Approximately half of head and neck carcinomas arise from the oral cavity. Imaging plays an essential role in the preoperative evaluation of oral cavity carcinomas. MR imaging is particularly advantageous in the evaluation of the oral cavity, with better depiction of the anatomy in this region and reduction of dental artifacts compared with CT. MR is also the preferred imaging modality for the evaluation of bone marrow invasion and perineural tumor spread, which are findings critical for treatment planning. Advanced MR imaging techniques may potentially better delineate true tumor extent, determine lymph node metastases, and predict treatment response.
- •
Surgical resection with 1-cm tumor-free margins is the primary treatment for oral cavity carcinomas.
- •
Accurate preoperative planning is critical to achieve adequate surgical margins and thereby minimize the risk for tumor recurrence.
- •
MR imaging is particularly advantageous in the evaluation of the oral cavity, because it provides a better-detailed depiction of normal oral structures and has reduced dental artifact compared with CT.
- •
Placement of a rolled 2 × 2–in gauze adjacent to the tumor just before the MR examination separates the mucosal surfaces and significantly improves tumor delineation.
- •
Evaluation of tumor depth and size, bone invasion, lymph node metastases, and perineural tumor spread is essential for all oral cavity carcinomas.
Introduction
Head and neck carcinomas account for 5% of all cancers, with approximately half of those arising from the oral cavity. Globally, the annual estimated incidence for oral cavity cancers is approximately 275,000, with oral cavity carcinomas constituting up to 25% of all new cancers in high-risk countries, such as India and Pakistan. Squamous cell carcinomas (SCCs) account for more than 90% of oral cavity cancers, with the remainder of oral cavity malignancies including salivary gland tumors (mucoepidermoid carcinoma, adenoid cystic carcinoma, polymorphous low-grade adenocarcinoma, and adenocarcinoma not otherwise specified), lymphomas, metastases, melanomas, and sarcomas. These cancers are typically not distinguishable on imaging.
Oral cavity carcinomas most frequently occur in older men, although recently the incidence among young men and women has increased. Risk factors include tobacco and alcohol use, betel quid (most commonly in Asia), and a vitamin-poor diet. Sun exposure with ultraviolet radiation is a major risk factor for carcinomas of the lips. Human papilloma virus (HPV) infections have been implicated in a small percentage of oral cavity carcinomas, although not nearly to the same degree as with oropharyngeal carcinomas. HPV does not entirely account for the increasing incidence of oral cavity carcinomas in the younger population.
Oral cavity carcinomas present as white or red lesions involving the oral mucosa, occasionally with ulceration or exophytic components. Most patients with oral cavity carcinomas present with pain, which often limits oral function. Other clinical findings and symptoms include loose teeth, oral bleeding, dysarthria, dysphagia, and palpable lymphadenopathy. Most, if not all, oral cavity SCCs arise from premalignant oral cavity lesions including erythroplakia, leukoplakia, erythroleukoplakia and proliferative verrucous leukoplakia.
Surgical resection with 1-cm tumor-free margins is the primary treatment for oral cavity carcinomas. Close or positive surgical margins are strongly associated with poor prognosis and locoregional recurrence. Indications for adjuvant radiation therapy or chemoradiotherapy include advanced-stage tumors, positive or close surgical margins, perineural invasion, extensive bone invasion, and nodal metastases with extracapsular spread. Adjuvant radiation therapy, however, does not seem to improve local control rates in patients with positive surgical margins. Radiation therapy alone may be performed for patients who are not surgical candidates, although the recurrence rate is high for both the primary lesion and neck disease. Radiation therapy is also associated with significant morbidity, including osteoradionecrosis and speech and swallowing dysfunction.
The diagnosis of oral cavity cancer is typically known at imaging; the mucosal extent is best evaluated through visual inspection and manual palpation. Preoperative imaging is essential for tumor staging and appropriate treatment planning. Carefully performed and interpreted imaging can assist in determining the depth of invasion, involvement of critical structures, including bone and the internal carotid artery, and the presence of lymph node metastases. Clear surgical margins are a primary determinant of patient outcome; accurate preoperative planning is critical to achieve adequate surgical margins and thereby minimize the risk for tumor recurrence. An accurate assessment of the size of the cancer and the required resection volume also allows the surgical team to plan appropriately for reconstruction. MR imaging is particularly advantageous in evaluation of the oral cavity. MR imaging provides a better-detailed depiction of normal oral structures and has reduced dental artifact compared with CT. In addition, advanced MR imaging techniques, including spectroscopy, diffusion-weighted imaging, and perfusion imaging, are currently being investigated to better delineate true tumor extent, more accurately determine lymph node metastases, and predict treatment response.
Imaging anatomy
The oral cavity includes the lips, maxillary and mandibular gingiva, buccal mucosa, hard palate, anterior two-thirds of the tongue, floor of the mouth, and retromolar trigone. The vestibule is the space posterior and medial to the lips and cheek, respectively, and anterior and lateral to the gingiva and teeth. Posteriorly, the oral cavity is separated from the oropharynx by the circumvallate papillae, the anterior tonsillar pillars, and the junction of the hard and soft palates. The circumvallate papillae are easily identified on clinical examination but not delineated on imaging. The circumvallate papillae divide the tongue into the oral tongue, which lies in the oral cavity, and the base of tongue, which lies in the oropharynx.
The gingiva covers the buccal (outer) and lingual or palatal (inner) surfaces of the maxillary and mandibular alveolar ridges. The gingiva covering the buccal surfaces is continuous with the buccal mucosa lining the inner lips and cheeks at the gingivobuccal sulcus. The gingiva covering the lingual surface of the maxilla is continuous with the mucosa covering the hard palate. The hard palate forms the roof of the oral cavity and posteriorly attaches to the soft palate, which lies in the oropharynx. Coronal and sagittal T1-weighted images best depict the hypointense cortices and central hyperintense marrow of the osseous hard palate. A variable amount of T1 hyperintense submucosal fat can be seen along the inferior margin of the hard palate. A high concentration of minor salivary glands is present in the submucosal space of the hard palate and can occasionally be seen as small enhancing foci ( Fig. 1 F).
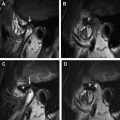
The floor of the mouth is a U-shaped space located inferior to the oral tongue and covered superiorly by squamous mucosa. The paired mylohyoid muscles provide the primary support for the floor of mouth, originating from the mylohyoid ridge along the inner surface of the mandible and attaching to a fibrous median raphe medially and to the hyoid bone posteriorly. On imaging, the mylohyoid muscles are best delineated in the coronal plane, forming a sling between the right and left inner margins of the mandible (see Fig. 1 A, B). In the axial plane, the muscles appear as linear structures, near-parallel and deep to the mandibular bodies; the mylohyoid muscles can also be readily identified in this plane, forming a “lollipop” configuration with the submandibular glands, with the “stick of the lollipop” formed by the mylohyoid muscle, and the “candy of the lollipop” formed by the submandibular gland (see Fig. 1 C). The paired geniohyoid muscles and anterior bellies of the digastric muscles provide additional support for the floor of mouth, located immediately superior and inferior to the mylohyoid muscle, respectively. These muscles are best depicted in the coronal plane (see Fig. 1 A).
The mylohyoid sling separates the sublingual space superiorly and medially from the submandibular space inferiorly and laterally. The posterior margin of the mylohyoid muscles is a free border that allows communication between the sublingual and submandibular spaces. The superficial portion of the submandibular gland lies within the submandibular space, with a small deep portion extending around the posterior margin of the mylohyoid muscle into the sublingual space. The duct of the submandibular gland courses anteriorly within the sublingual space and drains into the subfrenular region near midline (see Fig. 1 D). The sublingual space contains the deep portion of the submandibular gland, Wharton’s (submandibular) duct, sublingual gland, anterior portion of the hyoglossus muscle, hypoglossal and lingual nerves, and lingual artery and vein. The submandibular space is a predominantly fat-filled space that contains the superficial portion of the submandibular gland, anterior belly of the digastric muscle, facial artery and vein, and submandibular and submental nodes.
The oral tongue is composed of a midline fibrofatty lingual septum and four interdigitating intrinsic tongue muscles, including the superior longitudinal, inferior longitudinal, transverse, and vertical/oblique muscles. These intrinsic muscles cannot be distinguished from one another on imaging. There are also four paired extrinsic tongue muscles with origins external to the tongue, including the genioglossus, hyoglossus, styloglossus, and palatoglossus muscles. Involvement of these extrinsic muscles by carcinoma upstages the tumor to T4a. The genioglossus muscles arise from the genial tubercle along the inner surface of the mandible and superiorly interdigitate with the intrinsic tongue musculature. These muscles are easily identified on imaging as fan-shaped muscles forming the bulk of the tongue on sagittal T1-weighted images and as rectangular muscles on either side of the midline fatty lingual septum on coronal and axial images (see Fig. 1 A, C, E). The hyoglossus, styloglossus, and palatoglossus muscles are located laterally, with attachments to the hyoid bone, styloid process, and soft palate, respectively. The hyoglossus muscles are depicted in the coronal and axial planes as thin rectangular muscles parallel and medial to the mylohyoid muscles and lateral to the genioglossus muscles (see Fig. 1 B, C). Because the neurovascular bundles are closely related to the hyoglossus muscles, involvement of the hyoglossus muscle by tumor is a strong marker for neurovascular invasion.
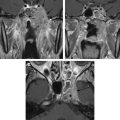
The retromolar trigone is a triangular area just posterior to the mandibular and maxillary third molars, immediately anterior to the mandibular ramus. The retromolar trigone lies immediately medial to the pterygomandibular raphe, which is a fascial band connecting the buccinator muscle anteriorly with the superior pharyngeal constrictor muscle posteriorly ( Fig. 2 ). Superiorly, the pterygomandibular raphe attaches to the hamulus of the medial pterygoid plate, and inferiorly, the raphe attaches to the mandibular body near the posterior margin of the mylohyoid ridge. The pterygomandibular raphe has been implicated in the route of tumor spread from the retromolar trigone.
Imaging anatomy
The oral cavity includes the lips, maxillary and mandibular gingiva, buccal mucosa, hard palate, anterior two-thirds of the tongue, floor of the mouth, and retromolar trigone. The vestibule is the space posterior and medial to the lips and cheek, respectively, and anterior and lateral to the gingiva and teeth. Posteriorly, the oral cavity is separated from the oropharynx by the circumvallate papillae, the anterior tonsillar pillars, and the junction of the hard and soft palates. The circumvallate papillae are easily identified on clinical examination but not delineated on imaging. The circumvallate papillae divide the tongue into the oral tongue, which lies in the oral cavity, and the base of tongue, which lies in the oropharynx.
The gingiva covers the buccal (outer) and lingual or palatal (inner) surfaces of the maxillary and mandibular alveolar ridges. The gingiva covering the buccal surfaces is continuous with the buccal mucosa lining the inner lips and cheeks at the gingivobuccal sulcus. The gingiva covering the lingual surface of the maxilla is continuous with the mucosa covering the hard palate. The hard palate forms the roof of the oral cavity and posteriorly attaches to the soft palate, which lies in the oropharynx. Coronal and sagittal T1-weighted images best depict the hypointense cortices and central hyperintense marrow of the osseous hard palate. A variable amount of T1 hyperintense submucosal fat can be seen along the inferior margin of the hard palate. A high concentration of minor salivary glands is present in the submucosal space of the hard palate and can occasionally be seen as small enhancing foci ( Fig. 1 F).
The floor of the mouth is a U-shaped space located inferior to the oral tongue and covered superiorly by squamous mucosa. The paired mylohyoid muscles provide the primary support for the floor of mouth, originating from the mylohyoid ridge along the inner surface of the mandible and attaching to a fibrous median raphe medially and to the hyoid bone posteriorly. On imaging, the mylohyoid muscles are best delineated in the coronal plane, forming a sling between the right and left inner margins of the mandible (see Fig. 1 A, B). In the axial plane, the muscles appear as linear structures, near-parallel and deep to the mandibular bodies; the mylohyoid muscles can also be readily identified in this plane, forming a “lollipop” configuration with the submandibular glands, with the “stick of the lollipop” formed by the mylohyoid muscle, and the “candy of the lollipop” formed by the submandibular gland (see Fig. 1 C). The paired geniohyoid muscles and anterior bellies of the digastric muscles provide additional support for the floor of mouth, located immediately superior and inferior to the mylohyoid muscle, respectively. These muscles are best depicted in the coronal plane (see Fig. 1 A).
The mylohyoid sling separates the sublingual space superiorly and medially from the submandibular space inferiorly and laterally. The posterior margin of the mylohyoid muscles is a free border that allows communication between the sublingual and submandibular spaces. The superficial portion of the submandibular gland lies within the submandibular space, with a small deep portion extending around the posterior margin of the mylohyoid muscle into the sublingual space. The duct of the submandibular gland courses anteriorly within the sublingual space and drains into the subfrenular region near midline (see Fig. 1 D). The sublingual space contains the deep portion of the submandibular gland, Wharton’s (submandibular) duct, sublingual gland, anterior portion of the hyoglossus muscle, hypoglossal and lingual nerves, and lingual artery and vein. The submandibular space is a predominantly fat-filled space that contains the superficial portion of the submandibular gland, anterior belly of the digastric muscle, facial artery and vein, and submandibular and submental nodes.
The oral tongue is composed of a midline fibrofatty lingual septum and four interdigitating intrinsic tongue muscles, including the superior longitudinal, inferior longitudinal, transverse, and vertical/oblique muscles. These intrinsic muscles cannot be distinguished from one another on imaging. There are also four paired extrinsic tongue muscles with origins external to the tongue, including the genioglossus, hyoglossus, styloglossus, and palatoglossus muscles. Involvement of these extrinsic muscles by carcinoma upstages the tumor to T4a. The genioglossus muscles arise from the genial tubercle along the inner surface of the mandible and superiorly interdigitate with the intrinsic tongue musculature. These muscles are easily identified on imaging as fan-shaped muscles forming the bulk of the tongue on sagittal T1-weighted images and as rectangular muscles on either side of the midline fatty lingual septum on coronal and axial images (see Fig. 1 A, C, E). The hyoglossus, styloglossus, and palatoglossus muscles are located laterally, with attachments to the hyoid bone, styloid process, and soft palate, respectively. The hyoglossus muscles are depicted in the coronal and axial planes as thin rectangular muscles parallel and medial to the mylohyoid muscles and lateral to the genioglossus muscles (see Fig. 1 B, C). Because the neurovascular bundles are closely related to the hyoglossus muscles, involvement of the hyoglossus muscle by tumor is a strong marker for neurovascular invasion.
The retromolar trigone is a triangular area just posterior to the mandibular and maxillary third molars, immediately anterior to the mandibular ramus. The retromolar trigone lies immediately medial to the pterygomandibular raphe, which is a fascial band connecting the buccinator muscle anteriorly with the superior pharyngeal constrictor muscle posteriorly ( Fig. 2 ). Superiorly, the pterygomandibular raphe attaches to the hamulus of the medial pterygoid plate, and inferiorly, the raphe attaches to the mandibular body near the posterior margin of the mylohyoid ridge. The pterygomandibular raphe has been implicated in the route of tumor spread from the retromolar trigone.
MR imaging
MR imaging provides superior soft tissue contrast and better depicts the detailed anatomy of the oral cavity compared with CT, and therefore can more accurately delineate the borders and extent of infiltration of oral cavity carcinomas. MR imaging also has the advantage of reduced metallic artifact from dental amalgam, which often hampers evaluation of the primary carcinoma with CT images. In addition, MR is the preferred imaging modality in the evaluation of perineural tumor spread and bone marrow invasion, which are important factors in treatment planning.
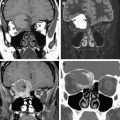
MR imaging should be performed with a dedicated neck coil and should include small field of view (FOV) images (14–18 cm) with thin sections (3–4 mm) dedicated to the oral cavity, and large FOV (20 cm) images of the entire neck to evaluate for nodal metastases ( Box 1 ). Small FOV images of the oral cavity should include thin-section axial and coronal T1-weighted images and axial and coronal thin-section postcontrast T1-weighted images, the latter with or without fat suppression. Fat suppression increases conspicuity of the enhancing tumor and enables distinction of tumor from the normal T1 hyperintense fat present throughout the oral cavity. However, fat saturation causes increased artifact from dental amalgam and soft tissue/air interfaces ( Fig. 3 C, D). Fat saturation also increases the time of acquisition, which may increase motion artifact. Frequency-selective fat-saturated T2-weighted images or short time inversion recovery (STIR) images should also be performed through the oral cavity and neck. At the authors’ institution, a coronal STIR sequence with a small FOV is obtained of the oral cavity, and an axial T2-weighted, frequency-selective fat-saturated sequence with a large FOV is obtained of the entire neck to evaluate for nodal metastases.
Placement of gauze adjacent to lesion, particularly helpful with buccal mucosal carcinomas
Small FOV of oral cavity: 14- to 18-cm FOV, 3- to 4-mm–thick slices
Large FOV of neck: 20-cm FOV, 4- to 5-mm–thick slices
- •
Large FOV, sagittal precontrast T1-weighted sequence
- •
Large FOV, axial T2-weighted fat-saturated or STIR sequence
- •
Small FOV, axial precontrast T1-weighted sequence
- •
(Small FOV, coronal precontrast T1-weighted sequence—optional)
- •
Small FOV, coronal T2-weighted fat-saturated or STIR sequence
Injection of intravenous contrast material
- •
Small FOV, axial postcontrast T1-weighted fat-saturated sequence
- •
Small FOV, coronal postcontrast T1-weighted fat-saturated sequence
- •
Large FOV, axial postcontrast T1-weighted fat-saturated sequence
Although MRI significantly reduces dental artifact compared with CT, extensive dental hardware may produce susceptibility artifact that can still obscure the primary tumor. Avoidance of gradient-echo (GRE), use of lower field strength magnets, reduction in echo train length (ETL) and echo time (TE), and increase in bandwidth are techniques that can minimize dental artifact ( Box 2 ). Frequency-selective fat saturation increases artifact from dental amalgam. As a result, a STIR sequence, which is not as affected by magnetic field inhomogeneities produced by metallic hardware, may be preferred over a frequency-selective fat-saturated T2-weighted sequence (see Fig. 3 C, E). In addition, postcontrast images without fat saturation in at least one plane may be helpful in patients with extensive dental work; although there is decreased conspicuity of the lesion without fat saturation, the gray signal of the enhancing tumor is typically distinguishable from the surrounding T1 hyperintense fat (see Fig. 3 D, F, G).
- •
Avoidance of GRE
- •
1.5T preferable to 3T
- •
Reduction of ETL and TE
- •
Increase in bandwidth
- •
Avoidance of frequency-selective fat-saturation techniques
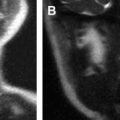
Because the structures within the oral cavity abut one another when imaged with the mouth closed, delineation of tumor depth may be problematic, particularly for evaluation of small mucosal tumors and tumors in certain locations, such as the gingiva and buccal mucosa. For CT examinations, the “puffed cheek” method of distending the cheeks has been successfully used, although the longer scanning times of MR imaging make it more difficult for the patient to maintain the same degree of distension throughout the examination. Placement of a rolled 2 × 2–in gauze adjacent to the tumor just before the MR examination has been shown to effectively separate the mucosal surfaces and significantly improve tumor delineation, with gauze having a similar appearance to air. This technique is particularly useful for the evaluation of buccal carcinomas (see Fig. 3 ; Fig. 4 ).