Cruciate ligament injuries, and in particular injuries of the anterior cruciate ligament (ACL), are the most commonly reconstructed ligamentous injuries of the knee. As such, accurate preoperative diagnosis is essential in optimal management of patients with cruciate ligament injuries. This article reviews the anatomy and biomechanics of the ACL and posterior cruciate ligament (PCL) and describes the magnetic resonance (MR) imaging appearances of complete and partial tears. Normal postoperative appearances of ACL and PCL reconstructions as well as MR imaging features of postoperative complications will also be reviewed.
Key points
- •
Magnetic resonance (MR) imaging is highly accurate in assessment of complete tears of cruciate ligaments.
- •
MR imaging is less accurate in assessment of chronic and partial tears of anterior cruciate ligament and posterior cruciate ligament.
- •
MR imaging is a useful technique in identifying causes of recurrent symptoms following cruciate ligament reconstruction.
Introduction
There are more than 200,000 anterior cruciate ligament (ACL) injuries annually in the United States. The incidence of posterior cruciate ligament (PCL) tears is considerably less common, accounting for 3% of all knee injuries in the general population.
A thorough understanding of ACL and PCL anatomy, injury patterns, and reconstructive techniques is a prerequisite to accurate MR interpretation of cruciate ligament injuries and postoperative appearances and these are covered in this article.
Introduction
There are more than 200,000 anterior cruciate ligament (ACL) injuries annually in the United States. The incidence of posterior cruciate ligament (PCL) tears is considerably less common, accounting for 3% of all knee injuries in the general population.
A thorough understanding of ACL and PCL anatomy, injury patterns, and reconstructive techniques is a prerequisite to accurate MR interpretation of cruciate ligament injuries and postoperative appearances and these are covered in this article.
Normal anatomy and function
ACL
The ACL is the major restraint to anterior translation of the tibia relative to the femur. It also provides restraint to rotatory load and contributes to the screw home mechanism of normal knee physiologic motion. The ACL arises from a semilunar region along the medial border of the lateral femoral condyle and inserts onto the proximal tibia, anterior to the tibial spines in close proximity to the anterior root of the lateral meniscus. It consists of 2 anatomically and functionally distinct bundles: the anteromedial (AMB) and posterolateral (PLB) bundles. An intermediate bundle has also been described in the literature.
- •
The AMB has a more proximal origin and is separated from the more distal origin of the PLB by the bifurcate ridge. The AMB inserts onto the tibia at a point anteromedial to the insertion of the PLB.
- •
The AMB and PLB parallel each other in the sagittal plane during knee extension but twist around each other during flexion.
- •
The 2 bundles have reciprocal tensioning characteristics. The AMB is maximally taut during knee flexion, and the PLB is maximally taut in extension and internal rotation.
- •
The AMB is the predominant restraint to anterior translation of the tibia during knee flexion and the PLB prevents anterior translation during knee extension as well as providing restraint against internal rotation of the tibia.
PCL
The PCL is the major restraint to posterior tibial translation, particularly during knee flexion. It consists of the ALB and PMB, functionally aided by the meniscofemoral ligaments.
- •
The stronger ALB arises anteriorly from the lateral margin of the medial femoral condyle, anterior to the origin of the PMB.
- •
The 2 bundles insert onto the posterior proximal tibia approximately 1 cm inferior to the articular surface.
- •
The ALB is maximally taut in flexion and the PMB is maximally taut during knee extension.
Imaging techniques and protocol
The exact MR imaging pulse sequences used to image the knee vary among different institutions. The pulse sequences at the authors’ institution are illustrated in Table 1 .
| Pulse Sequence | Plane | TR/TE | ETL | NEX | Matrix | FOV (cm) | Slice Thickness/Gap (mm) |
|---|---|---|---|---|---|---|---|
| Proton density | Sagittal oblique | 2100/14 | 6 | 2 | 288 × 256 | 14 | 4/0 |
| Fat-suppressed T2 | Sagittal oblique | 3900/75 | 8 | 2 | 256 × 224 | 14 | 4/0 |
| Intermediate-weighted | Coronal | 4900/34 | 8 | 1 | 512 × 256 | 14 | 4/0 |
| Fat-suppressed T2 | Axial | 3800/70 | 8 | 3 | 256 × 192 | 14 | 4/0 |
In addition to traditional orthogonal imaging, several oblique acquisitions have also been advocated in the literature for imaging of the ACL.
- •
Oblique sagittal images may be prescribed along an axis paralleling the lateral border of the lateral femoral condyle.
- •
Oblique coronal acquisitions, oriented along the longitudinal axis of the ACL or the roof of the intercondylar notch, may assist in depiction of the different components of the ACL and allow for complete visualization of the ACL.
- •
Oblique axial acquisitions obtained perpendicular to the long axis of the ACL have also been advocated particularly for evaluation of partial tears.
Three-dimensional (3D) isotropic fast spin-echo acquisitions producing high-quality multiplanar reformats in multiple oblique planes ( Fig. 1 ) may also be used to evaluate the cruciate ligaments and demonstrate similar diagnostic performance to standard orthogonal 2-dimensional (2D) acquisitions in evaluation of ACL and PCL tears.
Imaging findings
Normal Appearances
ACL
- •
In the sagittal plane, the normal ACL is taut and straight ( Fig. 2 A ). It runs parallel, or within 9°, to the roof of the intercondylar notch. On direct sagittal acquisitions, the entirety of the ACL may not be visualized on a single slice.
Fig. 2
Sagittal T2 fat-suppressed MR image ( A ) demonstrating a normal taut ACL with normal heterogeneity distally. Axial T2 fat-suppressed MR image ( B, C ) of the proximal and mid point of the normal ACL. Proximally ( B ), the ACL is elliptical and of low signal intensity ( arrowhead in B ). More distally ( C ), the 2 separate bundles are visualized with intervening normal increased signal intensity (AMB arrowhead , PLB arrow ). Coronal intermediate weighted MR image ( D ) demonstrating parts of a normal AMB ( arrowhead ) and PLB ( arrow ).
- •
On proximal axial images, the proximal ACL has an elongated elliptical appearance (see Fig. 2 B).
- •
The normal ACL is of low signal intensity proximally with a more heterogeneous appearance more distally as the ligament fans out toward its tibial attachment.
- •
The AMB and PLB may be distinguished on the axial and coronal planes (see Fig. 2 C, D).
PCL
- •
The PCL has a curved appearance with horizontal (proximal), genu, and vertical (distal) components.
- •
The PCL is of uniform low signal intensity on all pulse sequences ( Fig. 3 ). Slightly increased signal intensity may be visualized at the genu on short TE pulse sequences due to magic angle phenomenon.
Fig. 3
Sagittal T2 fat-suppressed MR imaging of the knee demonstrating the normal curved appearance of the PCL with the knee imaged in extension. The PCL is of homogeneous low signal intensity.
- •
Sagittal images demonstrate the PCL well throughout its entirety. Axial images are particularly well suited for visualization of the vertical component and the coronal images for visualization of the horizontal component.
ACL Tears
Mechanisms of injury
More than 80% of ACL tears occur because of noncontact injuries in sports, where deceleration, cutting, and pivoting are common.
- •
The most common mechanism of injury is the “pivot shift” injury in which a valgus and axial force is exerted on the flexed knee with concomitant quadriceps loading, anterior tibial translation, and external rotation of the femur.
- •
A varus force with internal rotation of the tibia can also produce an ACL tear and may be associated with a Segond fracture, an avulsion of the lateral rim of the tibia at the site of the attachment of the lateral capsular ligament ( Fig. 4 ).
Fig. 4
Coronal intermediate-weighted MR image ( A ) in a 21-year-old woman with an ACL tear ( arrowhead in A ) demonstrating a subtle undisplaced Segond fracture ( arrow ). Axial T2 fat-suppressed image ( B ) shows bone marrow edema at the site of the fracture ( arrow ), immediately posterior to the attachment of the iliotibial band ( arrowhead in B ).
- •
Hyperextension injuries may also result in ACL tears, often with associated PCL or the posterolateral corner injuries.
Depending on the mechanism of injury, associated injuries of the collateral ligaments, menisci, and articular cartilage may be present and impact the stability of the knee joint and the surgical management of patients. The mechanism of ligamentous injury can often be deduced from the bone marrow contusive patterns, aiding in identification of associated injuries.
MR imaging features of ACL injury
MR imaging is highly accurate in evaluation of ACL tears with an overall sensitivity of 83% to 95% and specificity of 95% to 100%. ACL injuries may involve the substance of the ACL, an avulsion of its tibial attachment ( Fig. 5 ), or a peel off lesion of its femoral attachment. Identification of the injury pattern impacts surgical management with intrasubstance ruptures treated by ligament reconstruction and acute osseous avulsions, or peel off lesions, treated by primary fixation.
Primary signs of ACL tear include the following :
- •
Focal discontinuity of the ACL ( Fig. 6 )
Fig. 6
Fat-suppressed T2-weighted sagittal image in a 46-year-old man a patient with an acute complete ACL tear demonstrating focal discontinuity of the mid ACL ( arrowhead ).
- •
Diffuse or focal abnormal signal intensity
- •
A mass-like appearance in the expected location of the ACL
- •
Abnormal orientation or bowing of the ACL
- •
Nonvisualization of the ACL ( Fig. 7 )
Fig. 7
Sagittal proton density MR image in a 38-year-old woman with a chronic ACL injury with nonvisualization of the ACL.
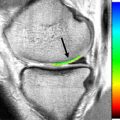
Focal discontinuity and diffuse increased signal intensity with enlargement of the ACL are among the most common patterns of ACL injury seen on MR imaging. Discontinuity is best appreciated on sagittal and axial images. Thickening and increased signal intensity of the ACL may also be encountered with mucoid degeneration of the ligament, but this often has a striated appearance with intact contiguous ligament fibers visible along its entire length ( Fig. 8 ). A horizontally oriented distal ACL, a vertically oriented proximal ACL, and discontinuity of the ACL have a positive predictive value of 100% for an ACL tear. An angle of greater than 15° between the roof of the intercondylar notch and the ACL or an angle of less than 45° between the distal ACL and the tibia, reflecting horizontal orientation of ACL fibers, are both highly accurate MR imaging findings of complete tears of the ACL. Distal fibers of a torn ACL may flip anteriorly, resulting in mechanical symptoms of a locked knee ( Fig. 9 ).
Secondary signs of ACL injury include ( Fig. 10 ) the following.
Osseous injuries
Osseous injury involving the anterior/central aspect of the lateral femoral condyle and the posterior aspect of the lateral tibial plateau is seen with pivot shift injuries. Less commonly, contusive injury of the posterior aspect of the medial tibial plateau and medial femoral condyle may also be visualized. Osseous injury is often associated with meniscal injury in the same compartment and is associated with poorer functional outcome at 1 year.
Anterior translation of the tibia
On the midsagittal image through the lateral compartment of the knee, the posterior aspect of the lateral tibial plateau subluxates anteriorly by greater than 5 mm in relation to the posterior aspect of the lateral femoral condyle, with a sensitivity of 86% and specificity of 99% for a complete ACL tear.
Uncovering of the posterior horn of the lateral meniscus
Uncovering the posterior horn of the lateral meniscus reflects a posterior displacement of the posterior horn of the lateral meniscus in relation to the posterior aspect of the lateral tibial plateau. Displacement of greater than 3.5 mm has a sensitivity of 44% and a specificity of 94% in the diagnosis of ACL disruption.
Several other signs have also been described in the setting of an ACL tear, including the buckling of the PCL, reduced PCL angle, posterior PCL line, and the posterior femoral line. In general, secondary signs are highly specific for the presence of an ACL injury but are of limited sensitivity. Overall, primary signs are the most useful for determining the status of the ACL and the addition of secondary signs are of little added or independent value.
The accuracy of clinical examination and MR imaging evaluation may be diminished in the setting of chronic and partial ACL tears.
With chronic complete ACL tears, the ACL remnant may reattach and the true severity of the injury may not be appreciated. Patterns of ACL scarring include the following :
- •
End-to-end scarring of the torn ACL ( Fig. 11 )
Fig. 11
Sagittal proton density MR image ( A ) in a 32-year-old woman with a high-grade to complete midsubstance tear of the ACL 2 months after injury. There is focal discontinuity of the mid-ACL. Sagittal T2 fat-suppressed MR image ( B ) in the same patient 1 year later shows complete continuity of the ACL with mild deformity and bowing.
- •
Scarring of the ACL to the PCL ( Fig. 12 )
Fig. 12
Sagittal T2 fat-suppressed MR image in a 49-year-old man 4 months after knee injury shows scarring of the ACL to the genu of the PCL ( arrowhead ). The distal ACL fibers are horizontally oriented in keeping with a complete tear.
- •
Scarring of the ACL to the roof of the intercondylar notch
- •
Scarring of the distal remnant onto the anatomic origin of the ACL
Scarring onto the anatomic origin of the ACL, although the least common pattern, has the most significant effect with reduced laxity on clinical examination.
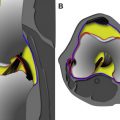
Partial ACL tears
Partial tears comprise up to 30% of all ACL tears. Partial injuries may consist of the following:
- •
Complete tear of the AMB with either a normal or a partially torn PLB. This pattern is the most common.
- •
Complete tear of the PLB with either a normal or a partially torn AMB ( Fig. 13 ).
Fig. 13
Sagittal isotropic fat-suppressed 3D SPACE acquisition ( A, B ) in a 33-old woman with a complete tear of the PLB of the ACL. There is focal discontinuity of the PLB ( arrowhead in A ). The AMB remains intact with mild signal changes and mild focal thickening consistent with a partial tear ( arrow in B ).
- •
Partial tears of both bundles.
Although the AMB is commonly injured with higher-energy trauma, the PLB may be injured with lower-energy rotational trauma. Clinically, complete tears of either the AMB or the PLB can be difficult to distinguish from an intact ACL and complete tears of one bundle with a partial tear of the other bundle may be mistaken for a complete tear. Accurate grading and diagnosis of a partial tear is of clinical significance because selective bundle reconstructions may be undertaken and risk of progression to ACL insufficiency is related to the grade of initial ligament injury sustained. With less than 25% of the ligament disrupted, there is a 12% risk of insufficiency as opposed to an 86% risk when greater than 75% of the ligament is injured.
Accuracy of MR imaging for identification of partial ACL tears is significantly diminished in comparison with complete tears, with sensitivities and specificities of 62% to 81% and 19% to 97%, respectively, and accuracy rates as low as 25% to 53%. 3T MR imaging has a sensitivity, specificity, and accuracy of 77%, 97%, and 95%, respectively. Diagnostic performance of axial oblique images, with a sensitivity and specificity of 87%, is better than orthogonal acquisitions, but this difference is not significant. Similarly, 3D isotropic acquisitions show no significant difference from standard 2D pulse sequences in the diagnosis of partial ACL injuries.
Signs that indicate partial tears include the following :
- •
Attenuation of the ACL
- •
Hyperintense intrasubstance signal with identification of intact fibers
- •
Posterior/inferior bowing of the ACL
- •
Distortion of the ACL without obvious discontinuity
Given that surgical treatment depends on the grade of injury, it is worthwhile to stratify ACL injuries as stable (normal ligament or stable partial tears) or unstable (unstable partial or complete tears) based on MR imaging ( Fig. 14 ). In one study using axial images, the visualization of a single bundle, an ill-defined mass-like appearance, and nonvisualization of the ACL had 100% sensitivity and 96% specificity for unstable tears. An elliptical ACL, attenuation of the ligament, and presence of isolated intrasubstance signal correlated with stable ACLs. Secondary signs of ACL insufficiency are more commonly seen with unstable tears, but these signs have a low sensitivity (specificity 100%, sensitivity 23%).