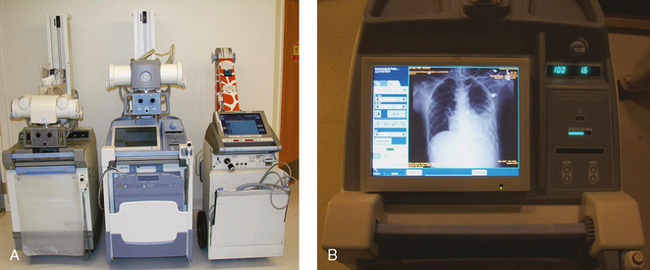
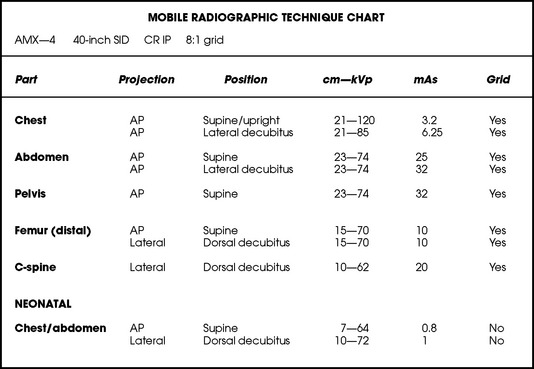
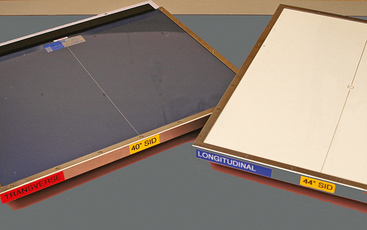
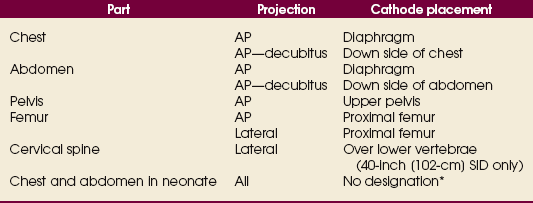
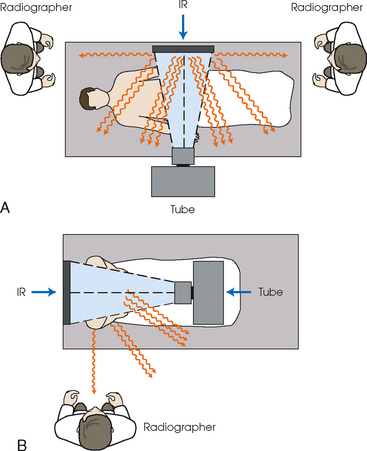
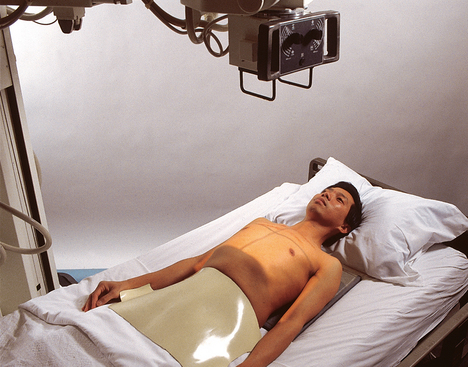
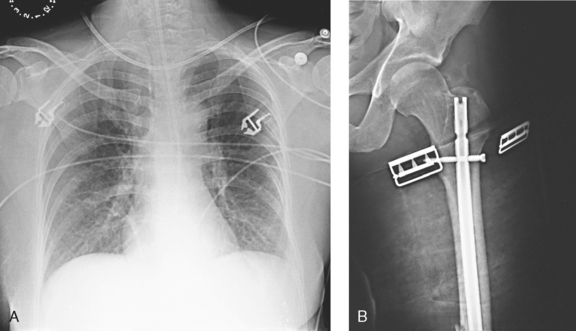
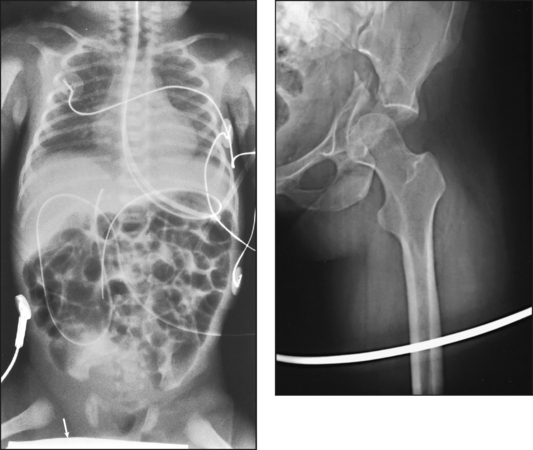
28 Mobile radiography using transportable radiographic equipment allows imaging services to be brought to the patient. In contrast to the large stationary machines found in radiographic rooms, compact mobile radiography units can produce diagnostic images in virtually any location (Fig. 28-1). Mobile radiography is commonly performed in patient rooms, emergency departments, intensive care units, surgery and recovery rooms, and nursery and neonatal units. Some machines are designed for transport by automobile or van to nursing homes, extended care facilities, or other off-site locations requiring radiographic imaging services. Some mobile units have direct digital capability, where the image is acquired immediately on the unit. These machines have a flat panel detector, similar to those found in a DR table Bucky. The detector either is connected to the portable unit by a tethered cord or communicates through wireless technology (Fig. 28-2). Mobile radiography presents the radiographer with challenges different from those associated with performing examinations with stationary equipment in the radiology department. Although the positioning of the patient and placement of the central ray are essentially the same, three important technical matters must be clearly understood to perform optimal mobile examinations: the grid, the anode heel effect, and the source–to–image receptor distance (SID). In addition, exposure technique charts must be available (see Fig. 28-5). For optimal imaging, a grid must be level, centered to the central ray, and correctly used at the recommended focal distance, or radius. When a grid is placed on an unstable surface such as the mattress of a bed, the weight of the patient can cause the grid to tilt “off-level.” If the grid tilts transversely while using a longitudinal grid, the central ray forms an angle across the long axis. Image density is lost as a result of grid “cutoff” (Fig. 28-3). If the grid tilts longitudinally, the central ray angles through the long axis. In this case, grid cutoff is avoided, but the image may be distorted or elongated. Grids used for mobile radiography are often of the focused type. Some radiology departments continue to use the older, parallel-type grids, however. All focused grids have a recommended focal range, or radius, that varies with the grid ratio. Projections taken at distances greater or less than the recommended focal range can produce cutoff in which image density is reduced on lateral margins. Grids with a lower ratio have a greater focal range, but they are less efficient for cleaning up scatter radiation. The radiographer must be aware of the exact focal range for the grid used. Most focused grids used for mobile radiography have a ratio of 6:1 or 8:1 and a focal range of about 36 to 44 inches (91 to 112 cm). This focal range allows mobile examinations to be performed efficiently. Inverting a focused grid causes a pronounced cutoff effect similar to that produced by improper distance. Today most grids are mounted on a protective frame, and the IR is easily inserted behind the grid (Fig. 28-4). A final concern regarding grids relates to the use of “tape-on” grids. If a grid is not mounted on an IR holder frame but instead is manually fastened to the surface of the IR with tape, care must be taken to ensure that the tube side of the grid faces the x-ray tube. The examinations described in this chapter present methods of ensuring proper grid and IR placement for projections that require a grid. Short SIDs and large field sizes are common in mobile radiography. In mobile radiography, the radiographer has control of the anode-cathode axis of the x-ray tube relative to the body part. Correct placement of the anode-cathode axis with regard to the anatomy is essential. When performing a mobile examination, the radiographer may not always be able to orient the anode-cathode axis of the tube to the desired position because of limited space and maneuverability in the room. For optimal mobile radiography, the anode and cathode sides of the x-ray tube should be clearly marked to indicate where the high-tension cables enter the x-ray tube, and the radiographer should use the heel effect maximally (Table 28-1). A radiographic technique chart should be available for use with every mobile machine. The chart should display, in an organized manner, the standardized technical factors for all the radiographic projections done with the machine (Fig. 28-5). A caliper should also be available; this device is used to measure the thickness of body parts to ensure that accurate and consistent exposure factors are used. Measuring the patient also allows the radiographer to determine the optimal kVp level for all exposures (Fig. 28-6). Radiation protection for the radiographer, others in the immediate area, and the patient is of paramount importance when mobile examinations are performed. Mobile radiography produces some of the highest occupational radiation exposures for radiographers. The radiographer should wear a lead apron and stand as far away from the patient, x-ray tube, and useful beam as the room and the exposure cable allow. The recommended minimal distance is 6 ft (2 m). For a horizontal (cross-table) x-ray beam or for an upright anteroposterior (AP) chest projection, the radiographer should stand at a right angle (90 degrees) to the primary beam and the object being radiographed. The least amount of scatter radiation occurs at this position (Fig. 28-7). Shielding and distance have a greater effect on exposure reduction, however, and should always be considered first. • X-ray examinations performed on children • X-ray examinations performed on patients of reproductive age • Any examination for which the patient requests protection • Examinations in which the gonads lie in or near the useful beam • Examinations in which shielding would not interfere with imaging of the anatomy that must be shown (Fig. 28-8) In addition, the source-to-skin distance (SSD) cannot be less than 12 inches (30 cm), in accordance with federal safety regulations.1 Before entering the patient’s room with the machine, the radiographer should follow several important steps (Box 28-1). The radiographer begins by checking that the correct patient is going to be examined. After confirming the identity of the patient, the radiographer enters, makes an introduction as a radiographer, and informs the patient about the x-ray examinations to be performed. While in the room, the radiographer observes any medical appliances, such as chest tube boxes, catheter bags, and intravenous (IV) poles, that may be positioned next to or hanging on the sides of the patient’s bed. The radiographer should ask family members or visitors to step out of the room until the examination is finished. If necessary, the nursing staff should be alerted that assistance is required. Patients who are in intensive care units or orthopedic beds because of fractures may be attached to various devices, wires, and tubing. These objects may be in the direct path of the x-ray beam and consequently produce artifacts on the image. Experienced radiographers know which of these objects can be moved out of the x-ray beam. When devices such as fracture frames cannot be moved, it may be necessary to angle the central ray or adjust the IR to obtain the best radiograph possible. In many instances, the objects have to be radiographed along with the body part (Fig. 28-9). The radiographer must exercise caution when handling any of these devices and should never remove traction devices without the assistance of a physician.
MOBILE RADIOGRAPHY
Principles of Mobile Radiography
Mobile X-Ray Machines
Technical Considerations
GRID
ANODE HEEL EFFECT
RADIOGRAPHIC TECHNIQUE CHARTS
Radiation Safety
Performing Mobile Examinations
PATIENT CONSIDERATIONS
Interfering devices