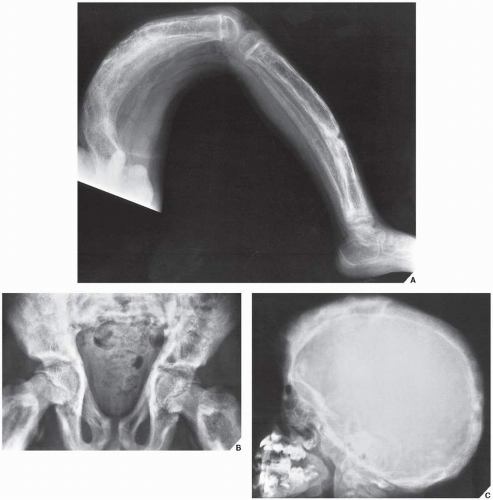
Evaluation of the foot on the lateral view allows an important measurement to be made, the heel-pad thickness. This index is determined by the distance from the posteroinferior surface of the os calcis to the nearest skin surface. In a normal 150-lb subject, the heel-pad thickness should not exceed 22 mm. For each additional 25 lb of body weight, 1 mm can be added to the basic value; thus, 24 mm would be the highest normal value for a 200-lb person. If the heel-pad thickness is greater than the established normal value, then acromegaly is a strong possibility (
Fig. 30.7), and determination of growth hormone level by immunoassay is called for.
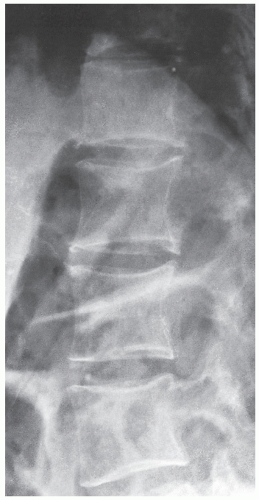
The spine in acromegaly may also reveal identifying features. A lateral radiograph of the spine may disclose an increase in the anteroposterior diameter of a vertebral body, as well as scalloping or increased concavity of the posterior vertebral margin (
Fig. 30.8). Although the exact mechanism of this phenomenon is not known, bone resorption has been implicated as a potential cause. Other conditions have also been associated with posterior vertebral scalloping (
Table 30.1). In addition, thoracic kyphosis is often increased in spinal acromegaly and lumbar lordosis is accentuated. The invertebral disk space may be wider than normal because of overgrowth of the cartilaginous portion of the disk.
The articular abnormalities seen in acromegaly are the result of a frequent complication, degenerative joint disease, which is in turn the result of overgrowth of the articular cartilage and subsequent inadequate nourishment of abnormally thick cartilage. The combination of joint space narrowing, osteophytes, subchondral sclerosis, and formation of cyst-like lesions is similar to the primary osteoarthritic process.