Abnormalities of the peripheral nervous, vascular, and immune systems contribute to the development of numerous foot and ankle pathologies in the diabetic population. Although radiographs remain the most practical first-line imaging tool, magnetic resonance (MR) is the tertiary imaging modality of choice, allowing for optimal assessment of bone and soft tissue abnormalities. MR allows for the accurate distinction between osteomyelitis/septic arthritis and neuropathic osteoarthropathy. Furthermore, it provides an excellent presurgical anatomic road map of involved tissues and devitalized skin to ensure successful limited amputations when required. Signal abnormality in the postoperative foot aids in the diagnosis of recurrent infection.
Key points
- •
Osteomyelitis occurs from direct inoculation in most cases, and identification of a skin defect should be the first step in evaluation of all diabetic feet.
- •
T2 hyperintensity and T1 hypointensity are required for the diagnosis of osteomyelitis. T2 hyperintensity on its own likely represents osseous stress response.
- •
Osteomyelitis tends to occur distal to the tarsometatarsal joints and in the malleoli and calcaneus.
- •
Neuropathic osteoarthropathy tends to be centered at the Lisfranc, Chopart, or metatarsophalangeal joints.
- •
Imaging findings suggestive of superimposed infection in neuropathic osteoarthropathy are ghosting of bones (indistinct on T1, but present on T2 or T1 postcontrast studies), disappearance of subchondral cysts, and greater-than-expected fluid collections.
Introduction/clinical presentation
Diabetic patients develop injury and progressive diseases of the foot from numerous sources, including disease of the peripheral nervous, vascular, and immune systems. There is frequently significant overlap between these issues, with one-third of all diabetic patients having a mixed neuropathic-ischemic foot ulcer. Sensory, motor, and autonomic nervous system problems arise in the setting of chronic hyperglycemia. Sensory neuropathy results in the inability to adapt to mechanical stresses with resultant soft tissue ulceration and articular structural disruption. Autonomic neuropathy deregulates perspiration, skin temperature, and arteriovenous shunting resulting in excessive callus formation and skin cracking. Motor neuropathy results in intrinsic muscle dysfunction or, less commonly, a single nerve defect, most frequently involving the common peroneal nerve. Diabetic patients have both large and small vessel ischemia. This ischemia is worsened by coexisting vascular risk factors, including smoking, hypertension, and hyperlipidemia. It is often refractory to revascularization of the larger vessels because of the extent of microvessel disease. Diabetes also inhibits the activity of polymorphonuclear leukocytes, reducing cellular immune responses. Collagen and keratin formation is also impaired. The primary role of imaging is to identify and delineate the sequelae of these systemic processes, including soft tissue infection, abscess formation, osteomyelitis, and the neuropathic joint. Prompt identification and accurate diagnosis are important for limb-sparing treatment planning.
Introduction/clinical presentation
Diabetic patients develop injury and progressive diseases of the foot from numerous sources, including disease of the peripheral nervous, vascular, and immune systems. There is frequently significant overlap between these issues, with one-third of all diabetic patients having a mixed neuropathic-ischemic foot ulcer. Sensory, motor, and autonomic nervous system problems arise in the setting of chronic hyperglycemia. Sensory neuropathy results in the inability to adapt to mechanical stresses with resultant soft tissue ulceration and articular structural disruption. Autonomic neuropathy deregulates perspiration, skin temperature, and arteriovenous shunting resulting in excessive callus formation and skin cracking. Motor neuropathy results in intrinsic muscle dysfunction or, less commonly, a single nerve defect, most frequently involving the common peroneal nerve. Diabetic patients have both large and small vessel ischemia. This ischemia is worsened by coexisting vascular risk factors, including smoking, hypertension, and hyperlipidemia. It is often refractory to revascularization of the larger vessels because of the extent of microvessel disease. Diabetes also inhibits the activity of polymorphonuclear leukocytes, reducing cellular immune responses. Collagen and keratin formation is also impaired. The primary role of imaging is to identify and delineate the sequelae of these systemic processes, including soft tissue infection, abscess formation, osteomyelitis, and the neuropathic joint. Prompt identification and accurate diagnosis are important for limb-sparing treatment planning.
Imaging the diabetic foot
The first-line examination of the diabetic foot is conventional radiographs, which should be performed in at least 3 planes and optimally 4. Relevant radiographic findings that should be observed include soft tissue swelling, radiopaque foreign bodies, cortical disruption/destruction, periostitis, joint incongruity, arterial calcification, and prior amputation. Radiographs can also be a beneficial adjunct in the evaluation of complex midfoot disruption. However, radiographs are insensitive to early osteomyelitis and notoriously underestimate the extent of osseous infection. Ultrasound may be used to evaluate soft tissue processes, such as abscess formation and tenosynovitis, and to locate radiolucent foreign bodies. However, this modality is limited in evaluating underlying bone and is also extremely user dependent. Triple phase bone scans that should be positive on all 3 phases (angiographic, blood pool, and delayed) in the setting of osteomyelitis are sensitive for osseous activity but not specific. Scintigraphic studies may be positive in other processes with high bone turnover, such as injury and neuropathic osteoarthropathy, and even osseous stress response. Labeled white blood cell scans have an increased sensitivity over bone scans; but the major limitation of nuclear medicine is the poor anatomic resolution, thus limiting the usefulness of these studies as a preoperative road map. MR imaging has emerged as the dominant imaging modality in the assessment of the diabetic foot, particularly the infected diabetic foot. It has high sensitivity (90%) and specificity (83%) for the diagnosis of osteomyelitis. Furthermore, it has the added benefit of providing good anatomic definition, allowing it to serve as an appropriate road map for surgical resection.
MR imaging scan protocols
The MR imaging examination should be tailored to the site of suspected abnormality. The authors divide the diabetic foot examination into either the ankle, including the ankle and hindfoot, or the foot, including the midfoot and forefoot. This designation allows for focused, smaller field-of-view imaging for the precise area of concern. Late-model multichannel ankle/foot receiver coils can provide high-resolution imaging from the ankle through the forefoot with a single acquisition, but prescription of imaging planes becomes difficult in this scenario. Most commercial payers still accept foot and ankle MR imaging examinations as distinct procedures; there are distinct Current Procedural Terminology codes: 73,718 and 73,720. The field of view for either examination can easily be tailored to the location of clinical concern.
As a standard protocol, with the use of dedicated extremity receiver coils, 2 sets of acquisitions are obtained in each plane. T1-weighted non–fat-suppressed imaging is performed in at least 2 planes to evaluate the bone marrow and the subcutaneous soft tissues. For these sequences, traditional spin echo is ideal; but multi-echo acquisitions with a short echo train are adequate. Fat suppressed, fast spin echo/turbo spin echo T2-weighted images are used to evaluate for edema and fluid signal. A short tau inversion recovery (STIR) sequence is recommended in at least one plane (generally sagittal) to mitigate potential near field homogeneity artifacts. Noncontrast examinations are almost always diagnostic; given the great frequency of renal disease in diabetic patients, contrast is rarely administered. When necessary and feasible, precontrast and postcontrast fat-suppressed, T1-weighted, fast gradient-echo sequences can be used to better delineate sinus tracts and abscess cavities and to identify devitalized/necrotic tissue. Dynamic contrast runs can be helpful in some cases, as the rate of enhancement can be measured and compared between normal tissues and devitalized tissues. To date, 1.5 T is still considered the imaging standard. Imaging at 3 T offers theoretic advantages, with shorter imaging times and/or higher resolution; but it is also prone to more artifacts and signal homogeneity issues.
MR imaging findings and diagnostic criteria in the diabetic foot
Soft Tissue Edema, Cellulitis
Skin thickening and edema (T1 hypointensity and T2 hyperintensity) are findings found in both soft tissue edema and cellulitis. Enhancement on postcontrast imaging is a characteristic feature of cellulitis. Furthermore, skin thickening and edema in the vicinity of soft tissue ulcer or abscess should raise suspicion of focal cellulitis rather than bland soft tissue edema.
Callus, Ulcer
Callus is a focal, masslike infiltration of the subcutaneous fat, seen as hypointense T1 and intermediate T2 signal. Callus enhances on T1-weighted postcontrast imaging. Typical locations for callus formation include beneath the first and fifth metatarsal heads and the distal phalanx of the hallux in the forefoot. In the midfoot, callus forms deep to the cuboid in patients with rocker bottom deformities and at the heel in the hind foot. Chronic friction at the site of callus can lead to the formation of overlying adventitial bursitis, which appears as a thin, linear, T2 fluid collection. Ulcers typically result from the breakdown of callus. Identifiable skin defects and heaped margins will allow differentiation of these two entities ( Fig. 1 ). Unlike callus, ulcers are T2 hyperintense. This high T2 signal is secondary to granulation tissue at the base and margins of the lesion. Ulcers also enhance after contrast administration.
Sinus Tract, Abscess
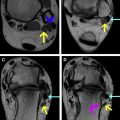
Sinus tracts are tubular or fissurelike conduits extending directly from the skin into the underlying soft tissues, or even into bone, allowing for spread of infection. These tracts may extend to any structure, even articular surfaces and joint spaces, resulting in osteomyelitis or septic arthritis. Identification of sinus tracts is essential. They can be observed on noncontrast fluid sensitive sequences but are more easily visualized on contrast-enhanced imaging as an enhancing connection between skin ulceration and soft tissue abscesses or infiltrated bone. Sinus tracts should be assessed in all 3 planes to accurately map out their full extent. Abscesses will be identified as pockets of fluid (areas of increased T2 signal) on fluid-sensitive imaging ( Fig. 2 ). Smaller abscesses may be difficult to identify without the aid of contrast. Linear peripheral contrast enhancement along the wall of the fluid collection is diagnostic of an abscess. Accurate delineation of all abscesses is a necessity before any surgical intervention.
Foreign Bodies
Barefoot walking in the presence of sensory neuropathy predisposes diabetic patients to the risk of plantar soft tissue injury and retained foreign bodies. These bodies will incite a local tissue response and can also act as vectors for the introduction of infection. Plain radiographs and particularly sonography are long established as sensitive diagnostic investigations in the evaluation of foreign bodies. MR imaging is generally less useful for detecting foreign bodies. The magnetic resonance (MR) appearance depends on foreign body composition. Foreign bodies often have low T1 and T2 signal and may be difficult to distinguish from surrounding soft tissues. Metal, air, and some forms of plastic and glass will be visible because of accompanying blooming artifact on gradient echo sequences. Surrounding enhancing tissue should be interpreted as reactive local tissue response/granulation tissue. If there is adjacent high T2 signal with an enhancing rim, an abscess can be documented; but it is important to distinguish between reactive soft tissue and adjacent abscess formation.
Muscle Denervation
MR imaging is exquisitely sensitive for muscle atrophy. Early muscle denervation from peripheral neuropathy is seen as high signal T2 linear streaks and patchy T1 hyperintensity in the intrinsic musculature of the forefoot, either diffusely or along neurotomal distribution. With advanced disease, there is fatty atrophy of these muscles. The muscle fibers become completely replaced by fat, appearing as bright signal on both T1 and T2 sequences and low signal on fat-suppressed imaging ( Fig. 3 ). Diabetic vasculopathy most frequently leads to the diffuse pattern of forefoot muscle atrophy, in contrast to posttraumatic and impingement processes that are more often neurotomal, along distributions of the medial or lateral plantar nerves. Forefoot muscle atrophy is associated with neuropathic arthropathies in the foot and, even at a preclinical stage, should be observed on MR imaging.
Necrotizing Fasciitis, Pyomyositis, Gangrene
Necrotizing fasciitis is a rapidly progressive medical emergency with mortality rates reported as high as 70% to 80%. Usually a polymicrobial infection, it starts in the superficial fascia extending to the deep fascia, resulting in necrosis by microvascular occlusion. MR imaging will demonstrate circumferential dermal and soft tissue thickening with smooth or fusiform thickening of the superficial and deep fascia. In advanced cases, fluid collections and gas formation occurs in the fascial planes. Gas bubbles appear as signal voids on all conventional sequences. If gas is suspected, but not visualized on conventional sequences, gradient sequences can be added to identify subtle areas of blooming artifact. The muscle immediately adjacent the fascia may ultimately become necrotic and demonstrate reduced enhancement when compared with the adjacent fascia. Although MR imaging is usually superior to computed tomography (CT) for demonstrating the extent of the infection, CT is often preferred when necrotizing fasciitis is suspected as the CT examination can be completed more rapidly, thus, facilitating urgent treatment. Air bubbles may also be more readily appreciated on CT.
The formation of ring-enhancing abscesses in muscle is a characteristic of pyomyositis and is less common in necrotizing fasciitis. Pyomyositis typically involves one muscle; however, in up to 40% of cases, multiple sites can be involved. Furthermore, thick irregular contrast enhancement of the deep fascia is more commonly seen in pyomyositis, compared with the smooth thickening of necrotizing fasciitis. The findings of early necrotizing fasciitis are not specific, and careful clinical correlation is required.
Diabetic myonecrosis or muscle infarction is not generally a diagnostic consideration in the foot, occurring more commonly in the thigh and calf. Diabetic myonecrosis displays nonspecific MR findings of inflammation interspersed with necrotic foci.
Gangrene results from tissue ischemia and can be described as either dry (noninfected) or wet (superinfected). Soft tissue devascularization will be identified as nonenhancing regions on postcontrast imaging. The margins of these regions may enhance secondary to reactive hyperemia. In areas of wet gangrene, marginal abscesses or foci of air may be evident in the adjacent tissues.
Tenosynovitis
Tendons in the foot and ankle are separated from the skin by minimal overlying soft tissue and are intimately related to the bones below. Direct extension of ulceration can lead to involvement of the tendon. The forefoot flexor, peroneal and Achilles tendons are most commonly involved ( Fig. 4 ). Tendon thickening, T2 hyperintensity, and enhancement on postcontrast imaging may indicate septic tenosynovitis; however, these findings are not specific and can be seen in a variety of pathologies, most notably in inflammatory arthropathies or after trauma. It is important to evaluate the entirety of the involved tendon. This evaluation is particularly important for flexor hallucis longus, evaluating for extension to the flexor digitorum longus at the intersection of both tendons (knot of Henry).