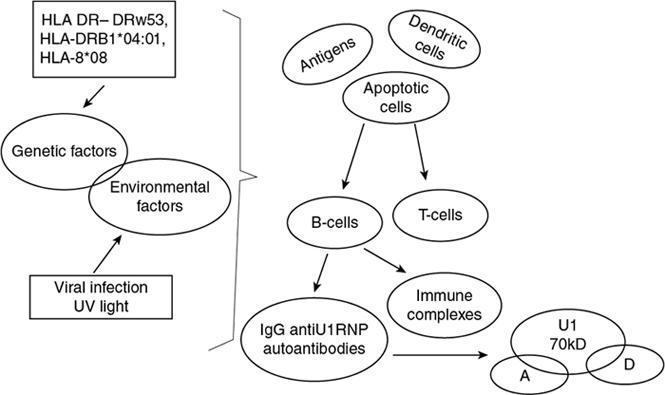
Jyoti Panwar Mixed connective tissue disease (MCTD) was first described in Sharp et al. (1972). It is characterized by an overlap of signs and symptoms of systemic lupus erythematosus (SLE), scleroderma and polymyositis-dermatomyositis, with antibodies against the U1-ribonucleoprotein (U1-RNP). Subsequently, it was found that these patients can also have manifestations of rheumatoid arthritis and showed an excellent response to glucocorticoid therapy with a favorable prognosis. Limited population studies show that the prevalence and incidence of MCTD are low. These few studies show a wide variation in the average age of onset between 38 and 48 years, with one study in the United States showing a significantly high incidence among women (84%), with an annual incidence rate of 1.9 per 100,000 individuals. In a study on Norwegian patients, the female/male ratio of 3.3 with an annual incidence of 2.1 per 1,000,000 individuals. The aetiology of mixed connective tissue disease is unknown, and the development of the disease is probably linked to interaction of genetic and environmental factors. The major histocompatibility complex (HLA) genes are implicated in the genetic predisposition of the disease. Classically, the HLA-DR4 and HLA-DRw53 genes have been related to MCTD and anti-U1-RNP-70kD antibodies. Recent studies show a strong association with HLA-DRB1*04:01 and HLA B*08. Therefore, MCTD is genetically different from SLE, which is characterized by HLA-DR2 and HLA-DR3, HLA-DRB1, HLA-DRB1*0301 and HLA-DRB1*1501; scleroderma associated with HLA-DR5/11, HLA-DR3 and DR2 or HLA-DQA1*0501; or polymyositis which is associated with HLA-DR3, HLA-B*0801 and DRB1*0301. Thus, MCTD is a distinct entity within autoimmune rheumatic diseases and path mechanism as described in Fig. 2.2.1. Although mixed connective tissue disease is an overlap of SLE, scleroderma, polymyositis–dermatomyositis and rheumatoid arthritis, the overlap of these conditions typically occurs sequentially over time rather than simultaneously. In the early stage of the disease, patients may present with nonspecific symptoms such as fatigue, myalgia, arthralgia and Raynaud phenomenon. High antinuclear antibody (ANA) and high anti-U1-RNP antibodies are characteristics of MCTD. Positive rheumatoid factor may also be seen in few patients. The clinical features of MCTD are variable and include fever, fatigue, weight loss, myositis, lymphadenopathy, sclerodactyly, digital swelling, Raynaud’s phenomenon, dyspnoea, dysphagia, diarrhoea, skin rash and neuralgia. Joint abnormalities that are clinically detectable are common in MCTD. Any joint may be involved, but the small joints of the hands and feet and the wrist are commonly affected. Symptoms may begin with intermittent arthralgia, which may progress into arthritis. Subcutaneous and peritendinous rheumatoid nodules may be seen in the dorsum of the hands and forearms. Joint deformities similar to those seen in rheumatoid arthritis can be seen in MCTD. The bony involvement is well demonstrated on plain radiographs, and soft-tissue involvement of the ligaments, tendons and joint capsules can be well appreciated on MRI. Radiographic abnormalities characteristically involve the metacarpophalangeal joints and proximal interphalangeal joints (MCP and PIP), midcarpal and radiocarpal joints of the wrist and the metatarsophalangeal and interphalangeal joints of the feet. The abnormalities can be symmetrical or asymmetrical. Periarticular osteoporosis, which is seen in rheumatoid arthritis, is common. Diffuse narrowing of the joint space is seen; with osseous erosions similar to those of rheumatoid arthritis, erosions of this distal interphalangeal joints may also be seen in MCTD. Occasionally, severe destructive arthritis can be seen similar to psoriatic arthritis. Intraarticular bony ankylosis is seen in the chronic phase. Symmetric soft-tissue swelling can be seen surrounding the involved joints; with diffuse swelling of the hand, secondary to oedema can be seen. Joint subluxation is seen similar to that seen in rheumatoid arthritis and SLE. Features of scleroderma such as soft-tissue atrophy, soft-tissue calcification and acroosteolysis can be seen in up to between 25% and 75% of patients (Fig. 2.2.2). Osseous resorption leads to pencil-like deformity of the phalanges. Intraarticular calcifications, due to calcium hydroxyapatite crystal deposition, have also been observed in the wrists and hands. Radiographic changes in the other large joints such as the knee, elbow or hip may be seen infrequently, which may not be evident clinically. Periarticular osteoporosis and rarely calcification can be seen in these joints. The radiographic features of the various connective tissue diseases seen in MCTD are summarized in Table 2.2.1 and also shown in Figs 2.2.3 and 2.2.4.
2.2: Mixed connective tissue disease
Introduction
Etiopathogenesis
Imaging features
Musculoskeletal manifestations

Scleroderma-like Features
SLE-like Features
Rheumatoid Arthritis-like Features
Dermatomyositis-like Features
Soft-tissue atrophy
Deforming nonerosive arthritis
Symmetrical soft-tissue swelling
Soft-tissue calcification
Soft-tissue or capsular calcification
Osteonecrosis
Periarticular osteopenia
Acroosteolysis
Diffuse joint space narrowing and marginal bone erosions
DIP joint erosions
Soft-tissue rheumatoid nodules
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine