MR angiography is a flexible imaging technique enabling morphologic assessment of mesenteric arterial and venous vasculature. Conventional gadolinium-based contrast media and ferumoxytol are used as contrast agents. Ferumoxytol, an intravenous iron replacement therapy approved by the US Food and Drug Administration for iron deficiency anemia, is an effective and well tolerated blood pool contrast agent. The addition of 4D flow MR imaging enables a functional assessment of the arterial and venous vasculature; when coupled with a meal challenge, the severity of mesenteric arterial stenosis is well appreciated. Noncontrast MR angiographic techniques are useful for evaluating suspected mesenteric ischemia.
Key points
- •
MR angiography is a flexible technique enabling assessment of the arterial and venous vasculature of the abdomen in a single examination.
- •
MR angiography of the abdomen can be performed using gadolinium-based contrast media or ferumoxytol as a blood pool contrast agent.
- •
Noncontrast MR angiographic techniques are mature, available across vendor platforms, and enable depiction of the mesenteric arterial vasculature.
- •
4D flow MR imaging can be performed simultaneously with MR angiography, adding functional evaluation to the anatomic visualization.
- •
Common and rare causes of mesenteric ischemia, including atherosclerosis, noninflammatory vasculopathies, vasculitis, dissection, arterial embolization, and mesenteric venous thrombosis are well depicted at MR angiography.
Introduction
Vascular MR techniques are well suited to evaluate for suspected mesenteric ischemia or to further characterize severity of aortic or mesenteric venous disease leading to mesenteric ischemia. MR techniques useful for this evaluation include contrast-enhanced MR angiography (MRA), phase-contrast imaging, including four-dimensional (4D) flow MR imaging, pseudo–steady-state imaging, noncontrast MR angiographic techniques, and vessel well imaging. MR has advantages over computed tomographic (CT) methods due to the insensitivity of the method for artifacts related to vascular calcifications, the intravascular T1 shortening achievable with lower amounts of administered contrast, flexibility to image the blood vessels in multiple phases of respiration, the ability to simultaneously evaluate the abdominal venous vasculature, and the lack of ionizing radiation. Disadvantages compared with CT include a longer examination time and artifact from ferromagnetic devices in the field of view, including stainless steel endografts and stents, surgical clips, and embolization coils. This review article describes MR techniques of relevance and discusses their role in the assessment of the mesenteric vasculature in patients with suspected mesenteric ischemia.
MR angiographic techniques
First-Pass MR Angiography
First-pass MRA is a conventional angiographic technique enabling multiphase imaging of the abdominal arterial and venous vasculature. Contrast is administered intravenously followed by a saline flush and the first imaging acquisition is initiated to align acquisition of the central lines of k-space with peak contrast arrival in the abdominal aorta and abdominal aortic branches ( Fig. 1 ). This first phase is typically performed with k-space sampling methods that focus on filling the central lines of k-space first, followed by the peripheral lines after peak arterial enhancement in the vascular territory of interest. MR angiographic techniques rely on the paramagnetic effect of gadolinium with T1 shortening. Using a spoiled gradient recalled echo imaging technique with a short repetition time (TR) increases the conspicuity of the vascular territory of interest. Mask subtraction additionally suppresses unenhanced background tissue improving the signal-to-noise ratio of the vasculature over perivascular fat.

First-pass MR angiographic techniques can be extended to multiple acquisitions, with continued use of the mask subtraction technique for visualization of the late arterial, early venous, and late venous phases of enhancement. These subsequent acquisitions are obtained using a sequential k-space ordering schema as the imaging is obtained after the pass of the peak arterial bolus or during the bolus tail.
First-pass MRA can be obtained with or without electrocardiographic (ECG) gating. ECG gating is necessary to freeze pulsatile motion in the mid-ascending aorta and aortic root, but is not necessary for assessing the arch, descending thoracic aorta, or abdominal aorta. ECG gating for abdominal aortic applications is helpful when imaging structures that change in configuration over the cardiac cycle, such as dissection flaps, pseudoaneurysms, luminal thrombus, or complex atheromas.
Time-Resolved MR Angiography
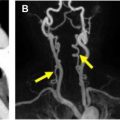
TR-MRA is an extension of the first-pass MR angiographic technique to enable highly accelerated imaging. , Although vendors have used different solutions to achieve TR-MRA imaging, the underlying principles are the same. Following complete sampling of the initial imaging volume or mask, the central lines of k-space are updated more frequently than the peripheral lines. All of the sampled k-space data are combined to enable a more frequent update of the entire k-space dataset than would be possible with accelerated methods and complete sampling of k-space alone. The addition of mask subtraction enables efficient review of these TR-MRA angiographic data ( Fig. 2 ). TR-MRA is helpful in identifying the contrast kinetics associated with atherosclerosis and dissection. In addition, the method is simple to perform and does not require careful timing of the onset of the acquisition with contrast arrival in the vascular territory of interest. TR-MRA is often used in conjunction with first-pass MR angiographic techniques as a method to calculate the transit time of contrast from a peripheral vein to the arterial territory of interest while obtaining useful information about vascular pathology.

Pseudo–Steady-State Imaging
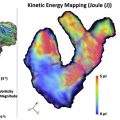
The gadolinium-based contrast media available on the market today are classified as extracellular, non-blood pool agents. Other than liver function agents, the gadolinium contrast media equilibrate into the interstitium and are excreted primarily via renal filtration with variable amounts of hepatic and enteric excretion. Despite formulation that does not optimize dwell time of gadolinium contrast media in the arterial and venous vasculature, vascular contrast concentration enabling effective imaging of the T1 shortening effect extends well beyond the second or third pass of gadolinium. So-called pseudo–steady-state imaging methods take advantage of this prolonged vascular dwell time as the contrast is being excreted, enabling imaging with both arterial and venous territories opacified ( Fig. 3 ). Pseudo–steady-state imaging can be performed with either spoiled gradient recalled echo imaging methods, T1-weighted imaging techniques using fat saturation to increase the conspicuity of the vasculature adjacent to fat, or other methods with inversion recovery-based fat suppression. Pseudo–steady-state imaging enables extension of a nonangiographic imaging examination to include a late-phase assessment of the arterial and venous vasculature in an anatomic region of interest. This approach works well with medium and larger vessels, where clear separation of the artery and accompanying vein(s) is possible. However, this approach is limited where smaller arterial branches are positioned adjacent to variably present paired veins, such as the distal branches of the mesenteric vasculature, along the portal triads, and at the visceral hila. Pseudo–steady-state imaging also precludes any assessment of contrast kinetics as the contrast media is completely dispersed throughout the arterial and venous vasculature. Imaging during the pseudo-steady state is useful to improve the conspicuity of the vasculature for 4D flow MR imaging, further increasing the contrast to noise ratio from perivascular fat and other tissue with short T1 values.

3D ECG-gated techniques with respiratory compensation methods have been developed and championed for pseudo–steady-state imaging. Respiratory compensation methods include respiratory bellows, respiratory navigators, and k-space reordering, with the central lines obtained at end-expiration and peripheral lines obtained at other less consistent portions of the cardiac cycle. Contrast medium in the pseudo-steady state is helpful with these methods as the intravascular T1 shortening effect can be used to take advantage of inversion recovery-based techniques to improve the conspicuity of the vasculature relative to perivascular fat. These techniques use spoiled gradient recalled echo or balanced steady-state free precession methods. Spoiled gradient recalled echo imaging has inherently less signal but is more resistant to off-resonance effects and susceptibility artifacts, useful for applications in the abdomen with air-filled bowel loops.
Steady-State Imaging with Ferumoxytol
Ferumoxytol (Feraheme, AG Pharmaceuticals) is an iron supplement Food and Drug Administration (FDA) approved for iron deficiency anemia. Ferumoxytol is an ultrasmall paramagnetic iron oxide with a dextran-derivative coating enveloping the Fe particle core resulting in a particle diameter of approximately 30 nm. The agent is slowly removed from the blood stream by the reticuloendothelial system with a half-life of approximately 14 hours. The long persistence in the blood stream necessitates coordination of other MR imaging tests with ferumoxytol administration ; nonangiographic MR imaging should be delayed for 3 days after administration. In addition, ferumoxytol has an FDA black box warning noting the risk of anaphylactoid-type reactions in susceptible patients in whom the agent is administered undiluted at the rate initially recommended by the manufacturer. It is now well recognized that administration of undiluted ferumoxytol unnecessarily increases the risk of treatment-resistant hypotension. Slower administration of dilute ferumoxytol coupled with screening for a history of medication-associated hypotension, resting systolic blood pressure less than 100 mm Hg, and past intolerance of Fe-related medications, while providing both intravenous and oral hydration, has been proven to be safe in clinical practice. The FeraSafe MRI Multi-Center Registry, developed and maintained by investigators from the University of California, Los Angeles, has documented the safe administration of ferumoxytol to more than 500 patients.
Ferumoxytol is administered intravenously and has been shown to act as an effective blood pool contrast agent at 1.5 and 3 T ( Fig. 4 ). , Ferumoxytol has distinct benefits for MR angiographic and venographic imaging in patients with suspected mesenteric ischemia. Ferumoxytol is typically administered as a slow bolus outside of the magnet with in-room nurse monitoring and subsequent imaging in the steady state. This enables simultaneous high-resolution imaging of the arterial and venous vasculature. Spatial resolution achievable with ferumoxytol is not limited by the short dwell time of high contrast concentration in the arterial vasculature; rather the image quality is primarily limited by the patient’s breath-holding ability or respiratory navigator technique used. Ferumoxytol greatly facilitates 4D flow MR imaging by improving the image quality of the accompanying phase-contrast MR angiogram, streamlining data analysis by improving the vascular segmentation step. Simultaneous arterial and venous imaging with adequate spatial resolution to distinguish arteries and veins in close proximity optimizes table time in these patients. Venous and arterial causes of mesenteric ischemia can be assessed simultaneously. What is lost from the dynamic components of the typical MR angiographic study with arterial, late arterial, portal venous, and systemic venous phases can be captured with 4D flow MR imaging. Artifact from bowel motility can be reduced by administering glucagon IV.

In addition, a meal challenge with Ensure can be performed to simulate the physiologic stressors leading to intestinal angina without requiring additional intravenous contrast for imaging after the meal challenge. , The long half-life of ferumoxytol also enables postinterventional steady-state imaging without administering additional contrast media.
Noncontrast MR Angiographic Techniques
Noncontrast MR angiographic techniques have been developed for peripheral MRA, and modifications of these methods applied to the mesenteric vasculature. The primary impetus for development was concerns around nephrogenic systemic fibrosis and subsequently the low but unknown risk of gadolinium chelate accumulation in patients irrespective of renal insufficiency. With the availability of macrocyclic gadolinium-based contrast and Fe-based contrast media the clinical need for noncontrast MR angiographic techniques is less apparent. Although a comprehensive review of noncontrast MR angiographic methods is beyond the scope of this review, methods useful in the mesenteric arterial system include both bright blood relatively flow-insensitive and bright blood flow-sensitive imaging techniques.
Bright blood flow-insensitive methods
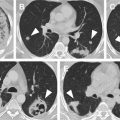
3D balanced steady-state free precession (bSSFP) described above as an imaging strategy for pseudo–steady-state imaging can also be used as a noncontrast MR angiographic technique ( Fig. 5 ). This technique is more commonly used in the chest for noncontrast coronary and thoracic aortic MRA. The relatively bright fat surrounding the vasculature compared with postcontrast techniques and susceptibility artifact from adjacent air-filled bowel loops can limit the overall image quality.

Quiescent interval single shot (QISS) is a robust technique with well-recognized accuracy in the evaluation of abdominal aortic, iliac, and lower extremity peripheral arterial disease. This approach suppresses signal from adjacent veins by using a tracking saturation pulse positioned toward the feet, an inversion pulse for static tissue, and a dedicated fat-suppression pulse. The resultant 2D axial images highlight the arterial signal. The principle limitation of this technique is the slice orientation and requirement for the blood vessel of interest to be orientated nearly orthogonal to the slice. Consequently, the superior mesenteric and inferior mesenteric arteries are well seen but the celiac axis is poorly assessed. When applied in the abdomen, concatenated breath-holds are used to cover the abdominal aorta and mesenteric branches ( Fig. 6 ).

Bright blood flow-sensitive methods
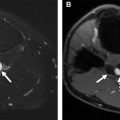
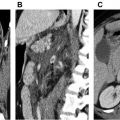
bSSFP inflow enhanced imaging overcomes the limitation of plane positioning described above with QISS. Implemented as a respiratory navigated 3D technique, the pulse sequence relies on saturating static tissue and venous inflow while highlighting fresh signal from arterial inflow into the volume to visualize the arterial vasculature. This approach is well suited to image the mesenteric arteries as well as the celiac axis and its branches ( Fig. 7 ). The inflow time can be lengthened in the presence of disease with reduced distal arterial flow. This method is, therefore, both anatomic and functional, similar to contrast-enhanced methods.